Wrist and Hand Anatomy
The wrist consists of several synovial articulations among the distal radius, the distal ulna, the proximal carpal row (scaphoid, lunate, triquetrum, pisiform), and the distal carpal row (trapezium, trapezoid, capitate, and hamate). The radiocarpal joint between the distal radius and the proximal carpal row and the distal radioulnar joint between the radius and the ulna are separated by fibrocartilage, called the triangular fibrocartilage , which extends from the ulnar aspect of the distal radius to the base of the ulnar styloid. The midcarpal joint is located between the carpal bones and is separated from the radiocarpal joint by two interosseous ligaments, the scapholunate and lunotriquetral ligaments. The scapholunate ligament is “U” shaped in the sagittal plane, with the open end of the U distal, and it consists of a volar portion, a thin proximal or central portion, and a thick and mechanically important dorsal portion. Additional dorsal and palmar wrist ligaments are also present, named for their osseous attachments, categorized as intrinsic (intercarpal) or extrinsic (radiocarpal or ulnocarpal).
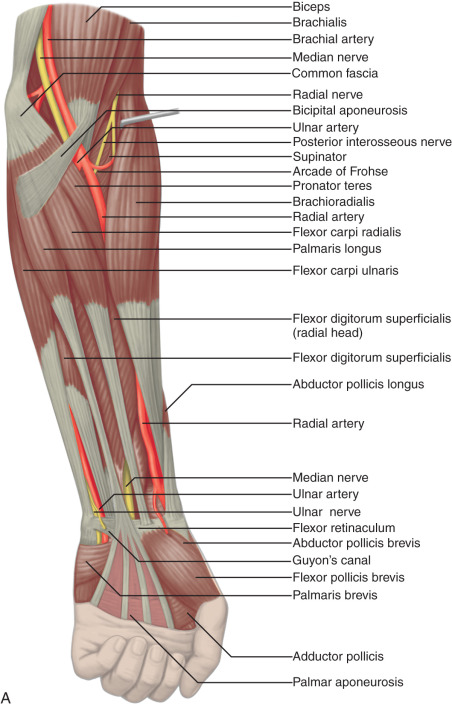
Structures enter the wrist through several fibro-osseous tunnels. In the volar wrist, the carpal tunnel contains the median nerve and the flexor digitorum profundus, flexor digitorum superficialis, and flexor pollicis longus tendons ( Fig. 5.1A–E ). The fibrous flexor retinaculum extends from the pisiform and hamate to the scaphoid and trapezium, to form the roof of the carpal tunnel. The Guyon or ulnar canal is also volar adjacent to the pisiform, which contains the ulnar nerve and ulnar artery and veins. Other tendons, the flexor carpi radialis and the palmaris longus tendons, are located outside the carpal tunnel, although the flexor carpi radialis is within its own fibro-osseous canal and distally is associated with the trapezium.




The tendons of the dorsal wrist are also separated into six fibro-osseous compartments (see Fig. 5.1C ). From radial to ulnar, they include the (1) abductor pollicis longus and extensor pollicis brevis, (2) extensor carpi radialis longus and brevis, (3) extensor pollicis longus, (4) extensor digitorum and extensor indicis, (5) extensor digiti minimi, and (6) extensor carpi ulnaris. A helpful bone landmark for orientation is the dorsal tubercle of the radius or Lister tubercle, which is located between the extensor carpi radialis tendons in the second compartment and the extensor pollicis longus tendon in the third compartment. The extensor carpi ulnaris is also found within a characteristic groove in the ulna.
The anatomy of the volar aspect of the fingers includes the flexor digitorum superficialis and profundus tendons. Each flexor superficialis tendon splits at the proximal interphalangeal joint, with each limb coursing to each side of the flexor digitorum profundus tendon to insert on the middle phalanx (see Fig. 5.1F–H ). The flexor digitorum profundus terminates at the distal phalanx. The flexor tendons are tethered or secured to the adjacent phalanges through a series of fibrous pulleys to prevent bowstringing of the tendons with flexion (see Fig. 5.1F ). The annular pulleys consist of the A1 pulley located at the metacarpophalangeal joint, the longer A2 pulley at the level of the proximal phalanx, the A3 pulley at the proximal interphalangeal joint, the A4 pulley at the level of the middle phalanx, and the A5 pulley at the distal interphalangeal joint. Smaller cruciform pulleys are located between these pulleys along the course of the flexor tendons. At the volar aspect of each metacarpophalangeal and interphalangeal joint is a fibrous structure called the volar or palmar plate . The metacarpophalangeal joints are stabilized by proper and accessory radial and ulnar collateral ligaments, with the latter extending to the volar plate. The interphalangeal joints are also stabilized by radial and ulnar collateral ligaments. The soft tissue distally at the volar aspect of distal phalanx is called the pulp .
At the dorsal aspect of each finger, the extensor digitorum tendon attaches to the middle phalanx as a central band, whereas slips of the extensor tendon that contribute to the lateral bands attach to the distal phalanx. The metacarpophalangeal joints have an overlying aponeurotic sheet or extensor hood, which consists of transverse-oriented sagittal bands that stabilize the extensor tendons. The metacarpophalangeal and interphalangeal joints are synovial articulations with prominent dorsal joint recesses.
Ultrasound Examination Technique
Tables 5.1 and 5.2 are ultrasound examination checklists. Examples of diagnostic wrist and hand ultrasound reports are shown in Box 5.1 and Box 5.2 .
Examination: Ultrasound of the Wrist
Date of Study: March 11, 2011
Patient Name: Derrick May
Registration Number: 8675309
History: Numbness, evaluate for carpal tunnel syndrome
Findings: The median nerve is unremarkable in appearance, measuring 8 mm 2 at the wrist crease and 7 mm 2 at the pronator quadratus. No evidence of tenosynovitis. The radiocarpal, midcarpal, and distal radioulnar joints are normal without effusion or synovial hypertrophy. The wrist tendons are normal without tear or tenosynovitis. Normal dorsal component of the scapholunate ligament. No dorsal or volar ganglion cyst. Unremarkable Guyon canal. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression: Unremarkable ultrasound examination of the wrist.
Examination: Ultrasound of the Wrist
Date of Study: March 11, 2011
Patient Name: Jacobim Mugatu
Registration Number: 8675309
History: Numbness, evaluate for carpal tunnel syndrome
Findings: The median nerve is hypoechoic and enlarged, measuring 15 mm 2 at the wrist crease and 7 mm 2 at the pronator quadratus. No evidence for tenosynovitis. The radiocarpal, midcarpal, and distal radioulnar joints are normal without effusion or synovial hypertrophy. The wrist tendons are normal without tear or tenosynovitis. Normal dorsal component of the scapholunate ligament. No dorsal ganglion cyst. A 7-mm volar ganglion cyst is noted between the radial artery and flexor carpi radialis tendon. Unremarkable Guyon canal. Additional focused evaluation at site of maximal symptoms was unrevealing.
Impression:
- 1.
Ultrasound findings compatible with carpal tunnel syndrome.
- 2.
A 7-mm volar ganglion cyst.
General Comments
Ultrasound examination of the wrist and hand is typically completed with the patient sitting and the hand resting on the examination table. This position allows easy comparison between each side if needed. A high-frequency transducer of at least 10 MHz is typically used because most of the structures are superficial, and a transducer with a small footprint is often helpful to maintain contact with the soft tissues under examination. I favor thick transmission gel over a stand-off pad. Evaluation of the wrist and hand may be focused over the area that is clinically symptomatic or relevant to the patient’s history. Regardless, a complete examination of all areas should always be considered for one to become familiar with normal anatomy and normal variants and to develop an efficient and comprehensive sonographic technique.
Wrist: Volar Evaluation
Median Nerve, Flexor Digitorum Tendons, and Volar Joint Recesses
The primary structures evaluated from the volar aspect at midline are the median nerve, the flexor tendons, and the volar aspects of the wrist joints. Examination begins short axis to the tendons and median nerve in the center of the wrist. For evaluation of the median nerve, the transducer is placed in the transverse plane at the level of the wrist crease, which is at the proximal aspect of the carpal tunnel ( Fig. 5.2 ). Normal peripheral nerves have a honeycomb appearance when they are imaged in short axis from hypoechoic nerve fascicles and surrounding hyperechoic connective tissue ( Fig. 5.2B ). Toggling the transducer to angle the sound beam along the long axis of the median nerve will help to show the characteristic appearance of the nerve when the sound beam is perpendicular ( ). Because peripheral nerve trunks are composed of both hypoechoic and hyperechoic elements, the median nerve appears relatively hypoechoic when surrounded by hyperechoic tissue in the carpal tunnel and relatively hyperechoic when surrounded by hypoechoic muscle in the forearm. At the wrist crease, the median nerve is identified by its hypoechoic nerve fascicles, which are most conspicuous surrounded by the adjacent hyperechoic tendons. If differentiation between the median nerve and adjacent tendons is difficult, median nerve identification is easily accomplished with movement of the transducer proximally in the transverse plane. During this maneuver, the normal median nerve courses radial to the flexor tendons and then moves ulnar and deep between the flexor digitorum superficialis and profundus ( Fig. 5.3 ) ( ). In addition, the median nerve now appears relatively hyperechoic as a result of the connective tissue and fat because it is surrounded by hypoechoic muscle. The characteristic course, location, and echogenicity assist in identification of the median nerve. An additional method to differentiate the median nerve from the adjacent flexor tendons at the wrist crease in the transverse plane is angulation of or toggling the transducer along the long axis of the tendons. This maneuver causes the hyperechoic tendons to become hypoechoic as a result of anisotropy, whereas the hypoechoic median nerve fascicles remain unchanged ( ). Evaluation of the median nerve is then continued distally into the carpal tunnel, where the thin and hyperechoic flexor retinaculum can be visualized, which attaches to the pisiform and trapezium proximally ( Fig. 5.2C ) and the hamate and scaphoid distally ( Fig. 5.2D ). A small branch of the median nerve, the palmar cutaneous branch, originates proximal to the carpal tunnel and courses superficial to the flexor retinaculum and ulnar to the flexor carpi radialis tendon ( Fig. 5.2E ). The thenar motor branch can also be visualized at the carpal tunnel outlet originating from the palmar ulnar aspect of the radial division of the median nerve, coursing vertically in a palmar direction and extending proximal between the abductor pollicis brevis and flexor pollicis brevis ( Fig. 5.2F ). The transducer is turned 90 degrees to visualize the median nerve in long axis ( Fig. 5.4 ) ( ). The variable appearance of peripheral nerve echogenicity relative to the surrounding tissue echogenicity is well demonstrated when imaging the median nerve in long axis in the distal forearm ( Fig. 5.4D ). Proximal to the wrist joint in the transverse plane, the pronator quadratus can be identified extending between the distal radius and ulna, a soft tissue landmark that is used for proximal measurement of the median nerve ( Fig. 5.3A ).












Attention is then turned back to the flexor tendons, with each tendon evaluated in both short axis and long axis. The flexor digitorum superficialis and profundus are identified about the median nerve as described earlier, proximally as hypoechoic muscle and distally as fibrillar and hyperechoic tendons (see Figs. 5.2 and 5.3 ). Just beyond the wrist crease, the thin hyperechoic flexor retinaculum is seen as it extends from the proximal scaphoid pole to the pisiform and from the trapezium to the hook of the hamate, which represents the roof the carpal tunnel (see Fig. 5.2D ). If the retinaculum is not imaged perpendicular to the ultrasound beam, it will appear hypoechoic as a result of anisotropy. The flexor digitorum tendons travel through the carpal tunnel to the digits, whereas the palmaris longus tendon, typically directly superficial to the median nerve, remains outside of the carpal tunnel. In the sagittal plane and long axis to the flexor tendons, the volar radiocarpal and midcarpal joint recesses are identified by the adjacent bone contours; the volar lip of the distal radius, the lunate bone, and the capitate bone have characteristic shapes (see Fig. 5.4B and C ). Between the distal radius and the lunate is the volar recess of the radiocarpal joint, and between the lunate and capitate bones is the volar recess of the midcarpal joint. The distal radioulnar joint is identified with placement of the transducer in the transverse plane between the distal radius and ulna.
Scaphoid, Flexor Carpi Radialis Tendon, Radial Artery, and Volar Ganglion Cysts
Evaluation of the radial aspect of the volar wrist begins in the transverse plane at the wrist crease. In this position, the various tendons of the volar wrist are identified. Just radial to the median nerve and somewhat similar in size is the flexor carpi radialis tendon, located outside the carpal tunnel in its own fibro-osseous canal (see Fig. 5.2B ). Ultrasound evaluation is completed in both long and short axis from proximal to the distal insertion of the flexor carpi radialis tendon on the second and third metacarpals, although some fibers insert onto the trapezium tuberosity. With placement of the transducer over the distal aspect of the flexor carpi radialis tendon in long axis ( Fig. 5.5 ), the characteristic bilobed or peanut-shaped bone contours of the scaphoid bone are identified deep to this tendon ( Fig. 5.5C ). The normal smooth and hyperechoic bone surface of the scaphoid bone is evaluated for cortical step-off fracture. Returning to the wrist crease in the transverse plane ( Fig. 5.6A ), the radial artery and veins are identified immediately radial to the flexor carpi radialis tendon ( Fig. 5.6B ). With the flexor carpi radialis tendon and radial artery in view, the transducer is moved both proximally and distally from the radiocarpal joint to evaluate for ganglion cysts. Placement of the transducer in the transverse plane between the scaphoid and lunate will show the normal hyperechoic and fibrillar volar component of the scapholunate ligament ( Fig. 5.6C ).






Ulnar Artery, Vein, and Nerve (Guyon Canal)
Evaluation of the ulnar aspect of the volar wrist begins in the transverse plane at the wrist crease. Moving the transducer ulnar to the carpal tunnel ( Fig. 5.7A ), the bone landmark of the pisiform is identified ( Fig. 5.7B ). Between the pisiform and the ulnar artery, the ulnar nerve is identified as hypoechoic nerve fascicles and surrounding hyperechoic connective tissue. The ulnar veins are usually not visible because they are easily compressed by pressure of the ultrasound transducer. As the transducer is moved distally, the hyperechoic and shadowing surface of the hook of the hamate is seen deep to the ulnar nerve and artery. The ulnar nerve branches, with a deep motor branch coursing along the ulnar side of the hamate hook and one to two predominantly sensory branches superficial to the hamate hook ( Fig. 5.7C ). This area should be evaluated as trauma can cause ulnar nerve and artery abnormalities as a result of compression by the hook of the hamate. Proximal to the pisiform, the flexor carpi ulnaris is identified as well as the dorsal cutaneous branch of the ulnar nerve coursing from volar to dorsal beneath the flexor carpi ulnaris ( Fig. 5.7D ). Evaluation of the ulnar artery and nerve is also completed in long axis ( Fig. 5.8 ).






Wrist: Dorsal Evaluation
Dorsal Wrist Tendons and Dorsal Joint Recesses
The primary structures of the dorsal wrist are the various extensor and abductor tendons of the six wrist compartments, and the dorsal radiocarpal, midcarpal, and distal radioulnar joint recesses. Evaluation of the dorsal tendons begins in the transverse plane over the Lister tubercle of the dorsal radius ( Fig. 5.9A and B ). This structure serves as an important starting point for dorsal wrist evaluation and assists in orientation and accurate identification of the wrist tendons. The Lister tubercle is seen as a pronounced bony prominence. Once the Lister tubercle is identified, the tendon immediately ulnar to it is the extensor pollicis longus of the third extensor compartment ( Fig. 5.9B ). Often there is an additional smaller dorsal radial protuberance at the ulnar aspect of the extensor pollicis longus as well. With movement of the transducer in the radial direction ( Fig. 5.9C ), the extensor carpi radialis brevis and then the extensor carpi radialis longus tendons are seen in the second extensor compartment ( Fig. 5.9D ). On further radial movement of the transducer, the extensor pollicis brevis and abductor pollicis longus tendons are seen in the first extensor compartment ( Fig. 5.9D ). It may be helpful to remember that the names of the tendons alternate from longus to brevis, beginning at the extensor pollicis longus and moving in a radial direction. The extensor pollicis longus tendon courses toward the thumb superficial to the extensor carpi radialis and ulnaris tendons in an oblique fashion proximally to distally. Therefore when short axis to the extensor carpi radialis brevis and longus tendons are moving distally, the extensor pollicis longus is seen moving in an ulnar to radial direction over the extensor carpi radialis brevis and longus tendons, a potential site of intersection syndrome ( Fig. 5.9E ) ( ). In the region of the first extensor wrist compartment, the superficial branch of the radial nerve can be seen as it courses from the volar to the dorsal aspect of the distal forearm superficial to the first extensor wrist compartment tendons and extensor retinaculum, near branches of the cephalic vein ( Fig. 5.9F ).




Beginning again in the transverse plane at the Lister tubercle, transducer movement ulnar from the extensor pollicis longus tendon ( Fig. 5.10A ) shows the extensor indicis and multiple tendons of the extensor digitorum in the fourth wrist compartment, and the extensor digiti minimi in the fifth wrist compartment near the distal radioulnar joint ( Fig. 5.10B ). The posterior interosseous nerve is identified deep within the radial aspect of the fourth dorsal extensor compartment ( Fig. 5.9B ). Over the most ulnar aspect of the ulna, the extensor carpi ulnaris tendon is identified in a concave groove of the ulna in the sixth extensor compartment ( Fig. 5.10C ). The extensor carpi ulnaris tendon often has a normal thin hypoechoic longitudinal cleft that should not be interpreted as a tendon tear. The dorsal retinaculum and the deeper subsheath stabilize the extensor carpi ulnaris, with the latter attaching to the ulna. Up to 50% of the extensor carpi ulnar tendon can be located outside of the groove and still be considered normal.



Each of the extensor tendons is also imaged in long axis throughout the wrist ( Fig. 5.11 ). The extensor retinaculum courses transversely but slightly oblique over the extensor tendons and appears hyperechoic, measuring up to 1.7 mm thick and 23 mm wide in cross section ( Fig. 5.11B ). If imaged oblique to the ultrasound beam, the extensor retinaculum can appear artifactually hypoechoic as a result of anisotropy, which should not be misinterpreted as tenosynovitis. Similar to the volar wrist, the dorsal recesses of the radiocarpal joint (between the radius and proximal carpal row), the midcarpal joint, and the distal radioulnar joint are identified with recognition of the characteristic bone contours for orientation. The radiocarpal and midcarpal joint recesses are optimally evaluated in the sagittal plane, whereas the distal radioulnar joint is evaluated in the transverse plane ( Fig. 5.10B ).


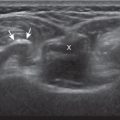
Scapholunate Ligament (Dorsal Component) and Dorsal Ganglion Cysts
Similar to the dorsal tendons, evaluation of the scapholunate ligament begins in the transverse plane over the Lister tubercle ( Fig. 5.9A ). As the transducer is then moved distally, the bone contours of the radius are interrupted by the radiocarpal joint, and the next osseous structure visualized is the scaphoid. With movement of the transducer in the ulnar direction, the adjacent lunate bone is brought into view. Between the dorsal aspects of the scaphoid and the lunate is a triangular area where one sees the dorsal aspect of the scapholunate ligament, which has a compact hyperechoic fibrillar echotexture ( Fig. 5.12 ). Directly superficial to the dorsal aspect of the scapholunate ligament, the dorsal radiocarpal ligament (or dorsal radiotriquetral ligament) is identified. This area is a common site for dorsal wrist ganglion cysts.

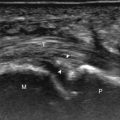
Triangular Fibrocartilage Complex
The triangular fibrocartilage complex consists of the triangular fibrocartilage, the meniscus homologue, the extensor carpi ulnaris tendon sheath, and the volar and dorsal radiocarpal ligaments. For evaluation of the triangular fibrocartilage, the transducer is placed in the sagittal plane over the dorsal lateral wrist to identify the bone contours of the distal ulna and then moved toward the coronal plane with the wrist in slight radial deviation ( Fig. 5.13A ). A hyperechoic slab of tissue is identified as it extends from the ulnar styloid base to the radius, which represents the triangular fibrocartilage ( Fig. 5.13B ). The radial attachment of the triangular fibrocartilage must be identified to ensure complete evaluation as this may be a site of traumatic tears. Evaluation of the triangular fibrocartilage can be difficult given its orientation in the transverse plane extending away from the transducer, and often a lower frequency transducer is helpful. The meniscus homologue is seen as a hyperechoic triangular structure with its base adjacent to the extensor carpi ulnar tendon and in contact with the triquetrum, and this should not be mistaken for the triangular fibrocartilage, which is thinner, more proximal, and directly over the ulnar head.


Finger Evaluation
Volar
At the volar aspect of the finger in long axis ( Fig. 5.14A ), both the hyperechoic and fibrillar flexor digitorum superficialis and profundus tendons can be seen at the level of the metacarpophalangeal joint with the overlying A1 pulley ( Fig. 5.14B ). The pulleys often have a trilaminar appearance at ultrasound, consisting of the superficial reflective surface of the pulley, the relatively hypoechoic pulley, and the deeper hyper-reflective surface of the adjacent flexor tendon sheath. With regard to imaging the flexor tendons in long axis, the individual tendons can be distinguished from each other with isolated passive movement of the distal phalanx because this will cause movement of the flexor digitorum profundus. At the level of the proximal phalanx, the A2 pulley can be identified; slight obliquity of the transducer may make the pulley appear hypoechoic from anisotropy and can aid in its identification ( Fig. 5.14C ). The A2 pulley normally is thicker distally, which assists in its identification. At the level of the proximal interphalangeal joint, the hyperechoic volar (or palmar) plate is identified ( Fig. 5.14D and E ). The A3 and A4 pulleys are also identified superficial to the flexor tendons, at the level of the proximal interphalangeal joint and middle phalanx, respectively ( Fig. 5.14D ). Just distal to the proximal interphalangeal joint, the flexor digitorum superficialis inserts on the middle phalanx in the parasagittal plane, whereas the flexor digitorum profundus extends distally over the volar plate of the distal interphalangeal joint in the sagittal plane to insert on the distal phalanx ( Fig. 5.14E ). The flexor digitorum superficialis inserts on the middle phalanx by dividing into two bundles, with each segment moving around the flexor digitorum profundus tendon. This is best appreciated by imaging in short axis ( Fig. 5.15A and B ). More proximally over the palm of the hand ( Fig. 5.16 ), the lumbrical and interosseous muscles can be identified, as can the common and proper palmar digital arteries and nerves. The metacarpophalangeal and interphalangeal joints are also evaluated in the sagittal plane for volar plate abnormality and joint recess distention from fluid or synovial disorders.








Dorsal
At the dorsal aspect of each digit, the thin, hyperechoic, and fibrillar extensor digitorum tendon extends over the metacarpophalangeal joint in the sagittal plane ( Fig. 5.17A and B ). At the level of the proximal interphalangeal joint, the central band of the extensor tendon inserts on the middle phalanx ( Fig. 5.17C and D ). With movement of the transducer just off midline of the phalanx, the slips of the extensor tendon to the lateral bands can be seen ( Fig. 5.17E ), which insert distally on the distal phalanx ( Fig. 5.17F ). The ultrasound beam penetrates through the nail and allows visualization of the underlying hypoechoic nail bed, subungual space, and the surface of the distal phalanx ( Fig. 5.17F ). At the level of the metacarpophalangeal joint, the transducer is positioned short axis to the extensor tendon, and the finger is flexed to evaluate for subluxation of the tendon, which would indicate sagittal band injury. The joints of each digit are also evaluated for distention from fluid or synovial hypertrophy, where the dorsal joint recess extends proximally beneath the extensor tendon. In addition, the hypoechoic hyaline articular cartilage of each joint can be visualized, which is accessible with flexion of the digits ( Fig. 5.17G–I ). A triangular region of connective tissue is normally found superficial to the metacarpophalangeal joint articulation ( Fig. 5.17H ). The dorsal metacarpophalangeal joints are imaged in both the sagittal and transverse planes to evaluate for synovial hypertrophy and erosions.






Ligaments
The collateral ligaments of the digits can also be assessed with ultrasound in the coronal plane around each individual joint. To specifically evaluate the ulnar collateral ligament of the first metacarpophalangeal joint, the hand is placed around a rolled-up towel, and the transducer is placed in the coronal plane relative to the first metacarpophalangeal joint ( Fig. 5.18A ). The (proper) ulnar collateral ligament proper will appear in long axis as hyperechoic with a compact fibrillar echotexture, extending from a broad concavity in the metacarpal to the proximal phalanx ( Fig. 5.18B ). Because the subcutaneous fat directly overlying the ulnar collateral ligament is hyperechoic, the ligament may appear relatively hypoechoic but should be fibrillar and of relatively uniform thickness. Additionally, the ligament may appear artifactually hypoechoic where it is oblique to the sound beam from anisotropy. The overlying adductor pollicis aponeurosis, which is specific to the ulnar collateral ligament of the first metacarpophalangeal joint, is seen as a thin hypoechoic structure over the ulnar collateral ligament. Flexion of the interphalangeal joint will produce isolated movement of the adductor pollicis aponeurosis, which assists in its identification ( ). An additional dynamic maneuver in assessment of any collateral ligament is stressing the joint (valgus for ulnar ligaments, varus for radial ligaments). This is accomplished with minimal stress and is helpful because joint fluid will often move into the ligament tear under ultrasound visualization to improve detection. Other ulnar and radial collateral ligaments of the digits similarly appear as compact and hyperechoic fibrillar structures, which extend across each joint.


Joint Abnormalities
There are multiple synovial articulations of the hand and wrist and each individual site should be evaluated for joint abnormalities. In the sagittal plane, the volar and dorsal recesses of the radiocarpal and midcarpal joints are assessed for abnormal distention ( Fig. 5.19A and B ). The distal radioulnar joint is also assessed from both dorsal and volar aspects in the transverse plane ( Fig. 5.19C ). The digits are assessed in the sagittal plane over each joint, including the dorsal and volar joint recesses ( Fig. 5.19D and E ). Anechoic distention of a joint recess typically represents simple fluid, although possible etiologies include degenerative, reactive, traumatic, and inflammatory causes; if there is concern for infection, ultrasound-guided aspiration should be considered. In the setting of trauma, one must evaluate the osseous structures at any focal area of symptoms for cortical step-off deformity, which would indicate fracture.

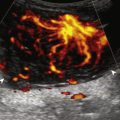
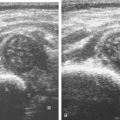
If a joint recess distention is not anechoic, considerations include complex fluid ( Fig. 5.20 ) versus synovial hypertrophy ( Fig. 5.21 ). Differentiation between these two etiologies may be difficult as both may appear hypoechoic or isoechoic compared with the overlying subcutaneous tissues. If joint recess distention collapses with transducer pressure or joint movement ( ), or if swirling of echoes within the recess are identified, and if there is no internal flow on color Doppler imaging, then complex fluid is suspected. In contrast, if there is no displacement, little compressibility of the joint recess, and internal flow on color Doppler imaging, then synovial hypertrophy is likely ( Fig. 5.21 ) ( ). Ultrasound-guided aspiration may be needed to make this determination. Because dorsal wrist ganglion cysts occur at the site of the dorsal radiocarpal joint recess and may appear similar, dynamic imaging with compression and joint movement also helps in their differentiation; a ganglion cyst is typically multilocular and noncompressible (see Fig. 5.89 ), whereas a fluid-filled joint recess is compressible and unilocular ( ). Possible etiologies for both complex fluid and synovial hypertrophy include hemorrhage and inflammation, which includes infection ( Fig. 5.22 ), rheumatoid arthritis ( Fig. 5.23 ) ( ), psoriatic arthritis ( Fig. 5.24 ), systemic lupus erythematosus ( Fig. 5.25 ), and gout ( Fig. 5.26 ) ( ), among other inflammatory arthritides.








Synovial hypertrophy appears as nondisplaceable and poorly or noncompressible distention of a joint recess that is hypoechoic ( Fig. 5.27 ) or less frequently isoechoic or hyperechoic compared with the adjacent subdermal fat ( Fig. 5.27C ). Active inflammatory synovitis is usually hypoechoic with hyperemia on color Doppler imaging. When evaluating superficial structures, the transducer should be “floated” on a thick layer of gel with minimal transducer pressure so as to not compress the vascularity. The ultrasound finding of synovial thickening without hyperemia is not specific for one diagnosis and may be seen with osteoarthritis as well as asymptomatic subjects; therefore, assessing multiple joints and review of history, laboratory values, distribution, and radiographic findings are important for the synthesis of a concise diagnosis of inflammatory arthritis. While uncommon with osteoarthritis, inflammatory changes as shown by ultrasound are more prevalent with erosive osteoarthritis. Synovial proliferative disorders such as pigmented villonodular synovitis and synovial chondromatosis are other considerations when synovial hypertrophy is identified. In the latter condition, superimposed hyperechoic calcifications may be seen in the synovial tissue.