CHAPTER 71 Arterial Anatomy of the Thorax
THORACIC AORTA
Normal Anatomy
The thoracic aorta can be divided into five segments: the aortic root, the ascending aorta, the proximal and posterior aortic arch (or aortic isthmus), and the descending aorta (Fig. 71-1). The aortic root is the short segment of the aorta that arises from the left ventricle to include the aortic valve and the sinuses of Valsalva. The right and left coronary arteries arise from the sinuses of Valsalva (Fig. 71-2). The sinotubular junction delineates this segment from the ascending aorta, which extends from the sinotubular junction to the first branch of the aortic arch. Although the average diameter of the ascending aorta is 3.5 cm, the diameter at which surgical repair is considered is 5.5 cm.1 The ascending aorta is branchless. It remains enveloped within the uppermost extent of the serous pericardium, and in some cases, in the presence of pericardial fluid, the transverse pericardial recess can be seen surrounding part of the ascending aorta. As the ascending aorta travels cephalad, it curves toward the right just above the right atrium and slightly anterior to the superior vena cava. It conventionally lies to the right of the main pulmonary artery and anterior to the right pulmonary artery, which branches from the main pulmonary artery at a lower level than that of the left pulmonary artery (Figs. 71-3 and 71-4).
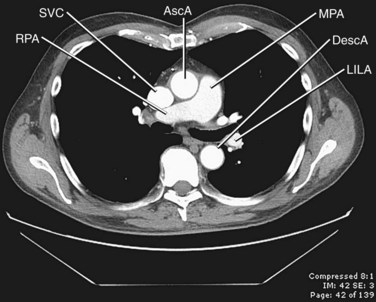
 FIGURE 71-4 Contrast-enhanced CT image through the middle mediastinum inferior to Figure 71-3 shows the origin of the right pulmonary artery (RPA) arising from the main pulmonary artery (MPA). The main pulmonary artery lies to the left of the ascending aorta (AscA), and the right pulmonary artery runs posterior to the superior vena cava (SVC). DescA, descending aorta; LILA, left interlobar artery.
FIGURE 71-4 Contrast-enhanced CT image through the middle mediastinum inferior to Figure 71-3 shows the origin of the right pulmonary artery (RPA) arising from the main pulmonary artery (MPA). The main pulmonary artery lies to the left of the ascending aorta (AscA), and the right pulmonary artery runs posterior to the superior vena cava (SVC). DescA, descending aorta; LILA, left interlobar artery.
The aortic arch is defined from the origin of the right brachiocephalic artery to the insertion of the ductus arteriosus, the ligamentum arteriosum in the adult. The arch courses obliquely through the anterior mediastinum from anterior to posterior and horizontally from right to left. Anterior to the arch lies the prevascular space, which is typically composed of mediastinal fat. The trachea is posterior to the proximal portion of the arch and is located to the right of the distal or posterior arch. The superior vena cava is conventionally to the right of the proximal arch (Fig. 71-5). The proximal aortic arch typically includes three branches in the following order from right to left: the right brachiocephalic, the left common carotid, and the left subclavian artery (Fig. 71-6). The distal segment of the arch, also known as the aortic isthmus, includes the portion extending from the left subclavian artery to the ligamentum arteriosum (Fig. 71-7). The ligamentum arteriosum represents the remnant of fetal circulation that shunts blood from the pulmonary artery to the arch and can often be identified in adults by associated calcification.
The descending aorta is divided into thoracic and abdominal portions. The thoracic segment of the descending aorta extends from the ligamentum arteriosum to the diaphragmatic aortic hiatus, at approximately T10. The average diameter is 2.48 cm, ranging from 1.6 to 3.7 cm. However, surgical intervention is considered when the diameter is greater than 6.5 cm.1 The descending thoracic aorta tapers distally and just above the diaphragm has an average diameter of 2.42 cm, with ranges from 1.4 to 3.3 cm.2 It courses along the left aspect of the spine within the posterior mediastinum. There are several paired branches arising from the descending thoracic aorta, which include the bronchial arteries, the esophageal arteries, and the posterior intercostal arteries. Phrenic branches and pericardial branches are also typically present.
Variant Anatomy
Variant branching patterns of the arch vessels are frequently encountered, particularly within the black population. The term bovine arch is a commonly used misnomer that refers to common origin of the brachiocephalic and left common carotid arteries (Fig. 71-8). Cadaveric studies show an overall incidence of 13%, with an incidence of 25% in blacks and 8% in whites.3 A variant of this, also erroneously referred to as bovine arch, consists of the left common carotid arising as a branch from the brachiocephalic artery, usually between 1 and 2.5 cm from the brachiocephalic origin.4 The incidence is 9% in the overall population, with 10% seen in blacks and 5% seen in whites.4
Anomalies of the aortic arch are rare, with the exception of the left aortic arch with aberrant right subclavian artery, which has an occurrence of 1 : 200.5 The incidence of the remaining anomalies is reported as less than 1% of all congenital cardiac anomalies; 85% to 95% of the arch anomalies are double aortic arch and right aortic arch with aberrant left subclavian artery.6 Arch anomalies are characterized by their sidedness as well as by the branching patterns off of the arch. There are five described anomalies: double aortic arch, right-sided aortic arch with mirror-image branching, right-sided aortic arch with abnormal branching, left-sided arch with abnormal branching, and cervical aortic arch.
To understand the origin of these variants, it is necessary to understand the embryology of the aortic arch. There are six paired aortic arches in the fetus as well as two dorsal aortae. The first and second aortic arches contribute to the formation of the stapedial artery. The third arches form the carotid system, including the right and left common, external, and internal carotids. The left fourth arch forms the aortic arch; the right forms a portion of the right subclavian artery. The fifth pair of aortic arches regress in their entirety. The sixth arches contribute to the development of the right and left pulmonary arteries, and the left also forms the ductus arteriosus. The left seventh segmental artery forms the left subclavian artery. The right seventh segmental artery contributes to the distal right subclavian artery. The right subclavian artery also receives contributions from the dorsal aorta.7 It is the abnormal regression or persistence of these structures that contributes to the anomalies discussed next (Fig. 71-9).8
In the normal development of the arch, the right dorsal aorta as well as a portion of the right sixth aortic arch regresses. In double aortic arch development, both of the paired dorsal aortae persist, with regression or persistence of the sixth arch, which contributes to the formation of the ductus arteriosus. Because there is complete encasement of the trachea and esophagus, patients often present early in life with nonpositional stridor. Double aortic arch can be seen on plain film radiography as a posterior indentation on the trachea by the right arch on lateral view and often on the posteroanterior view as tracheal indentations by the more superior right arch and inferior left arch. However, CT and MRI are the preferred methods for characterization of the anatomy as well as of any associated cardiac anomalies. Axial images demonstrate the “four artery sign,” representing paired carotid and subclavian arteries, evenly spaced around the trachea, just cephalad to the aortic arch (Fig. 71-10).9
When there is persistence of the right dorsal aorta and the left dorsal aorta regresses, a right-sided arch develops. There are three subtypes of right aortic arch, depending on the branching pattern. Mirror-image branching replicates the order of branching seen with a left-sided aorta, with a left brachiocephalic artery arising first, followed by the right common carotid and then the right subclavian artery (Fig. 71-11). A left-sided ductus arteriosus is typically seen with this entity, passing between the descending aorta and left pulmonary artery. Right aortic arch with mirror-image branching is almost always associated with congenital heart anomalies, most commonly tetralogy of Fallot, reported in 25% of cases.10
With right aortic arch with aberrant left subclavian artery, there is abnormal dorsal aortic regression between the origins of the left common and the left subclavian arteries. The left subclavian arises from a retroesophageal diverticulum, which is the remnant of the regressed dorsal segment.11 The ductus arteriosus arises from this diverticulum and connects to the left pulmonary artery, creating a complete vascular ring (Fig. 71-12). Because this condition forms a complete vascular ring, these patients often present with nonpositional stridor due to airway compression.11
Right aortic arch can also be seen with an isolated left subclavian artery, which has no direct communication to the aorta. Instead of originating from the arch, an isolated left subclavian artery arises from the left pulmonary artery through the ductus arteriosus. The embryologic origin of this anomaly is hypothesized to involve regression of the fourth arch as well as a portion of the sixth arch, with migration of the seventh intersegmental artery to the level of the sixth arch, forming the communication between the ductus and the pulmonary artery (which arises from the left sixth arch) and the left subclavian artery (arising from the seventh intersegmental artery).12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


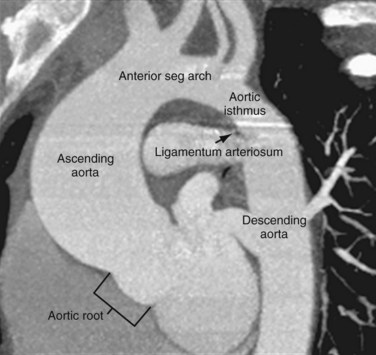
 FIGURE 71-1
FIGURE 71-1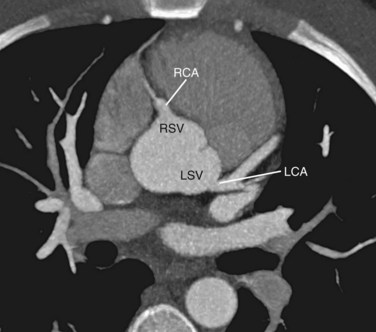
 FIGURE 71-2
FIGURE 71-2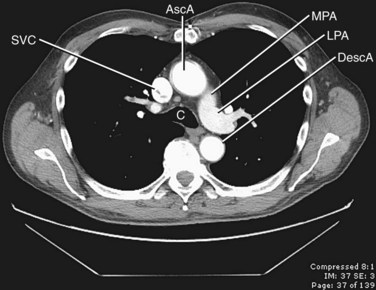
 FIGURE 71-3
FIGURE 71-3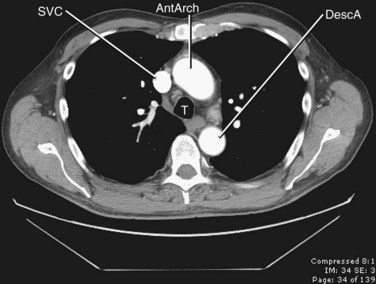
 FIGURE 71-5
FIGURE 71-5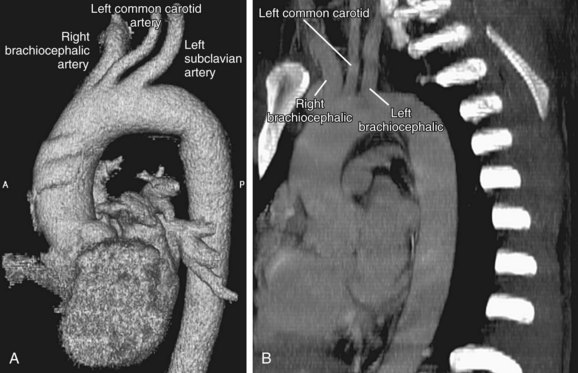
 FIGURE 71-6
FIGURE 71-6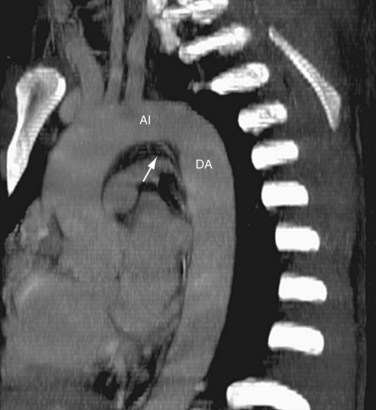
 FIGURE 71-7
FIGURE 71-7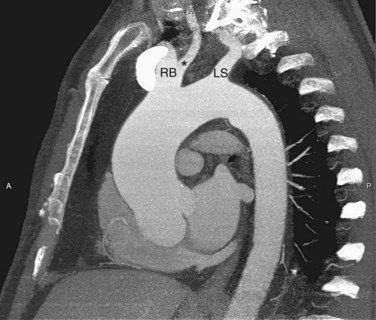
 FIGURE 71-8
FIGURE 71-8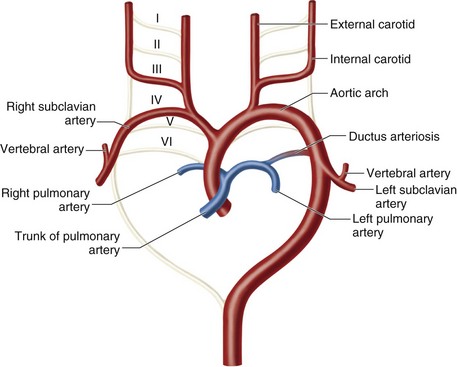
 FIGURE 71-9
FIGURE 71-9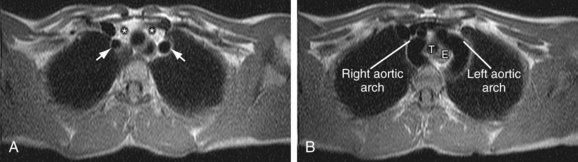
 FIGURE 71-10
FIGURE 71-10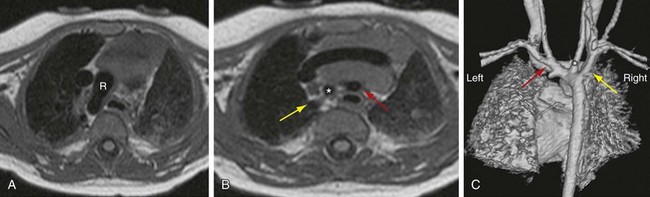
 FIGURE 71-11
FIGURE 71-11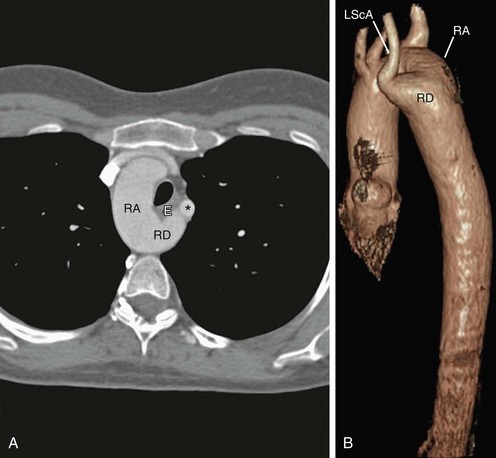
 FIGURE 71-12
FIGURE 71-12