Fig. 12.1
(a) The anterior labrum was detached from approximately 6 o’clock to 11 o’clock and was folded and inverted medially and inferiorly. (b) The labrum is outlined in yellow after being freed from the glenoid rim and scapular neck. (c) Arthroscopic view of medium-sized Hill–Sachs lesion. (d) T2 fat-suppressed oblique coronal left shoulder MR arthrogram. The anteroinferior labrum (arrow) is abnormal in signal and folded, inverted, and flipped medially and inferiorly in respect to the glenoid. (e) T2 fat-suppressed oblique sagittal left shoulder MR arthrogram. There is abnormal T2 signal involving the anteroinferior labrum which is folded, inverted, and flipped medially and inferiorly in respect to the glenoid (arrow). (f) T2 fat-suppressed axial left shoulder MR arthrogram. There is marrow edema surrounding a moderate-sized well-defined impaction fracture of the posterolateral humeral head
Arthroscopy
The patient was taken to the operating room and placed in the lateral decubitus position. A standard diagnostic arthroscopy of the right shoulder was completed. Arthroscopic findings demonstrated a medium-sized Hill–Sachs lesion (Fig. 12.1c). The anterior labrum was detached from approximately 6 o’clock to 11 o’clock and was folded and inverted medially and inferiorly (Fig. 12.1a, b). There was a split in the labrum and capsule inferiorly and the labrum was split superiorly. The posterior labrum was normal. The biceps anchor and tendon were normal. The rotator cuff tendons were normal.
To repair this injury, the anterior capsulolabral complex was mobilized from the glenoid rim and scapular neck. The glenoid rim and scapular neck were abraded with an arthroscopic shaver to create a bleeding bony surface. The inferior capsular split was repaired with a #2 high-strength, polyethylene core suture passed with a suture lasso. The labrum was then repaired back to the glenoid rim using three 2.4 mm biocomposite suture anchors. The sutures were passed using a suture lasso and then tied in a simple fashion arthroscopically. Superiorly, the labrum and capsule were repaired utilizing the two suture limbs from the anchor. This resulted in stable repair of the labrum and restoration of the normal tension within the inferior glenohumeral ligament complex (Fig. 12.2a, b).
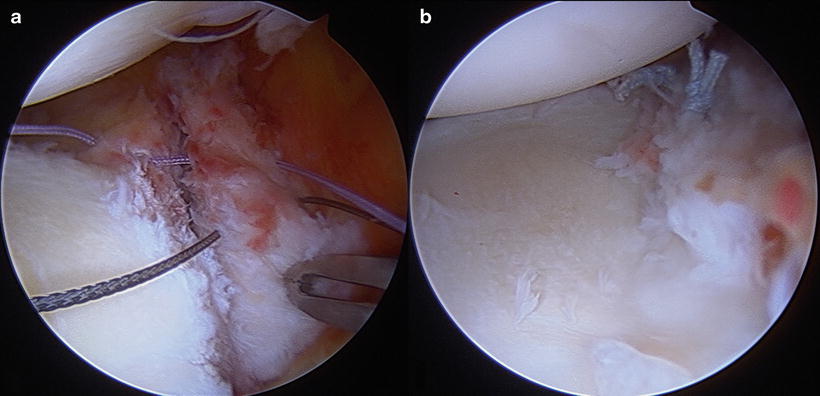
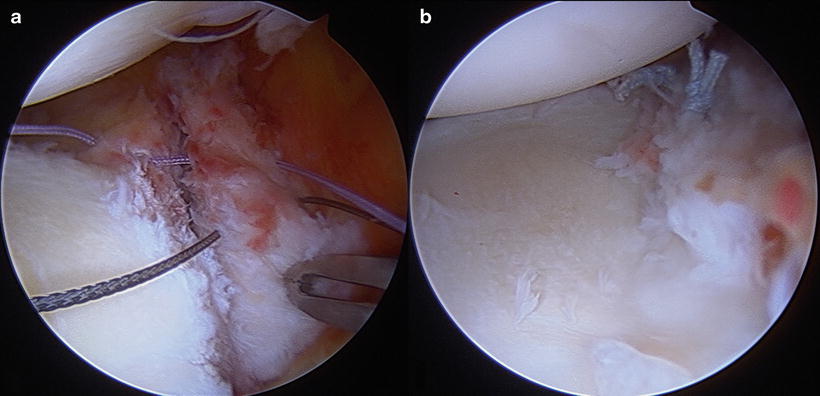
Fig. 12.2
(a) Suture passing through the labrum. (b) Stable repair construct
Discussion
This case illustrates the importance of careful MRI and arthroscopic evaluation. The inverted labrum was not initially appreciated on MRI. It was not until further evaluation that the labrum was found to be inverted and scarred to the glenoid rim and scapular neck.
There are two variants of the soft tissue Bankart lesion, Perthes and ALPSA. In a Perthes lesion the scapular periosteum remains intact and is stripped medially. In the anterior labroligamentous periosteal sleeve avulsion (ALPSA), the anterior scapular periosteum is not disrupted. This allows the capsulolabral complex to displace medially and rotate inferiorly on the scapular neck. In the case of an ALPSA lesion, the capsulolabral junction scars medially on the scapular neck. In the Perthes and Bankart lesions, the capsulolabral complexes do not displace medially [5]. This distinction is important when determining the anatomy on MRI and arthroscopically. It is also important to distinguish with regard to patient outcomes. Reports for recurrent instability after arthroscopic repair of an ALPSA lesion are twice as high compared with Bankart lesions [4, 6].
Case 2: GLAD
History/Exam
The patient is a 28-year-old right-hand-dominant male who injured his right shoulder when falling forward during a landing while skydiving. He presented to the clinic 5 weeks after this injury due to persistent right shoulder pain. He did not describe a dislocation or subluxation.
Physical exam in the clinic revealed range of motion: forward elevation 145°, external rotation 50°, internal rotation T10, and IGHE 90°. Provocative maneuvers included anterior apprehension, posterior apprehension, and 1+ anterior drawer, with an otherwise normal exam.
At the time of surgery his exam under anesthesia revealed 145° of forward elevation, 80° of external rotation in abduction, 40° of internal rotation, and 75° of external rotation with the arm at the side. There was a 1+ anterior load shift and a 1+ posterior load shift. There was a 0.5 cm sulcus sign in internal rotation, neutral rotation, and external rotation.
Imaging
Initial right shoulder radiographs of the patient were unremarkable. The patient then underwent an MR arthrogram of the right shoulder with axial and oblique coronal fat-saturated T1- and T2-weighted imaging and oblique sagittal T1-, fat-saturated T1-, and fat-saturated T2-weighted imaging. MR demonstrated a partial tear of the anteroinferior labrum with a focal chondral defect at the 4–6 o’clock position consistent with a glenolabral articular disruption (GLAD)-type lesion shown in Fig. 12.3d, e. There was also degenerative fraying of the posterosuperior labrum (not shown).
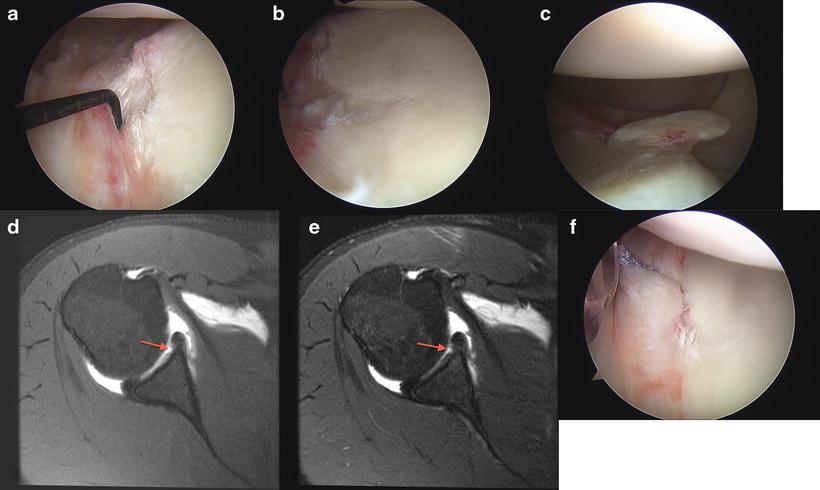
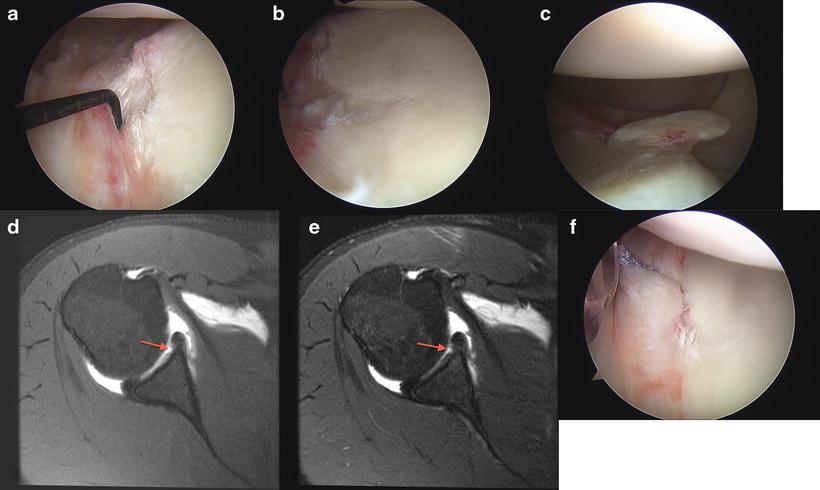
Fig. 12.3
(a) Detachment of the anterior labrum associated with the GLAD lesion. (b) Articular cartilage defect associated with GLAD lesion. (c) Articular cartilage flap flipped into the axillary pouch. (d) Axial T1 fat-suppressed right shoulder MR arthrogram. There is a focal chondral defect involving the anteroinferior glenoid. There is faint signal abnormality extending into the anteroinferior labrum consistent with a partial tear. (e) Axial T2 fat-suppressed right shoulder MR arthrogram. There is a focal chondral defect involving the anteroinferior glenoid. There is faint signal abnormality extending into the anteroinferior labrum consistent with a partial tear. (f) Suture was passed through the labrum and tied reapproximating the labrum into the defect resulting in stable fixation
Arthroscopy
The patient was taken to the operating room and placed in the lateral decubitus position. A standard diagnostic arthroscopy of the right shoulder was completed. This demonstrated normal glenoid and humeral articular cartilage in the areas away from the lesion. The biceps tendon and rotator cuff tendons were normal. The posterior labrum had some fraying but was intact in a meniscoid configuration. The anterior–inferior labrum had an articular cartilage and labral flap that was flipped into the axillary pouch (Fig. 12.3b, c). There was a partial detachment of the anterior labrum associated with this GLAD lesion (Fig. 12.3a). There was no sublabral hole.
With an arthroscopic shaver, the flap of the articular cartilage and anterior–inferior labrum was resected. The remaining defect in the anterior–inferior articular cartilage of the glenoid as well as detachment of the labrum was further explored. We elected to repair the anterior–inferior labrum into the glenoid defect. A single 3.0 mm PEEK suture anchor was placed into the defect. Suture was passed through the labrum which was then tied reapproximating the labrum into the defect resulting in stable fixation (Fig. 12.3f).
Discussion
With GLAD lesions the articular cartilage defect can be subtle and often missed on imaging. A high index of suspicion is needed to appreciate the articular cartilage defect. Additionally, the piece of cartilage from the defect can occasionally be seen as in Fig. 12.3b, c. It is important to identify the articular cartilage lesion to prepare for possible micro-fracture or other treatment that may be necessary at the time of arthroscopy.
Case 3: Bankart
History/Exam
The patient is a 34-year-old left-hand-dominant male who sustained a traumatic right shoulder dislocation approximately 1 year prior to presentation during a paint ball match. He subsequently had four dislocations. His most recent dislocation was from sneezing, but he was able to relocate his shoulder within a few minutes.
Physical exam in the clinic revealed a normal range of motion with no generalized laxity. Provocative maneuvers included anterior apprehension and anterior relocation, 1+ load and shift (anterior), and 1+ load and shift (posterior) with a 1+ sulcus (neutral).
At the time of surgery his exam under anesthesia revealed 150° of forward elevation, 90° of external rotation in abduction, 30° of internal rotation, and 30° of external rotation with the arm at the side. There was a grade 2 anterior load shift and a grade 2 posterior load shift. There was 0 cm of inferior humeral head translation in internal rotation and 0 cm in external rotation.
Imaging
Initial shoulder radiographs were unremarkable for fracture or dislocation. A complete MRI arthrogram of the shoulder with axial, oblique, sagittal, and oblique coronal fat-suppressed T2 FSE sequences as well as oblique sagittal T1-weighted sequence was obtained. The MRI arthrogram demonstrated irregularity/partial detachment of the anteroinferior labrum with possible scarring consistent with a labral Bankart lesion (Fig. 12.4e). In addition, there was increased marrow signal in the posterolateral humeral head consistent with a small Hill–Sachs impaction fracture (Fig. 12.4d).
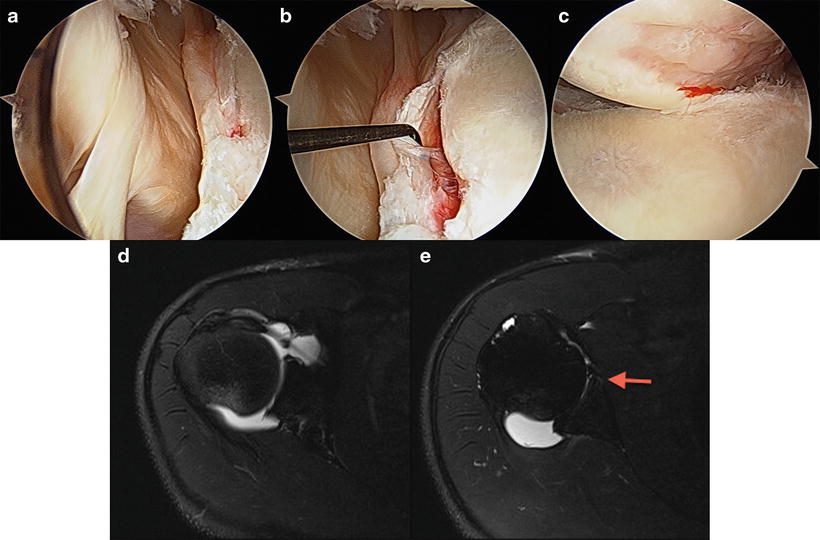
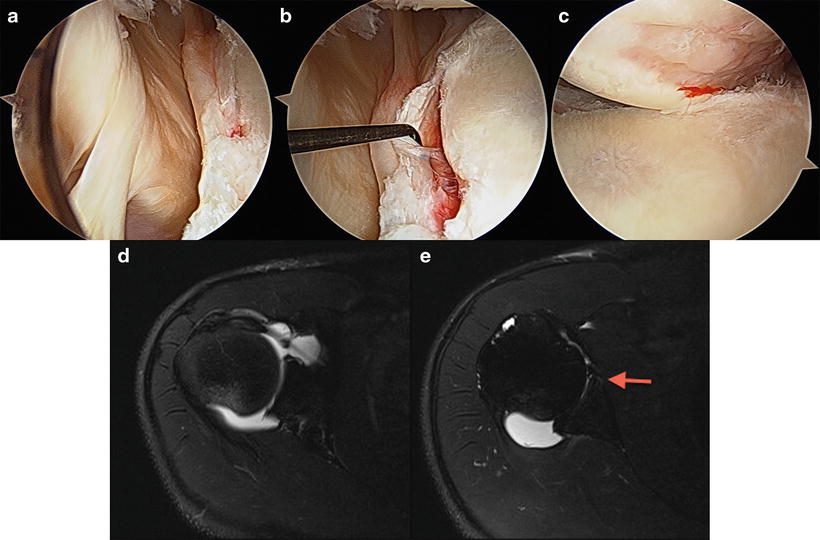
Fig. 12.4




(a, b) The anterior labrum was detached from approximately 1 o’clock to 5 o’clock. (c) Medium-sized Hill–Sachs. (d) Axial T2 fat-suppressed right shoulder MR arthrogram. There is abnormal flattening of the posterolateral humeral head with associated increased marrow signal consistent with a Hill–Sachs impaction fracture. (e) Axial T2 fat-suppressed right shoulder MR arthrogram. There is abnormal T2 signal between the glenoid and the anteroinferior labrum consistent with a labral Bankart lesion (arrow)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree