Functions
• Special sensory afferent (SA) for balance (via superior and inferior vestibular nerves) and hearing (via cochlear nerve).
Anatomy: Vestibular System
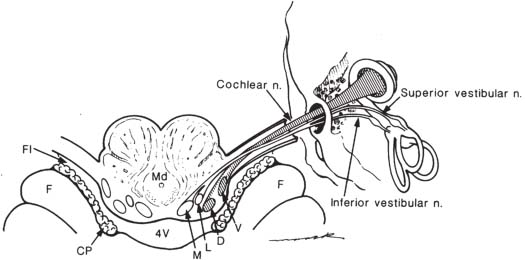
Vestibular Nerves (Figs. 8.1, 8.2)
• SA. Vestibular components of membranous labyrinth (three semicircular canals, utricle, and saccule) provide information to two vestibular nerves (superior and inferior vestibular nerves).
• The superior vestibular nerve (from utricle and superior and horizontal semicircular canals) and the inferior vestibular nerve (from inferior semicircular canal and saccule) connect with cell bodies in the vestibular ganglion (Scarpa ganglion), which lies near the fundus of the internal auditory canal.
• The vestibular nerves, joined by the cochlear nerve, form the vestibulocochlear nerve, which enters the pontomedullary junction near the lateral recess of the fourth ventricle. Whereas the cochlear fibers split dorsally to reach the cochlear nuclei, the vestibular fibers split ventrally to terminate in
1. Vestibular nuclei (superior, lateral, medial, and inferior) (see below) .
2. Cerebellum (flocculonodular lobe). The flocculonodular lobe functions with the semicircular canals to detect rapid changes in direction.
3. Reticular formation. The reticular formation is an area of interspersed small nuclei and fibers that spans the brainstem (see Appendix A, The Brainstem for more information).
• The vestibular system has three functions:
1. Provides information about movement of the head and changes in head position. This aids in coordinating the position of the eyes, head, and neck and in providing a sense of balance.
2. Increases tone in antigravity extensors to support the body against the pull of gravity.
3. Holds eyes on target while the head moves (vestibular impulses counter-roll the eyes against the direction of head movements to maintain fixation).
• Macula. Sensory organ of utricle and saccule. Contains hair cells with cilia embedded in gelatinous layer containing calcium carbonate otoliths. When the head moves in a given direction, otoliths move relatively in the opposite direction because they have more inertia than the surrounding fluid. The hair cells (each with 50–70 stereocilia and one large kinocilium) face in various directions, are stimulated by otolith movement thereby altering their firing rate, and synapse with the vestibular nerve.
• Based on their orientation, the utricle senses horizontal linear acceleration and the saccule senses vertical linear acceleration .
• The three semicircular canals (superior, posterior, and horizontal or lateral) are at right angles to one another and so detect motion in any combination of three planes (i.e., in any direction).
 Ampulla. Dilation at the end of each semicircular canal filled with endolymph. Contains crista ampullaris (sensory organ of semicircular canals), which has hair cells with cilia that project into the gel cup (cupula).
Ampulla. Dilation at the end of each semicircular canal filled with endolymph. Contains crista ampullaris (sensory organ of semicircular canals), which has hair cells with cilia that project into the gel cup (cupula).
 Cristae of semicircular canals detect angular acceleration because fluid in the ducts stays relatively still from inertia despite head rotation.
Cristae of semicircular canals detect angular acceleration because fluid in the ducts stays relatively still from inertia despite head rotation.
• Blood supply of membranous labyrinth is from the labyrinthine artery (also called internal auditory artery; usually a branch of the anterior inferior cerebellar artery [AICA], or less commonly of the basilar artery). Labyrinthine artery branches into (1) anterior vestibular artery, to superior and horizontal semicircular canals and utricle; (2) posterior vestibular artery, to posterior semicircular canal, saccule, and part of cochlea; and (3) cochlear artery.
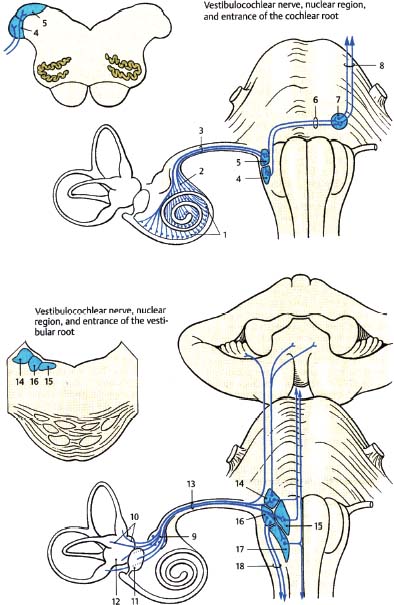
Fig. 8.1 Vestibulocochlear nerve: cochlear and vestibular roots. (1, spiral ganglion; 2, spiral tract; 3, cochlear root; 4, ventral cochlear nucleus; 5, dorsal cochlear nucleus; 6, trapezoid body; 7, trapezoid nuclei; 8, lateral lemniscus; 9, vestibular (Scarpa) ganglion; 10, semicircular ducts; 11, saccule; 12, utricle; 13, vestibular root; 14, superior vestibular nucleus; 15, medial vestibular nucleus; 16, lateral vestibular nucleus; 17, inferior vestibular nucleus; 18, vestibulospinal tract.)
Vestibular Sensory Organs (Figs. 8.3, 8.4)
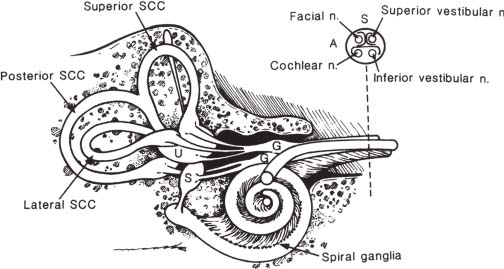
Fig. 8.3 Inner ear. Hearing-related structures include the cochlea, spiral ganglia, and cochlear nerve. Balance-related structures include the superior, posterior, lateral semicircular canals (SCC); utricle (U) and saccule (S); vestibular ganglion (G); and superior and inferior vestibular nerves. A cross-section of the apex of the IAC is shown at upper right. (A, anterior; S, superior.) (From Harnsberger HR. Handbook of Head and Neck Imaging (2nd ed.). St. Louis, MO: Mosby, 1995. Reprinted with permission.)
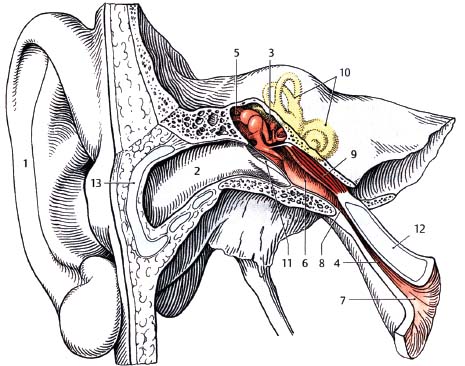
Fig. 8.4 View of the middle and inner ear. 1, auricle. 2, external acoustic meatus. 3, tympanic cavity. 4, auditory (Eustachian) tube. 5, epitympanic recess. 6, tympanic opening into auditory tube. 7, pharyngeal opening into auditory tube. 8, isthmus of auditory tube. 9, tensor tympani muscle. 10, bony labyrinth. 11, tympanic membrane. 12, auditory tube cartilage. 13, continuation of auricular cartilage.
Vestibular Nuclei (see also Appendix A)
• There are four vestibular nuclei:
1. Superior vestibular nucleus (of Bechterew)
2. Medial vestibular nucleus (of Schwalbe)
3. Lateral vestibular nucleus (of Deiters)
4. Inferior vestibular nucleus (of Roller)
• The vestibular nuclei straddle the pontomedullary junction and contain the cell bodies of the second-order neurons of the vestibular pathways.
• An interstitial nucleus of the vestibular nerve, located among the fibers of the vestibular root, has also been described, but its functional significance is unclear.
• Inputs to the vestibular nuclei include the following:
1. Vestibular portion of cranial nerve (CN) VIII (details below)
2. Cerebellovestibular tracts. The fastigial nucleus (a deep cerebellar nucleus) projects bilaterally to lateral and inferior vestibular nuclei. Uncrossed fastigial fibers project through the juxtarestiform body (a subdivision of the inferior cerebellar peduncle); crossed fastigial fibers project through the uncinate fasciculus of Russell, which travels along the superior cerebellar peduncle (see Appendix A).
3. Reticulovestibular tracts.
• Outputs from vestibular nuclei include the following:
1. Cerebellum (vestibulocerebellar pathways). Inferior and medial vestibular nuclei project via juxtarestiform body to ipsilateral cortex of flocculonodular lobe, uvula, and fastigial nucleus (vestibulocerebellum). This is a reciprocal connection for maintenance of posture.
2. Medial longitudinal fasciculus (MLF). All vestibular nuclei contribute to the MLF. Only the superior vestibular nucleus projects to the ipsilateral MLF; other nuclei send fibers to the contralateral MLF. The MLF interconnects the nuclei of CN III, IV, VI, the PPRF, the superior colliculus, and the interstitial nucleus of Cajal (a mesencephalic nucleus considered to be an important premotor center for eliciting vertical and rotatory eye and head movements) (see Appendix B).
3. Medial vestibulospinal tract. Medial vestibular nucleus to cervical and upper thoracic levels of contralateral spinal cord.
4. Lateral vestibulospinal tract. Lateral vestibular nucleus (Deiters’ nucleus) to ipsilateral lateral vestibulospinal tract to innervate antigravity extensors.
5. Reticular formation (vestibuloreticular pathways). Vestibuloreticular fibers mediate the nausea, vomiting, pallor, and hypotension that accompany vestibular disorders (e.g., motion sickness).
6. Vestibular hair cells for feedback control.
• Superior (Bechterew) and medial (Schwalbe) vestibular nuclei, Involved with eye reflexes (vestibuloocular reflexes) and coordination of eye movements with head movements. Receive afferent input from the semicircular canals and have efferent fibers to the MLF for eye movement and to the medial vestibulospinal tract for head and neck movement. The medial vestibular nucleus is the largest vestibular nucleus and sends crossed fibers to all nuclei involved with control of extraocular muscles and to the cerebellum. The superior vestibular nucleus sends uncrossed fibers by way of the MLF to the CN III and IV nuclei.
• Lateral vestibular nucleus (Deiters’ nucleus). Involved with posture. Afferent input is from the utricle (via the superior vestibular ganglion) and direct inhibitory input is from Purkinje cells in the cerebellar vermis. Efferent fibers to the lateral vestibulospinal tract serve to elicit lower limb extension for posture control.
• Inferior vestibular nucleus (of Roller), Integrates input from the vestibular system and the cerebellum. Afferent input from the saccule (from the inferior vestibular ganglion). Efferent fibers to the cerebellum and reticular formation.
Anatomy: Cochlear Nerve and Auditory Pathway (Figs. 8.1, 8.2)
• SA. Cochlear nerve fibers originate from the bipolar neurons of the spiral ganglion (Fig. 8.1). The peripheral processes terminate at the hair cells of the organ of Corti (see below), whereas the central processes (axons) combine in the fundus of the internal auditory canal (IAC) to form the cochlear nerve. The cochlear nerve then traverses the IAC, crosses the subarachnoid space, and enters the brainstem at the lateral recess of the fourth ventricle at the pontomedullary junction. Cochlear nerve fibers synapse in the ventral and dorsal cochlear nuclei, The organization is tonotopic, with high frequency dorsal and low frequency ventral. Auditory information is passed centrally via the lateral lemniscus to both inferior colliculi (though mainly contralateral). The inferior colliculus tonotopically projects to the medial geniculate body (MGB) of the thalamus. The MGB in turn gives rise to geniculotemporal fibers (auditory radiations) that travel to lamina IV of the primary auditory cortex (area 41) in the transverse temporal gyrus of Heschl (buried in the temporal operculum of the sylvian fissure) and to area 42 (auditory association cortex), which also surrounds and receives afferent fibers from area 41.
• Each cochlea projects bilaterally, but more so to the contralateral side.
• The ventral cochlear nucleus also sends fibers to the reticular formation and to the trapezoid body in the pons (see below) en route to the ipsi- and contralateral superior olivary complex (for sound localization; see below).
• There are four auditory commissures (white matter pathways crossing the midline):
1. The trapezoid body, located in the pontine tegmentum, connects the ventral cochlear nuclei to the lateral lemniscus and contralateral superior olivary nucleus. This is the only auditory commissure needed for sound localization.
2. The commissure of Probst connects the nuclei of the lateral lemniscus.
3. The inferior collicular commissure connects the inferior colliculi.
4. The commissure of Gudden (ventral supraoptic decussation) connects the medial geniculate bodies.
• Sound localization. Aided by the medial superior olivary (MSO) nucleus (detects time lag between ears) and lateral superior olivary (LSO) nucleus (detects sound intensity difference between ears). The superior olivary nuclear complex extends from the midpons through the rostral medulla (see Appendix A).
• Acoustic reflexes. Mediated by olivocochlear bundle from the superior olivary complex to (1) both motor CN VII nuclei to the stapedius muscles to decrease amplitude of sound waves by reducing ossicle movement; and (2) both motor CN V nuclei to the tensor tympani muscles to decrease sensitivity of tympanic membrane by pulling it taut. These pathways are activated during loud sounds to protect cochlea and during speech production to decrease hearing of one’s own speech.
Anatomy: Middle and Inner Ear (Fig. 8.4)
• Tympanic membrane (TM). Thin membrane that separates external ear from middle ear. It is attached to the malleus, which is attached to the incus, which is attached to the stapes, which lies against the oval window of the vestibule. The tympanic membrane is kept tense by the tensor tympani muscle (innervated by V3). The ossicles (malleus, incus, stapes) amplify the force of the sound wave that contacts the tympanic membrane.
• Cochlea , Consists of three side-by-side concentrically coiled tubes (scala vestibuli, scala media, scala tympani) that make 2.5 turns. Sound vibrations travel along the flexible Reissner’s membrane between the scala vestibuli and scala media. The basilar membrane, separating the scala media and scala tympani, is fibrous and is made up of 25,000 reed-like fibers extending from the bony center of the cochlea (modiolus); they are fixed at the modiolus and free at outer points to enable vibration. Near the base of the cochlea, the basilar membrane fibers are stiff and short and sensitive to high frequency; at the apex, they are sensitive to lower frequencies.
• Organ of Corti (spiral organ). Located on the surface of the basilar membrane; senses vibration. Consists of internal and external hair cells that synapse with dendrites of cochlear nerve endings. Cochlear nerve endings have cell bodies in the spiral ganglion in Rosenthal’s canal in the modiolus at the center of the cochlea. Axons from the spiral ganglion make up the cochlear nerve.
1. Stereocilia project from each hair cell onto gel of tectorial membrane in the scala media (cochlear duct). Bending one way causes hyperpolarization, the other way depolarization. The tectorial membrane is immobile, whereas the basilar membrane moves.
2. Depolarization. Occurs by increased K+ conductance into the stereocilia. The scala media contains endolymph, whereas the scala vestibuli and scala tympani contain perilymph that communicates with the cerebrospinal fluid (CSF) and with the perilymph of vestibular organs.
3. Endolymph. Secreted by the stria vascularis, has increased K+ and decreased Na+ compared with perilymph, creating endolymph potential (endocochlear potential).
• Sound interpretation involves place principle in which stimulation of different areas of the cochlea causes different nerves to fire and this determines frequency (pitch). Loudness is detected by increased amplitude, causing increased frequency of hair-cell firing and spatial summation. Humans are able to distinguish ~1 dB in sound intensity. Low-frequency sounds need higher intensity to be heard.
Vestibulocochlear Nerve: Normal Images (Figs. 8.5, 8.6, 8.7, 8.8, 8.9, 8.10, 8.11, 8.12, 8.13, 8.14)

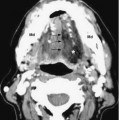
Fig. 8.5 A high-resolution axial CT image in bone window through the right internal auditory canal (*), cochlea (black straight arrowhead) and vestibule (v). Note the canals for the cochlear division (black straight arrow) and vestibular division (black concave arrow) of the CN VIII nerves; also note the horizontal semicircular canal (black concave arrowhead). Normal ossicles including the head of malleus (white straight arrow) and body of incus (white concave arrow) are seen within the middle ear cavity.
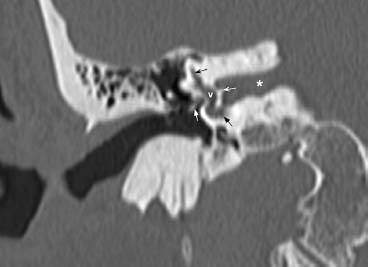
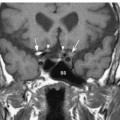
Fig. 8.6 A high-resolution coronal CT image in bone window at the level of the right internal auditory canal (*) shows the crista falciformis (white concave arrow) separating superior and inferior compartments of the lateral IAC. Vestibule (v) is indicated, as is a portion of the superior semicircular canal (black concave arrow) and cochlea (black straight arrow). The stapes (white straight arrow) is partially visualized extending into the oval window.
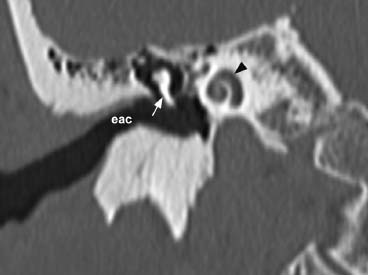
Fig. 8.7 More anteriorly, a high-resolution coronal CT image in bone window at the level of the external auditory canal (eac) shows the normal “snail-like” appearance of the right cochlea (arrowhead). The malleus (arrow) is seen within the middle ear.
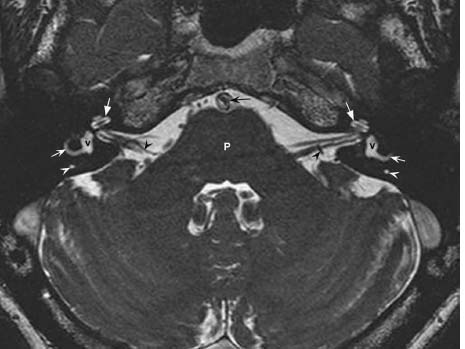
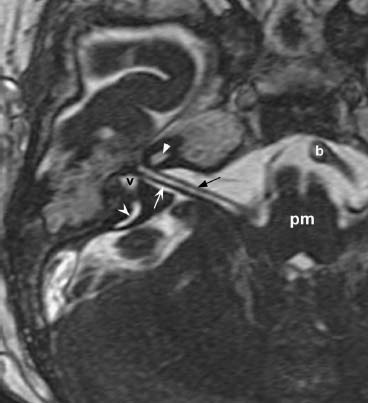
Fig. 8.9 An axial three-dimensional FIESTA image from a different patient at the level of the pontomedullary junction (pm) and through the upper aspect of the right internal auditory canal (IAC) demonstrates the course of the right CNs VII and VIII traversing the cerebellopontine angle and entering the IAC. CN VII (the facial nerve, black straight arrow) is seen anteriorly and the superior vestibular nerve (branch of CN VIII, white concave arrow) is seen posteriorly. The cochlea (straight arrowhead), vestibule (v), and posterior semicircular canal (concave arrowhead) are partially shown. Basilar artery flow void (b) is seen at its junction with the left vertebral artery.
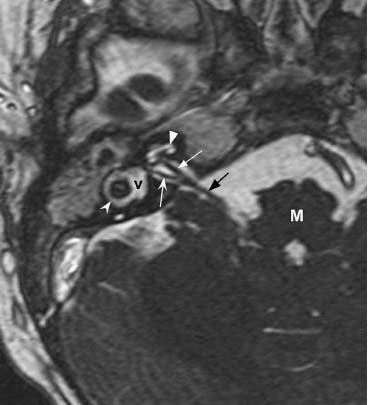
Fig. 8.10 More inferiorly, an axial three-dimensional FIESTA image in the same patient at the level of the upper medulla (M) and lower part of the right internal auditory canal (IAC) demonstrates the vestibulocochlear nerve (black arrow) branching into the more anterior cochlear nerve (white straight arrow) and the more posterior inferior vestibular nerve (white concave arrow). The cochlear branch is seen entering the cochlea (white straight arrowhead). The normal vestibule (v) and horizontal semicircular canal (white concave arrowhead) are demonstrated.
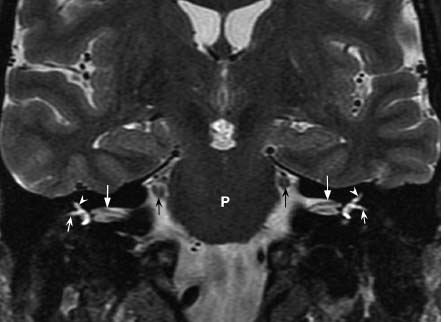
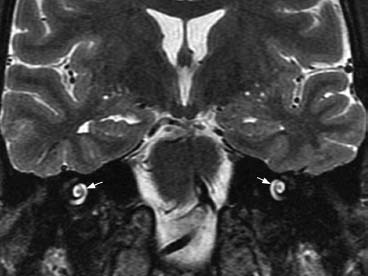
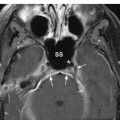
Fig. 8.12 More anteriorly, a coronal T2-weighted image shows fluid signal with the normal turns of the snail-like bilateral cochleae (arrows).
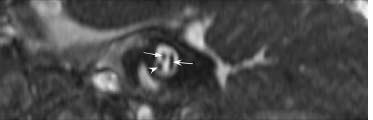
Fig. 8.13 A sagittal three-dimensional FIESTA image at the level of the mid internal auditory canal shows the facial nerve anterosuperiorly (straight arrow) and the cochlear nerve anteroinferiorly (concave arrowhead). More posteriorly, the branch point of the CN VIII superior and inferior vestibular nerves is seen (concave white arrow).
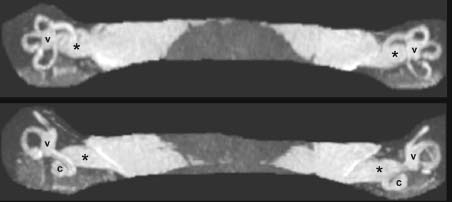
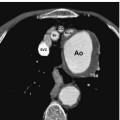
Fig. 8.14 Three-dimensional MIP (maximum intensity projection) an axial FIESTA images demonstrate the internal auditory canals (*) and also show the normal relationship of the cochleae (c), vestibules (v), and three semicircular canals in different projections.
Evaluation
• Patients with suspected vestibular dysfunction should have a detailed neurologic evaluation including a detailed CN examination, evaluation of hearing, examination of ocular movements, cerebellar testing, and evaluation of vestibular control of balance and movement.
• Romberg test is usually positive in unilateral vestibular dysfunction. A positive Romberg test is when a patient is unable to maintain balance while standing upright with feet together and eyes closed. The patient tends to fall to the side of vestibular hypofunction.
• Vestibular reflexes
 Decerebrate reflex (decerebrate rigidity). Described by Sherrington in 1896. Due to anatomical or functional transection of the brainstem above the vestibular nuclei but below the red nucleus. All four extremities become tonically extended. Arises from combined effects of tonic activity in vestibulospinal and pontine reticulospinal neurons (innervating extensors).
Decerebrate reflex (decerebrate rigidity). Described by Sherrington in 1896. Due to anatomical or functional transection of the brainstem above the vestibular nuclei but below the red nucleus. All four extremities become tonically extended. Arises from combined effects of tonic activity in vestibulospinal and pontine reticulospinal neurons (innervating extensors).
 Decorticate reflex (decorticate rigidity). When the brainstem is functionally lesioned above the red nucleus, posture is regulated by the rubrospinal tract, which opposes vestibulospinal and reticulospinal pathways. In humans, lower extremity (LE) extensors and upper extremity (UE) flexors contract steadily (because the rubrospinal tract in humans only projects as far as the cervical region and only counteracts vestibulospinal activity in UEs but not LEs).
Decorticate reflex (decorticate rigidity). When the brainstem is functionally lesioned above the red nucleus, posture is regulated by the rubrospinal tract, which opposes vestibulospinal and reticulospinal pathways. In humans, lower extremity (LE) extensors and upper extremity (UE) flexors contract steadily (because the rubrospinal tract in humans only projects as far as the cervical region and only counteracts vestibulospinal activity in UEs but not LEs).
 Vestibuloocular reflex (VOR). A reflex eye movement that keeps the visual image still during head movement by producing coordinated eye movements in the direction opposite to head movement. Head rotation causes motion in the membranous labyrinth and ipsilateral horizontal semicircular canal → increases activity in ipsilateral CN VIII → information conveyed to vestibular nuclei → reciprocal alteration in activity in brainstem nuclei that control ipsilateral and contralateral eye movements → compensatory movement of the eyes → stabilization of the visual image on the retina with head movement. The VOR is one of the fastest reflexes in the body, and eye movements lag head movements by < 10 milliseconds. In comatose patients, the VOR is tested as the oculocephalic reflex or “doll’s eye” reflex when the physician turns the head and examines compensatory eye movements. Absent oculocephalic reflexes indicate brainstem dysfunction.
Vestibuloocular reflex (VOR). A reflex eye movement that keeps the visual image still during head movement by producing coordinated eye movements in the direction opposite to head movement. Head rotation causes motion in the membranous labyrinth and ipsilateral horizontal semicircular canal → increases activity in ipsilateral CN VIII → information conveyed to vestibular nuclei → reciprocal alteration in activity in brainstem nuclei that control ipsilateral and contralateral eye movements → compensatory movement of the eyes → stabilization of the visual image on the retina with head movement. The VOR is one of the fastest reflexes in the body, and eye movements lag head movements by < 10 milliseconds. In comatose patients, the VOR is tested as the oculocephalic reflex or “doll’s eye” reflex when the physician turns the head and examines compensatory eye movements. Absent oculocephalic reflexes indicate brainstem dysfunction.
 Caloric testing (oculovestibular reflex), Useful largely for determining the presence/absence of brainstem function in comatose patients rather than for diagnosis of vestibular dysfunction. Cold water irrigation into the external ear canal causes a decrease in CN VIII firing rate in the ipsilateral utricle, which leads to nystagmus with the fast component away from the stimulus. The mnemonic “COWS” (cold—opposite, warm—same) refers to the direction of the fast component of nystagmus induced by water irrigation.
Caloric testing (oculovestibular reflex), Useful largely for determining the presence/absence of brainstem function in comatose patients rather than for diagnosis of vestibular dysfunction. Cold water irrigation into the external ear canal causes a decrease in CN VIII firing rate in the ipsilateral utricle, which leads to nystagmus with the fast component away from the stimulus. The mnemonic “COWS” (cold—opposite, warm—same) refers to the direction of the fast component of nystagmus induced by water irrigation.
Clinical Manifestations
• Nystagmus (oscillating eye movements)
• Oscillopsia (a sense of oscillation of objects viewed)
• Autonomic effects (nausea, vomiting, pallor, sweating, hypotension)
• Vertigo
 Vertigo is an illusory sensation of movement associated with disease of the labyrinth or its central connections (CN VIII, vestibular nuclei).
Vertigo is an illusory sensation of movement associated with disease of the labyrinth or its central connections (CN VIII, vestibular nuclei).
 Usually the movement is described as a “spinning” but can also be a “tilting.”
Usually the movement is described as a “spinning” but can also be a “tilting.”
 May be associated with nausea/vomiting (activation of medullary area postrema), pallor, sweating, nystagmus.
May be associated with nausea/vomiting (activation of medullary area postrema), pallor, sweating, nystagmus.
 Differentiate from faintness, lightheadedness, presyncope (caused by decreased cerebral blood flow), dysequilibrium (unsteadiness when walking), nonspecific dizziness.
Differentiate from faintness, lightheadedness, presyncope (caused by decreased cerebral blood flow), dysequilibrium (unsteadiness when walking), nonspecific dizziness.
 Categorized into central causes (dysfunction of vestibular connections), peripheral causes (vestibular labyrinthine disease), and systemic causes (other diseases/drugs/toxins).
Categorized into central causes (dysfunction of vestibular connections), peripheral causes (vestibular labyrinthine disease), and systemic causes (other diseases/drugs/toxins).
• Central causes of vertigo
 More likely to be chronic or permanent compared with peripheral vestibulopathies.
More likely to be chronic or permanent compared with peripheral vestibulopathies.
 Associated brainstem findings are more prominent, whereas auditory involvement is less frequent.
Associated brainstem findings are more prominent, whereas auditory involvement is less frequent.
 Vascular.
Vascular.
1. Transient ischemic attacks (TIAs). Vertebrobasilar ischemia is often accompanied by vertigo. It may be part of a subclavian steal syndrome (stenosis of subclavian artery proximal to the origin of the vertebral artery associated with flow reversal in the vertebral artery especially during arm exercise).
2. Wallenberg syndrome (lateral medullary syndrome). Caused by occlusion of the intracranial vertebral artery or PICA and leads to vertigo by ischemic injury to the vestibular nuclei. It is associated with some or all of the following findings: ipsilateral facial hypalgesia and thermoanesthesia, contralateral trunk and extremity hypalgesia and thermoanesthesia, ipsilateral vocal cord paralysis, dysphagia, dysarthria, ipsilateral Horner syndrome, nausea, vomiting, ipsilateral cerebellar signs/symptoms, diplopia, and hiccups. See also Case 9.1, Chapter 9 and Appendix A.
3. Basilar migraine (vertigo followed by suboccipital headache and vomiting).
4. Cerebellar infarction/hemorrhage (often accompanied by vertigo and ataxia).
 Inflammatory. Multiple sclerosis (MS) (~20% of patients with MS experience vertigo at some point).
Inflammatory. Multiple sclerosis (MS) (~20% of patients with MS experience vertigo at some point).
 Vestibular epilepsy (vertigo may be an aura for temporal lobe epilepsy).
Vestibular epilepsy (vertigo may be an aura for temporal lobe epilepsy).
• Peripheral causes of vertigo. Due to lesion of semicircular canals and/or otolith organs. Patient usually lies with affected ear uppermost, slow phase of nystagmus is toward lesion, and Romberg test is positive (falls toward lesion).
 The three most common peripheral causes of vertigo are benign paroxysmal positional vertigo, viral infection/inflammation, and Meniere disease.
The three most common peripheral causes of vertigo are benign paroxysmal positional vertigo, viral infection/inflammation, and Meniere disease.
 Benign paroxysmal positional vertigo (BPPV). Most common single cause of vertigo (~20% of all cases). Usually idiopathic but may be caused by trauma or other ear diseases. Generally considered to be caused by an abnormality of the posterior semicircular canal otoliths. After head tilt toward affected ear or after head extension, rotational vertigo and nystagmus occur. The Dix-Hallpike maneuver (also known as the Nylen-Barany maneuver) is the standard test for BPPV and involves moving the patient rapidly from a sitting to a supine position with the head turned 45 degrees to the right or left; after 20–30 seconds, the patient is returned to the sitting position. The finding of rotatory nystagmus with limited duration is considered pathognomonic. Treatments include conservative therapy, vestibulosuppressants (e.g., meclizine), and canalith repositioning procedures (e.g., Semont or Epley maneuvers). Surgery (e.g., posterior canal occlusion) is limited to intractable cases.
Benign paroxysmal positional vertigo (BPPV). Most common single cause of vertigo (~20% of all cases). Usually idiopathic but may be caused by trauma or other ear diseases. Generally considered to be caused by an abnormality of the posterior semicircular canal otoliths. After head tilt toward affected ear or after head extension, rotational vertigo and nystagmus occur. The Dix-Hallpike maneuver (also known as the Nylen-Barany maneuver) is the standard test for BPPV and involves moving the patient rapidly from a sitting to a supine position with the head turned 45 degrees to the right or left; after 20–30 seconds, the patient is returned to the sitting position. The finding of rotatory nystagmus with limited duration is considered pathognomonic. Treatments include conservative therapy, vestibulosuppressants (e.g., meclizine), and canalith repositioning procedures (e.g., Semont or Epley maneuvers). Surgery (e.g., posterior canal occlusion) is limited to intractable cases.
 Vestibular neuritis. Typically affects young to middle-aged adults, with no gender preponderance. There is often a history of upper respiratory infection, and the etiology is thought to be viral in most cases. Vestibular neuritis is characterized by acute severe vertigo, nausea/vomiting, abnormal caloric testing, and falling to ipsilateral side. No tinnitus or deafness is present. It generally resolves within several weeks, and can be treated with antihistamines and/or antiemetic agents.
Vestibular neuritis. Typically affects young to middle-aged adults, with no gender preponderance. There is often a history of upper respiratory infection, and the etiology is thought to be viral in most cases. Vestibular neuritis is characterized by acute severe vertigo, nausea/vomiting, abnormal caloric testing, and falling to ipsilateral side. No tinnitus or deafness is present. It generally resolves within several weeks, and can be treated with antihistamines and/or antiemetic agents.
 Acute labyrinthitis, Like vestibular neuritis, but with associated tinnitus and hearing loss. May follow systemic or middle ear infections or use of ototoxic drugs (toxic labyrinthitis).
Acute labyrinthitis, Like vestibular neuritis, but with associated tinnitus and hearing loss. May follow systemic or middle ear infections or use of ototoxic drugs (toxic labyrinthitis).
 Labyrinthine hemorrhage or stroke secondary to thrombosis of the labyrinthine (internal auditory) artery. If the cochlear branch is involved, then deafness may occur as well.
Labyrinthine hemorrhage or stroke secondary to thrombosis of the labyrinthine (internal auditory) artery. If the cochlear branch is involved, then deafness may occur as well.
 Meniere disease, Recurrent vertigo with fluctuating unilateral tinnitus and low-tone sensorineural hearing loss (these are more likely later in the disease course). Typical onset at age 40 years, no gender preponderance. Onset abrupt, and episode may last minutes to hours. Usually unilateral, but can be bilateral in 20% of cases. Also sensation of fullness around affected ear. Horizontal nystagmus is contralateral (occurs during an acute attack) and falling is ipsilateral. Pathology thought secondary to endolymphatic hydrops (distension of the endolymphatic duct with rupture into the perilymph, dumping K+ that paralyzes the vestibular apparatus and may cause nerve degeneration over time).
Meniere disease, Recurrent vertigo with fluctuating unilateral tinnitus and low-tone sensorineural hearing loss (these are more likely later in the disease course). Typical onset at age 40 years, no gender preponderance. Onset abrupt, and episode may last minutes to hours. Usually unilateral, but can be bilateral in 20% of cases. Also sensation of fullness around affected ear. Horizontal nystagmus is contralateral (occurs during an acute attack) and falling is ipsilateral. Pathology thought secondary to endolymphatic hydrops (distension of the endolymphatic duct with rupture into the perilymph, dumping K+ that paralyzes the vestibular apparatus and may cause nerve degeneration over time).
 Vestibular schwannoma (acoustic neuroma). May also cause vertigo secondary to CN VIII involvement, but hearing loss and tinnitus are far more common presenting symptoms.
Vestibular schwannoma (acoustic neuroma). May also cause vertigo secondary to CN VIII involvement, but hearing loss and tinnitus are far more common presenting symptoms.
 Perilymphatic fistula. Pathologic communication between the fluid-filled space of the inner ear and the air-filled space of the middle ear (e.g., after trauma or barotrauma, postsurgical or idiopathic). Associated with sudden or progressive sensorineural hearing loss and vertigo. Surgical repair is often necessary.
Perilymphatic fistula. Pathologic communication between the fluid-filled space of the inner ear and the air-filled space of the middle ear (e.g., after trauma or barotrauma, postsurgical or idiopathic). Associated with sudden or progressive sensorineural hearing loss and vertigo. Surgical repair is often necessary.
 Systemic causes of dizziness/vertigo
Systemic causes of dizziness/vertigo
 Dizziness is a subjective term variably used to connote lightheadedness, faintness, and disequilibrium among other things, whereas vertigo refers specifically to an illusory sensation of movement (often described as spinning sensation).
Dizziness is a subjective term variably used to connote lightheadedness, faintness, and disequilibrium among other things, whereas vertigo refers specifically to an illusory sensation of movement (often described as spinning sensation).
 Cardiovascular disease (usually dizziness/syncope).
Cardiovascular disease (usually dizziness/syncope).
 Vasculitides (e.g., Cogan syndrome—vertigo, tinnitus, hearing loss, keratitis).
Vasculitides (e.g., Cogan syndrome—vertigo, tinnitus, hearing loss, keratitis).
 Hematologic disorders (hyperviscosity or anemia can both cause dizziness).
Hematologic disorders (hyperviscosity or anemia can both cause dizziness).
 Hypoglycemia (dizziness).
Hypoglycemia (dizziness).
 Hypothyroidism (associated with lightheadedness, dizziness, and occasionally vertigo).
Hypothyroidism (associated with lightheadedness, dizziness, and occasionally vertigo).
 Hyperventilation (dizziness, circumoral paresthesiae).
Hyperventilation (dizziness, circumoral paresthesiae).
 Ototoxic drugs (e.g., aminoglycoside antibiotics).
Ototoxic drugs (e.g., aminoglycoside antibiotics).
Auditory Pathway Lesions
Types
Cortical Lesions
• Unilateral damage to primary auditory cortex (Heschl gyri, area 41) causes a subtle impairment in spatial localization of sound.
• Damage to auditory association areas causes sound agnosia (difficulty identifying sounds).
• Bilateral temporal lesions affecting Heschl gyri and/or their interconnections may cause the syndrome of pure word deafness (auditory verbal agnosia).
Brainstem Lesions
• Brainstem lesions above the cochlear nuclei do not cause complete deafness.
• Lesion of the lateral lemniscus causes bilateral partial deafness, greater in the contralateral ear.
• Localization of auditory brainstem lesions can be assisted with brainstem auditory evoked responses (BAERs).
Cerebellopontine Angle and Peripheral Lesions
• Usually cause sensorineural hearing loss (deficit in perceiving tones or speech).
• Often associated with tinnitus (see below).
• Causes include the following:
1. Cerebellopontine angle (CPA)/IAC mass lesions. Typically cause unilateral high-pitched tinnitus and progressive sensorineural hearing loss. Include tumors or tumor-like lesions (e.g., schwannomas, epidermoids, meningiomas, arachnoid cysts) and vascular lesions such as AICA aneurysms.
2. Trauma (basal skull fracture with temporal bone involvement). Conductive hearing loss is classically associated with longitudinal fractures and sensorineural hearing loss with transverse fractures, but fractures are often complex and components of each may occur.
3. Infection (e.g., suppurative labyrinthitis, meningitis, syphilis).
4. Ototoxic drugs (e.g., aminoglycoside antibiotics).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree