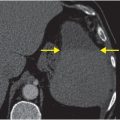
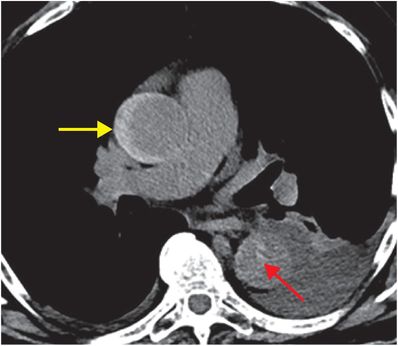
Diagnosis: Main right pulmonary artery embolus and thrombosed type B aortic dissection
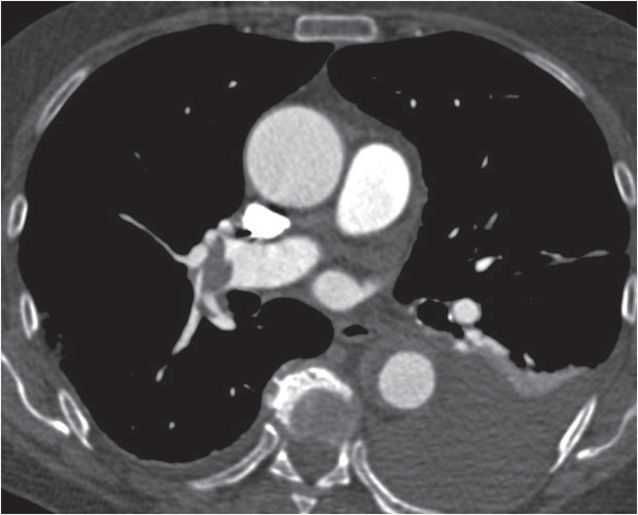
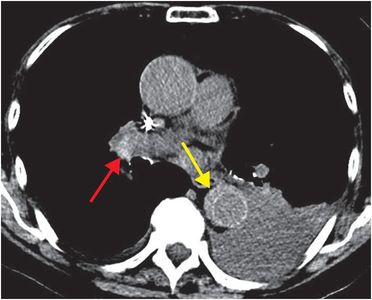
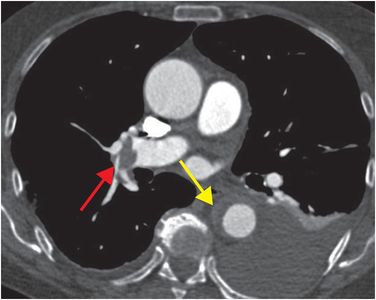
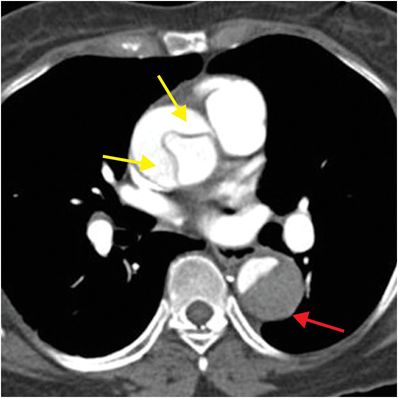
Unenhanced (left) and contrast-enhanced (right) axial CT of the chest shows crescentic high attenuation in the descending thoracic aorta on unenhanced CT that does not enhance following intravenous contrast material (yellow arrows). Pulmonary embolus is present in the right main pulmonary artery (red arrows).
Discussion
Overview of aortic dissection (pulmonary embolism is case 31)
CT is the modality of choice for evaluating aortic dissection. Most institutions perform a low-dose unenhanced CT followed by a contrast-enhanced CT of the chest.
Although aortic dissection occurs most commonly in older hypertensive patients, risk factors in younger patients include hypertension, connective tissue diseases (e.g., Marfans, Ehlers–Danlos), bicuspid aortic valve, aortic coarctation, pregnancy, and cocaine use.
Approximately 60% of aortic dissections involve the ascending aorta (type A) and 40% involve the descending aorta (type B).
Type A dissection is usually accompanied by substernal chest pain at onset, while type B dissection is usually accompanied by interscapular back pain at onset. Pain symptoms can migrate as aortic dissection progresses, and can abate as the dissection stops.
Type A dissection is generally managed surgically, and type B dissection is generally managed medically. In-hospital mortality is 26% and 11% for type A and type B dissection, respectively.
Clinical synopsis
The patient was admitted to the hospital where echocardiography showed no evidence of right heart strain despite the large burden of pulmonary embolus. A decision was made not to anticoagulate the patient because of the aortic dissection. An IVC filter was placed because of the continued presence of DVT in both lower extremities. The aortic dissection was managed medically with a beta-blocker for blood pressure control. The patient became asymptomatic and was discharged to rehabilitation 5 days later.
Self-assessment
|
|
|
|
|
|
|
|
|
|
Spectrum of aortic dissection
The spectrum of aortic dissection ranges from conspicuous intimal flap to subtle thickening of the aortic wall. Dissection may involve both the ascending and descending aorta, or be confined to either. Extent of dissection may be limited to several centimeters within a single segment, or involve the entire aorta and propagate distally into the common iliac arteries. Associated complications of aortic dissection may be absent, or may include aortic rupture, thrombosis, and/or end-organ ischemia/infarction.
Stanford type A / DeBakey type I aortic dissection
Approximately 60% of aortic dissections involve the ascending aorta. Because ascending aortic involvement is associated with higher mortality when treated medically, dissection involving this segment is generally managed surgically. Axial CT angiogram demonstrates an obvious dissection flap involving the ascending aorta with beak sign in the false lumen (arrow) where the flap meets the aortic wall. The true lumen is the inner lumen. In the descending aorta the false lumen is unperfused and larger than the true lumen (red arrow).
Stanford type A / DeBakey type I aortic dissection
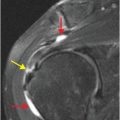
The false lumen of an aortic dissection can thrombose, which may diminish conspicuity of the pathognomonic feature of dissection, the intimal flap. When this occurs, unenhanced CT will reveal smooth, crescentic high attenuation. Following administration of intravenous contrast material, the false lumen will not perfuse. Unenhanced CT (top image) shows crescentic high attenuation intramural hematoma in the ascending aorta (yellow arrow) and the intimal flap sign in the descending aorta (red arrow). Following intravenous contrast material, no significant enhancement is seen in the thrombosed ascending false lumen (yellow arrow). There is some enhancement of the false lumen in the descending aorta indicating slow flow as compared to the true lumen (red arrow).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree