Condition
Physical exam signs
Cervical radiculopathy and/or neuroforaminal stenosis
Cervical range of motion and Spurling’s maneuver
AC joint osteoarthritis or distal clavicle osteolysis
Cross body adduction and acromioclavicular (AC) tenderness
Abnormal scapular position or motion
Scapular dyskinesia or scapular winging
SLAP tear
Active compression (O’Brien’s) test
Anterior instability
Apprehension/relocation/load and shift
Subacromial impingement
Hawkins’/Neer’s signs
Multidirectional instability
Sulcus sign, load and shift
Biceps tenosynovitis
Speed and Yergason’s test, palpation of long head biceps tendon
Glenohumeral internal rotation deficit
Decreased abducted internal rotation with decreased total arc of motion
Thoracic outlet syndrome
Adson’s test (diminished pulse with forward elevation and neck rotation)
Rotator cuff tendonitis/rotator cuff tear/suprascapular neuropathy (partial or full)
Direct rotator cuff strength testing
MRI Findings in the Throwing Shoulder
MRI is commonly ordered in the injured or dysfunctional throwing shoulder to evaluate the presence or absence of structural damage as well as the extent of the damage. Conventional MRI and MR arthrography can be used to evaluate the disabled throwing shoulder. There is some evidence that MRI arthrography is more sensitive in the diagnosis of both labral tear and partial thickness rotator cuff tears [21, 22]. MRI is taken in standard coronal/sagittal/axial views; in addition, MR arthrography in the abducted external rotated position has been advocated in the overhead athlete as an effective adjunct to identify partial thickness rotator cuff tears [23, 24].
A systematic approach to evaluate the MRI in the throwing athlete is critical. It is common for multiple areas of pathology to be present (e.g., SLAP tear and partial thickness rotator cuff tear). Interpretation of the rotator cuff images should include an evaluation of not only the tendon and tendon insertion but also the muscle belly to document the presence or absence of atrophy. Evaluation of the labrum is obviously centered on evaluating the superior labrum, biceps anchor, and long head biceps tendon. However, the labrum should be inspected on MRI circumferentially as superior labral tears can extend both anteriorly and posteriorly. MRI should also be used to evaluate acromial morphology, the AC joint, glenohumeral articular cartilage, and surrounding structures to ensure proper diagnosis of concomitant pathology.
Case 1: Superior Labral Tear with Posterosuperior Paralabral Cyst
A 19-year-old collegiate water polo player with 12 months of low-grade shoulder pain presented with an acute exacerbation of pain in his dominant right shoulder after a game. He reported an inability to throw hard and a feeling of a dead-arm.
The patient had normal cervical spine exam and a negative Spurling’s maneuver. He had no tenderness to palpation over the AC joint but mild tenderness to palpation over the biceps tendon. Inspection revealed no muscle atrophy or scapular winging. Strength was 5/5 throughout except for slight (5−/5) weakness with external rotation in the dominant shoulder. Range of motion was full, and there was no glenohumeral internal rotation deficit. Provocative testing revealed negative apprehension/relocation testing, 2+ load and shift anteriorly/1+ load and shift posteriorly (symmetric to left shoulder), and positive active compression (O’Brien’s test) with relief of symptoms with supination of the hand. Speed’s and Yergason’s tests were negative, as were Neer and Hawkins’ tests.
Due to the duration and severity of the symptoms, plain radiographs and MRI arthrography were performed. Plain radiographs were unremarkable. MRI arthrography revealed a type 2 superior labral tear with multiloculated posterosuperior labral cyst just superior to the spinoglenoid notch (Fig. 16.1a–d). Anterior labrum, posterior labrum, and rotator cuff were intact.
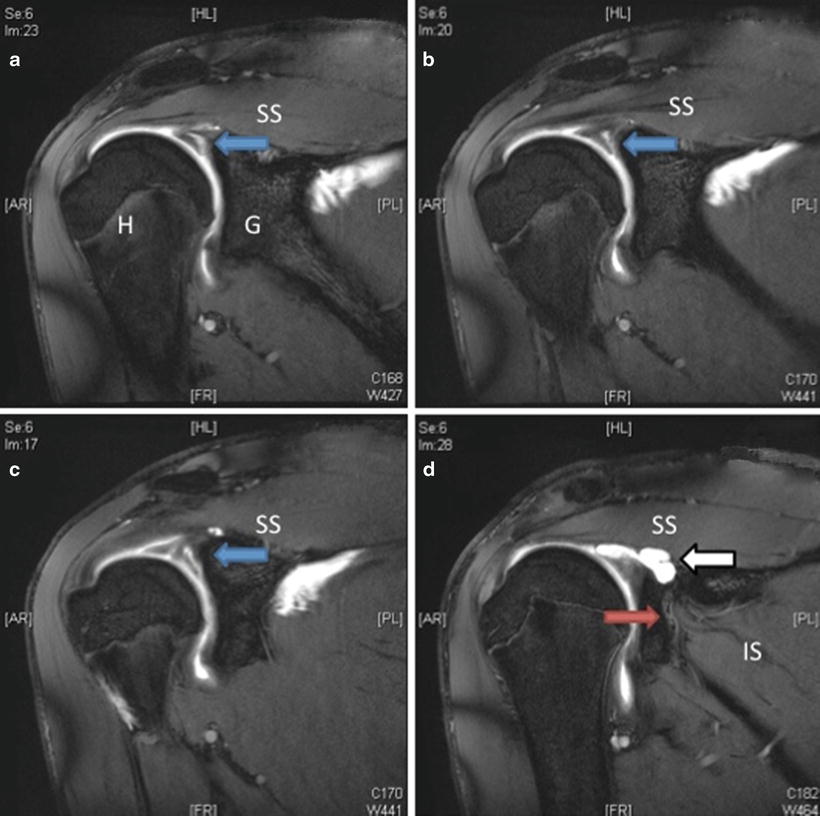
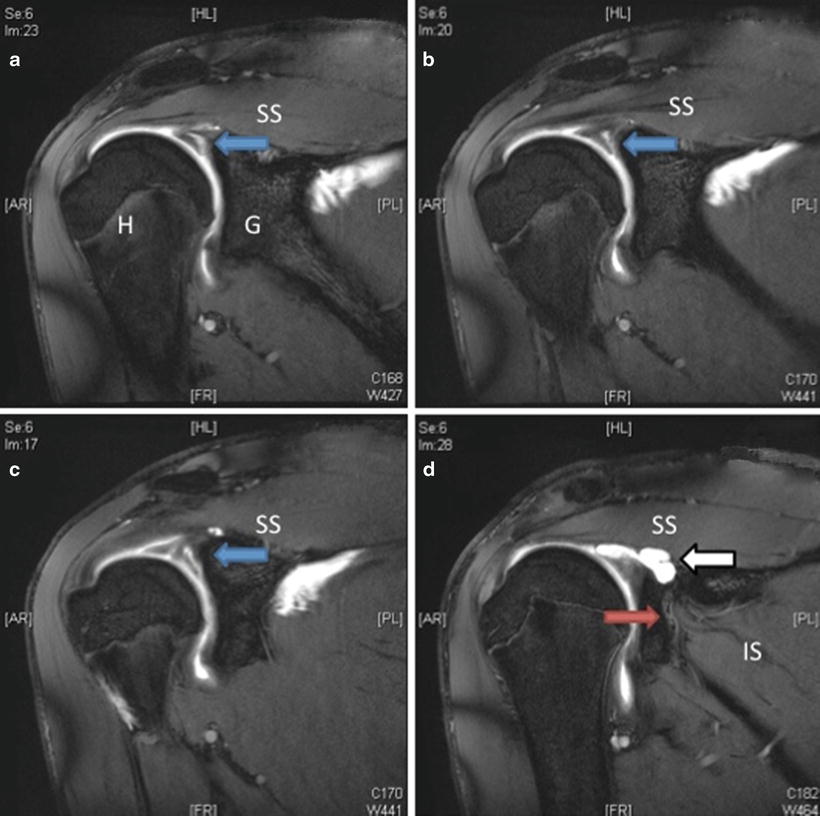
Fig. 16.1
Coronal T1-fat suppressed MR arthrography images reveal intact rotator cuff and significant superior labral tearing (a–c) with contrast extending under and within the superior labrum (blue arrows). In addition, a spinoglenoid notch cyst (d) was present at the posterior aspect of the superior glenoid (white arrow). This cyst effaced the suprascapular neurovascular bundle (red arrow) as it exits the spinoglenoid notch toward the infraspinatus. H humerus, G glenoid, SS supraspinatus, IS infraspinatus
The patient failed 6 weeks of conservative treatment that included rest, physical therapy, and NSAIDs and was still unable to throw or swim comfortably after an attempted return to play.
Arthroscopic surgery was recommended (Fig. 16.2a–f). At the time of surgery, diagnostic arthroscopy revealed intact biceps tendon, type 2 superior labral tear (10:00–12:00) with a small, displaced flap of labrum, intact posterior and anterior labrum, intact glenohumeral cartilage, and normal supraspinatus/infraspinatus/subscapularis.
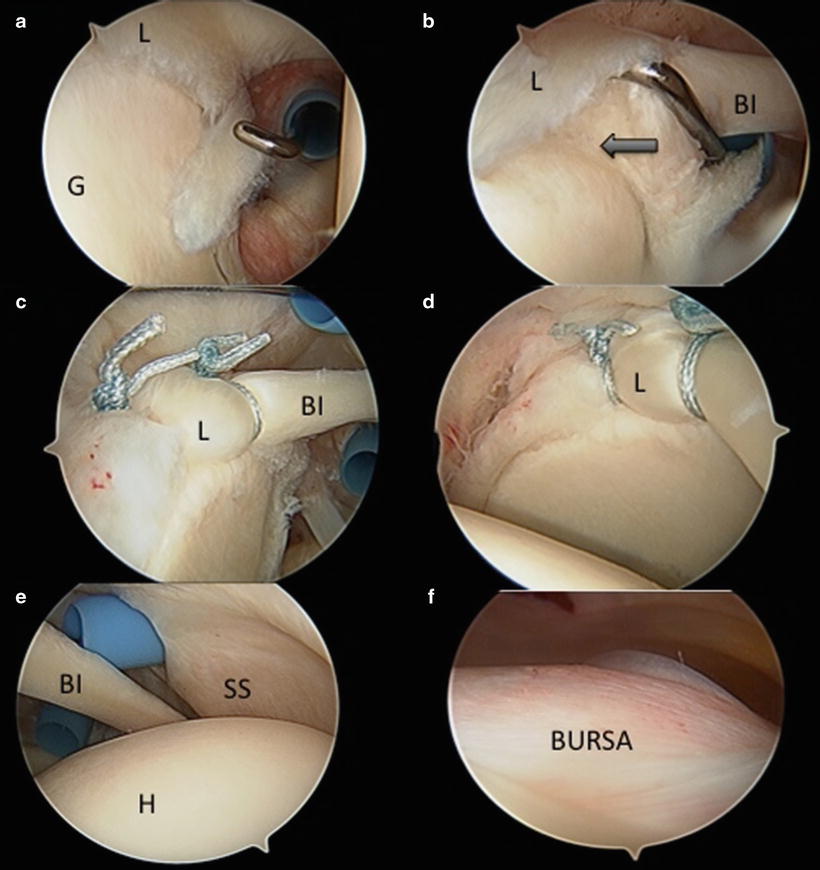
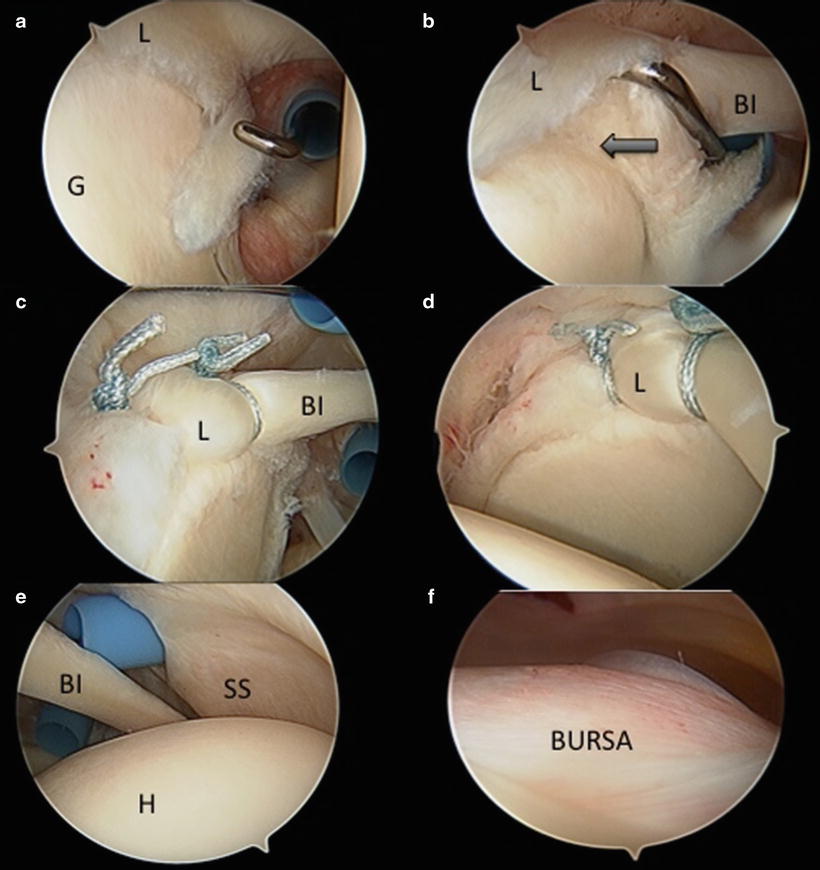
Fig. 16.2
(a–f) Arthroscopic images. (a) Probe demonstrates small interposed labral flap. (b) Probe demonstrates type 2 SLAP tear from 10:00 to 12:00 (black arrow). (c) Superior labral repair with two suture anchors viewed from the posterior portal. (d) Repair viewed from the anterosuperior portal. (e) Pristine articular supraspinatus. Note the low rotator interval portal (working) and the high lateral rotator interval just anterior to the supraspinatus above the biceps tendon (used for anchor placement). (f) Normal subacromial space and subacromial bursa. L labrum, G glenoid, H humerus, BI biceps, SS Supraspinatus
Two working portals were established. The paralabral cyst was entered and debrided with a 3.5 mm shaver through the posterior extent of the tear. The superior labral repair was accomplished using two 2.4 mm bioabsorbable suture anchors with sutures tied in a simple fashion. The subacromial space was pristine.
Postoperatively, immobilization was 3 weeks. Passive range of motion was permitted. Full range of motion was restored at 10 weeks. Strengthening was permitted at 12 weeks. Throwing program was initiated at 18 weeks. Successful return to competition was accomplished at 6 months. The patient subsequently competed for 2 years in collegiate water polo.
Discussion
While early results in the throwing athlete were very promising after the arthroscopic repair of SLAP lesions [25, 26], more recent literature reporting outcome scores more sensitive for overhead activity have tempered the enthusiasm for labral repair in the throwing athlete; return to previous level of activity may not be as high as once thought [27–29]. Brockmeier et al. showed that acute traumatic SLAP tears may be better candidates for surgery with better short-term results [30]. A study by Provencher et al. revealed a high rate of continued pain after SLAP repair in the military population sometimes leading to reoperation [27]. In addition, there is evidence that older athletes with SLAP tears may be better served with biceps tenodesis [31] and that SLAP tears can possibly be ignored in the setting of rotator cuff repair [32, 33]. Certainly good to excellent outcomes can be obtained with SLAP repair in the overhead athlete, but recent literature suggests following a conservative course and ensuring the athlete have realistic expectations following surgery.
Case 2: Internal Impingement with SLAP Tear and Partial Thickness Rotator Cuff Tear
A 27-year-old former junior college baseball player who now plays recreational softball complains of years of right shoulder pain. He has found it difficult over the last 12 months to throw. He complains of posterior shoulder pain in the cocking phase of his throwing motion. He reports no trauma in the shoulder but does report a history of successful cortisone injections to his shoulder years ago.
The patient had normal cervical spine exam and a negative Spurling’s maneuver. He had no tenderness to palpation over the AC joint but mild tenderness to palpation over the biceps tendon. Inspection revealed no muscle atrophy or scapular winging. Strength was 5/5 throughout. Range of motion was full in forward elevation bilaterally, but there was a glenohumeral internal rotation deficit of 20°. Abducted external rotation in the right shoulder was 105°; abducted internal rotation in the right shoulder was 35°. Abducted external rotation in the left shoulder was 95°; abducted internal rotation in the left shoulder was 65°. Provocative testing revealed negative apprehension/relocation testing, 1+ load and shift anteriorly/1+ load and shift posteriorly (symmetric to left shoulder), and positive active compression (O’Brien’s test) with relief of symptoms with supination of the hand. Speed’s and Yergason’s tests were negative. Neer and Hawkins’ tests were slightly positive.
Plain radiographs revealed a type 2 acromion and early AC joint osteoarthritis but were otherwise negative.
Because he had success with a corticosteroid injection in the past, a subacromial injection was prescribed; this partially relieved his baseline shoulder pain over the next several weeks. A course of physical therapy was prescribed to include restoration of right shoulder internal rotation using sleeper stretches. The patient returned to softball but still had pain while throwing. Due to the duration and severity of the symptoms, MRI arthrography was performed. MRI arthrography revealed a small posterosuperior labral tear. In addition, contrast was observed in a delaminated partial thickness articular sided rotator cuff tear in the posterior supraspinatus (Fig. 16.3a–d). Anterior labrum and posterior labrum were intact, but there was MRI evidence of subacromial impingement.
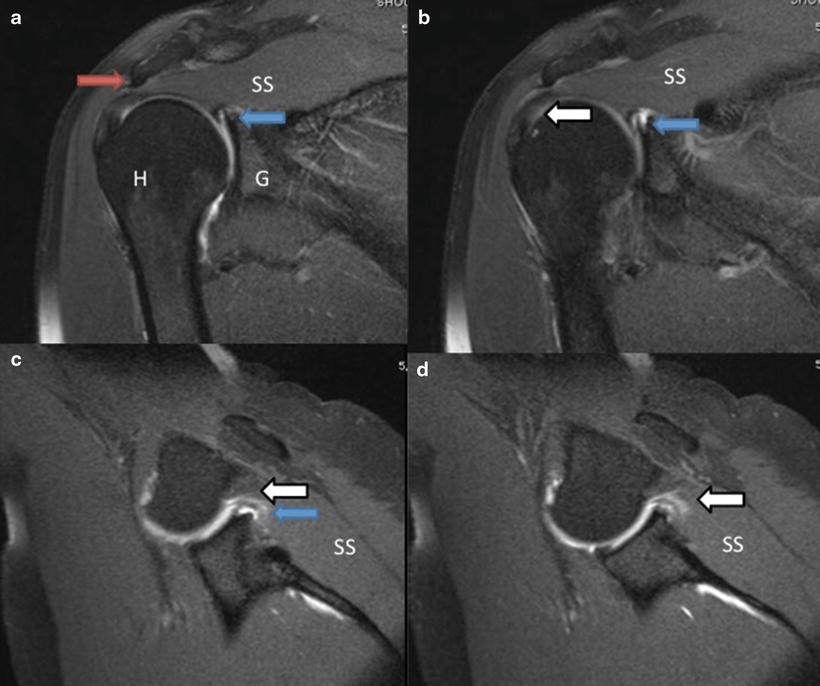
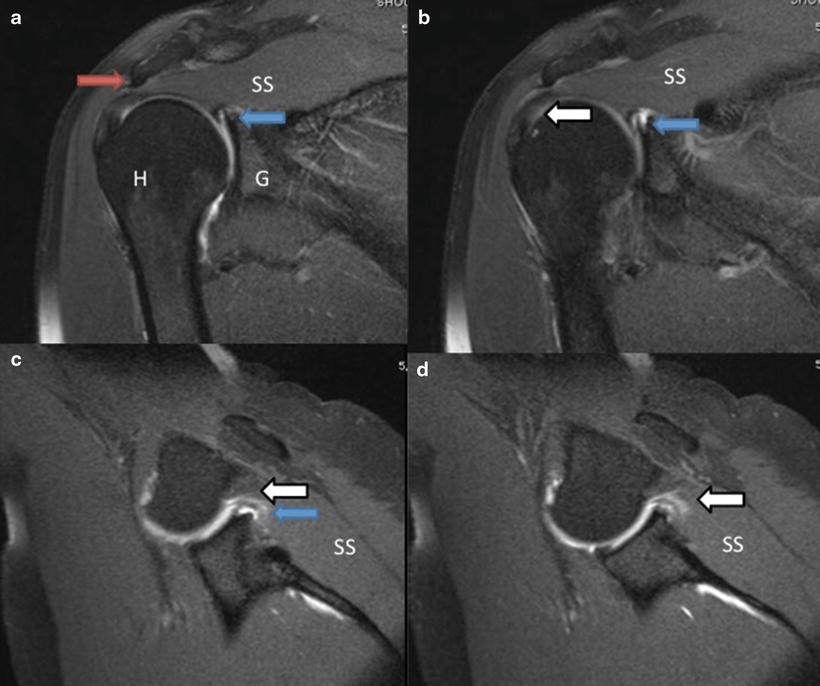
Fig. 16.3
(a–d) Coronal T1-fat suppressed MR arthrography images reveal downsloping acromion (red arrow). The rotator cuff was largely intact but with some high signal in the articular surface of the posterior supraspinatus (white arrow in b). There was superior labral tearing (blue arrows in a–c) with contrast extending under and within the superior labrum. The ABER views (c, d) revealed contact of the rotator cuff with the superior glenoid. In addition, contrast was observed in a delaminated partial thickness articular sided rotator cuff tear in the posterior supraspinatus (white arrows c, d). H humerus, G glenoid, SS supraspinatus
The patient elected to undergo arthroscopic surgery (Fig. 16.4a–f). At the time of surgery, diagnostic arthroscopy revealed intact biceps tendon and a peel-back type 2 superior labral tear (9:30–10:30) with an Ellman grade 1A partial thickness articular sided rotator cuff tear in the posterior aspect of the supraspinatus. There was intact posterior and anterior labrum, intact glenohumeral cartilage, and normal infraspinatus/subscapularis. Contact between the rotator cuff tear and posterosuperior labrum was observed in the abducted-externally rotated position at the time of arthroscopy.
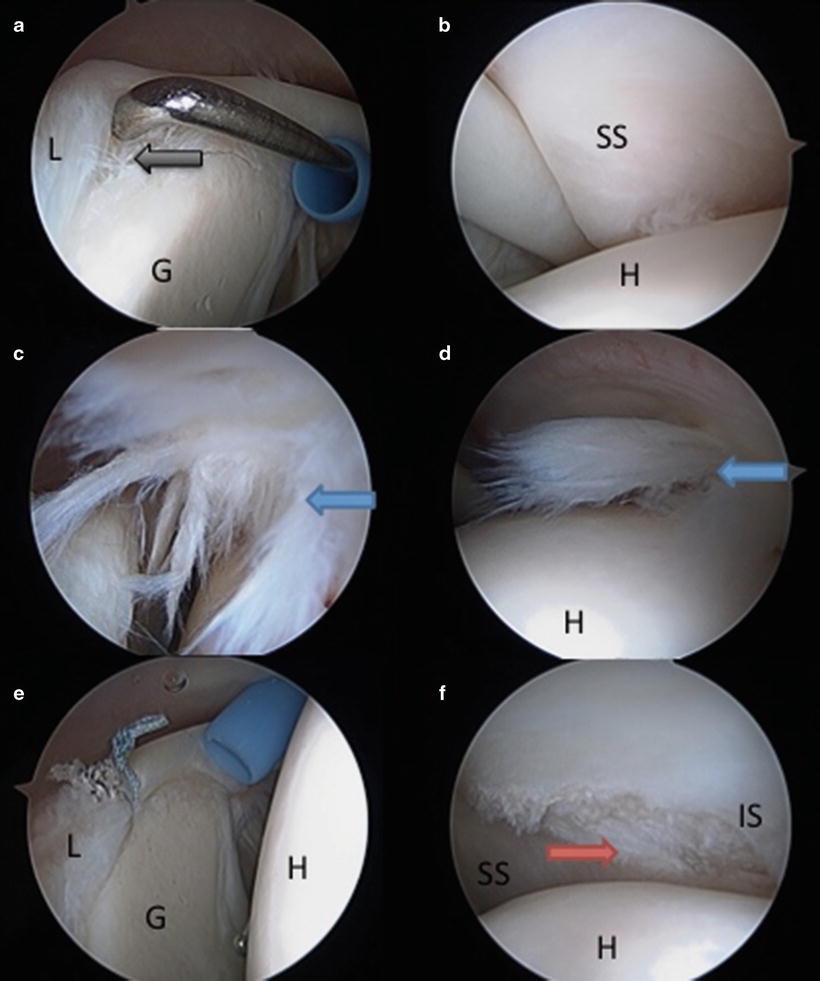
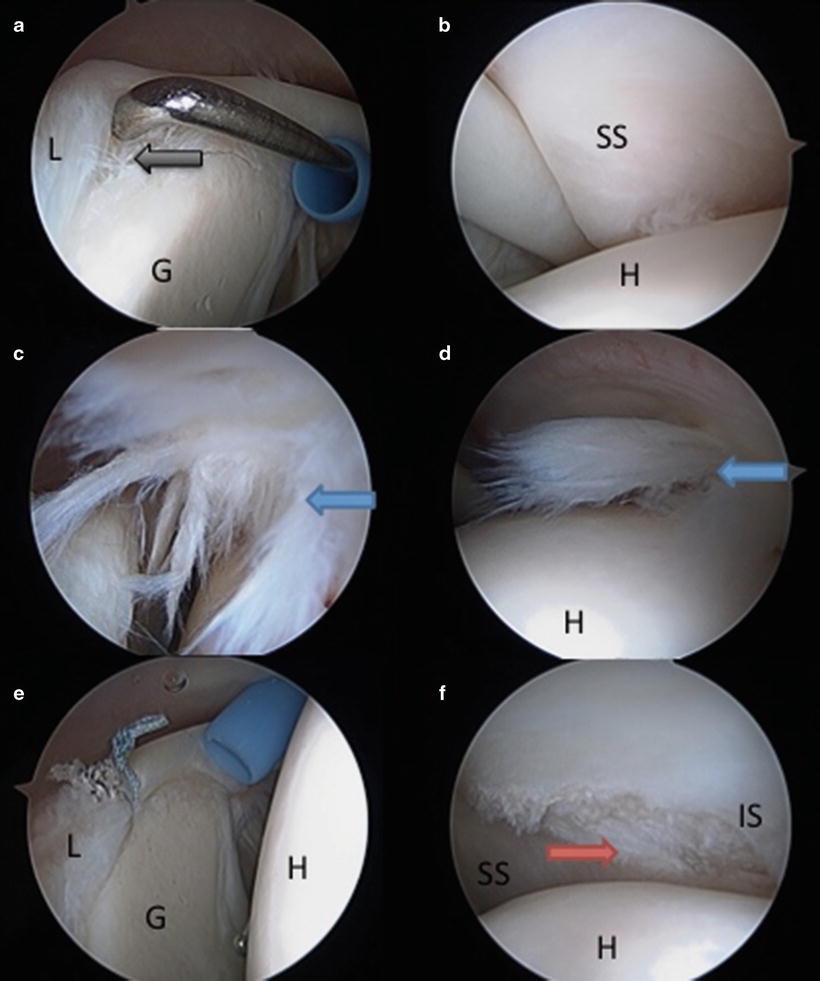
Fig. 16.4




(a–f) Arthroscopic images. (a) Probe demonstrates a small peel-back type 2 superior labral tear (9:30–10:30) (black arrow). (b) Intact supraspinatus. (c) ABER position arthroscopically reveals contact between torn articular side of supraspinatus and posterosuperior glenoid. (d) Partial articular sided rotator cuff tear viewed with the arm in the neutral, adducted position. (e) Superior labral repair with a single anchor, double loaded suture. (f) After debridement of the rotator cuff to stable tissue, no repair of the rotator cuff was performed. L labrum, G glenoid, H humerus, BI biceps, SS supraspinatus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree