Fig. 25.1
Lateral radiograph showing ossific density anterior to the distal humerus (published with kind permission. Copyright © Felix H. Savoie, III, MD)
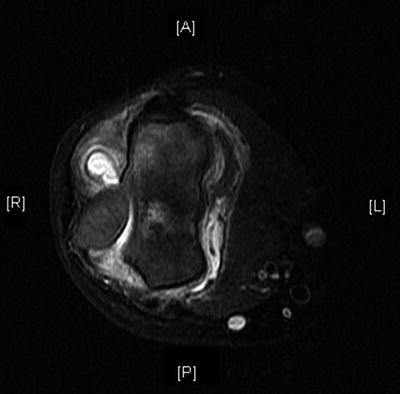
Fig. 25.2
Axial MRI view showing a large displaced capitellar fragment (published with kind permission. Copyright © Felix H. Savoie, III, MD)

Fig. 25.3
Sagittal MRI view of the displaced capitellar fragment (published with kind permission. Copyright © Felix H. Savoie, III, MD)
The patient was brought to the operating room and placed in the prone position after placement of an interscalene block and induction of general anesthesia. Examination under anesthesia showed posterolateral instability with stable medial structures. The range of motion showed poor pronation and supination with −30° of extension and flexion to 90°.
Arthroscopy was initiated with formation of a proximal anteromedial portal. A large, loose fragment of articular cartilage was seen in front of the radiocapitellar joint. A lateral portal was established to assist in evaluation. The cartilage piece was approximately 1.5 cm × 1.0 cm (Fig. 25.4), but unfortunately, there was no bone on the backside of the cartilage fragment. The piece was deemed irreparable and removed. Further arthroscopic evaluation showed arthrofibrosis involving the capsule. The capsule was incised from lateral to medial and resected. The capitellum was devoid of cartilage (Fig. 25.5) as was the central portion of the radial head (Fig. 25.6). These two areas were microfractured. Range-of-motion assessment now showed extension of 0°, flexion of 145°, and full pronation and supination. No pathology was seen posteriorly in the olecranon fossa. The medial gutter showed evidence of previous injury to the medial ulnar collateral ligament (MUCL) that appeared to be healing well. A positive “drive-through sign” on the lateral side confirmed lateral instability. In the lateral gutter, there was a second large osteochondral fragment of capitellum with ligaments attached that was separated from its base without evidence of healing. This piece can be seen on the MRI (Figs. 25.7 and 25.8). It was felt that this fragment warranted fixation. The area was debrided and microfractured. A bioabsorbable anchor with PDS® suture (Ethicon, Somerville, NJ) was placed. The PDS® was passed through the fragment and tied, securing the piece in its bed (Figs. 25.9, 25.10, and 25.11). A test of range of motion confirmed stable fragment fixation with maintenance of range of motion. The patient was placed into a splint in full extension and awoken from anesthesia.
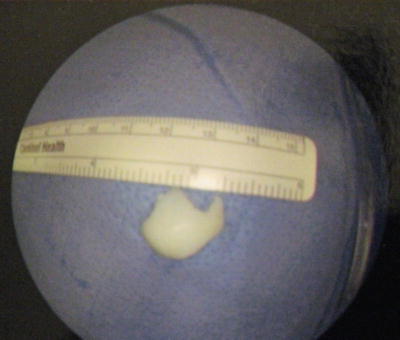
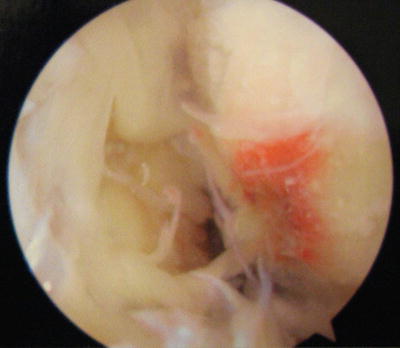
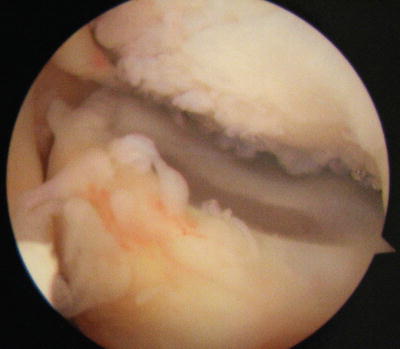
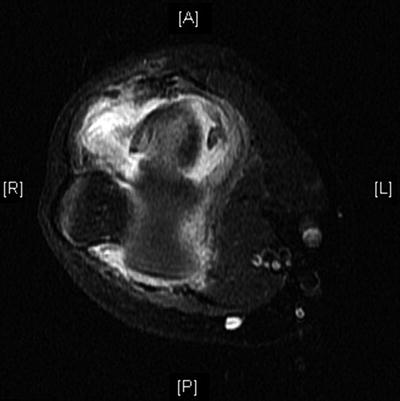

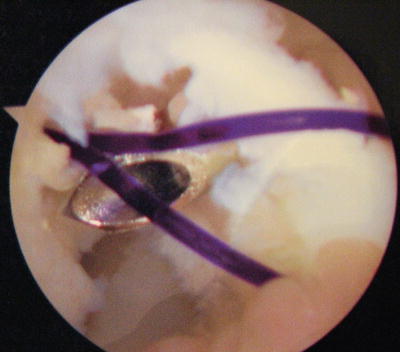
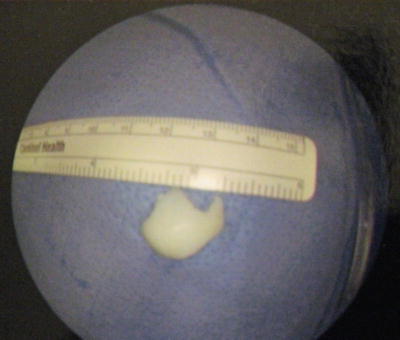
Fig. 25.4
Arthroscopic view of the capitellar cartilage fragment. The fragment did not have any bone on its backside and was deemed to be irreparable (published with kind permission. Copyright © Felix H. Savoie, III, MD)
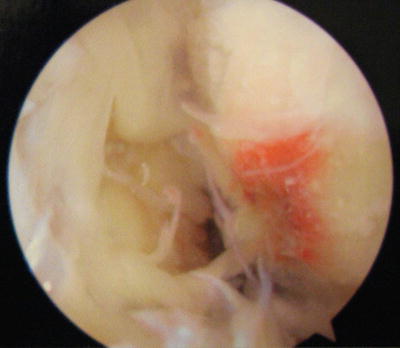
Fig. 25.5
Arthroscopic view of the capitellum devoid of cartilage (published with kind permission. Copyright © Felix H. Savoie, III, MD)
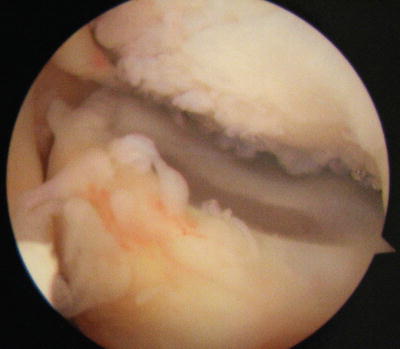
Fig. 25.6
Arthroscopic view again showing the bare capitellum and the central portion of the radial head without cartilage coverage (published with kind permission. Copyright © Felix H. Savoie, III, MD)
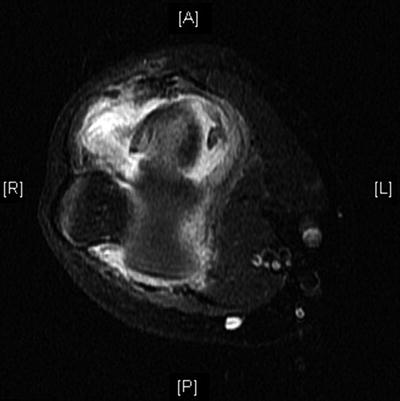
Fig. 25.7
Axial MRI view of the smaller capitellar fragment that had the lateral ligaments attached to it (published with kind permission. Copyright © Felix H. Savoie, III, MD)

Fig. 25.8
Coronal MRI view of the smaller fragment that had the lateral ligaments attached to it (published with kind permission. Copyright © Felix H. Savoie, III, MD)
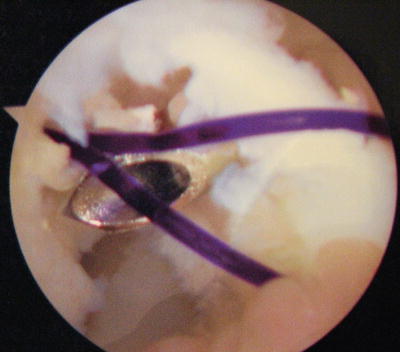
Fig. 25.9




Arthroscopic view of the repair. The anchor can be seen at the tip of the spinal needle. The nonabsorbable suture that the anchor was preloaded with has been replaced by PDS® suture (published with kind permission. Copyright © Felix H. Savoie, III, MD)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








