Fig. 31.1
Illustration depicting anterior and posterior views of the ligamentous constraints of the hip. The iliofemoral and pubofemoral ligaments can be seen anteriorly, and the ischiofemoral ligament can be seen posteriorly
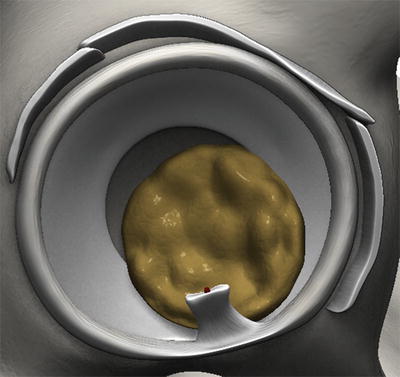
Fig. 31.2
Illustration showing the orientation of the ligamentum teres relative to the acetabular labrum. Note the significant increase in acetabular depth produced by the labrum
The etiologies of hip instability are most often conceptually divided into traumatic and atraumatic causes.
Most cases of acute traumatic dislocation occur when a sudden, excessive axial load is applied to the femur with the hip in a flexed position—this type of injury may or may not result in fracture of the posterior wall of the acetabulum [10, 11]. Some athletes may be predisposed to have an acute dislocation as a manifestation of chronic overuse [12, 13]. Although specific injury patterns following acute dislocations have not been well described, concomitant injuries to the articular surface, ligamentum teres, acetabular labrum, and capsuloligamentous structures may result in symptoms of recurrent, painful microinstability [11].
Atraumatic hip instability has numerous potential etiologies. Congenital defects involving bone or soft tissues, multiligamentous laxity, certain systemic diseases, or any one of several acquired causes such as previous open or arthroscopic hip surgery may predispose an individual to develop chronic, atraumatic hip instability which can be debilitating [14]. In most adults, true hip dislocations are uncommon without significant trauma or previous surgery. On the other hand, dislocations in children are more often associated with congenital malformations, such as torticollis and talipes equinovarus [15], that may lead to developmental abnormalities of the hip with a high potential for long-term sequelae including degenerative osteoarthritis and/or femoroacetabular impingement.
Developmental dysplasia of the hip (DDH) is a frequently cited entity associated with atraumatic hip instability that has yet to be clearly defined in the literature. As a result, published research related to DDH can be confusing and often conflicting. Nevertheless, DDH is generally considered to be a continuum of pathologies with various morphologic features ranging from normal hip development to gross abnormalities that can result in significant instability. Some of these features may include a shallow or underdeveloped acetabular fossa (a cause and effect of recurrent hip dislocations in children), an abnormally small head–neck offset, and an excessive chondral wear as a result of altered biomechanical shear forces across the articular surfaces (Fig. 31.3). The development of ultrasonographic screening programs for the detection of hip subluxations and dislocations in young children has provided a cost-effective avenue for early recognition and treatment of DDH, thus significantly reducing the morbidity and cost associated with known long-term sequelae.
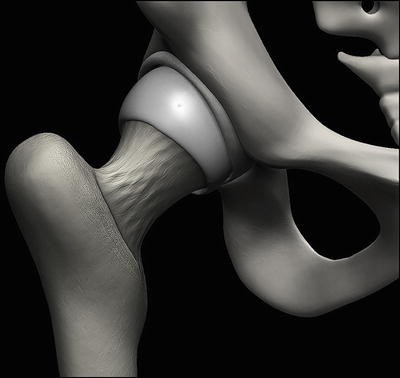
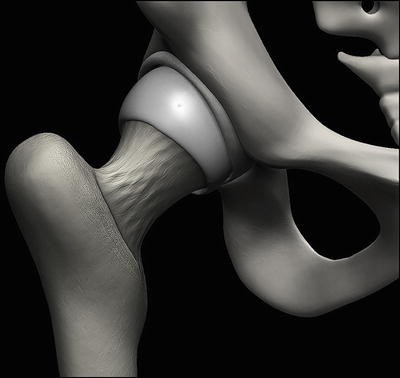
Fig. 31.3
Illustration depicting a dysplastic hip with a decreased head–neck offset and shallow acetabulum
In all patients, a thorough history is necessary to determine the circumstances associated with their reasons for seeking medical treatment and to develop a succinct, yet thoughtful, differential diagnosis that can be used to guide further management decisions. During the patient encounter, it is also important to obtain information regarding hip pathologies throughout the family history, especially inquiring about those pathologies that may be involved with the development of hip instability such as Ehlers–Danlos syndrome and Marfan syndrome. A documented history of instability involving other appendicular joints, such as the shoulder, may also be important in the diagnosis of multiligamentous laxity.
A complete assessment of gait, posture, and neurovascular function should be performed in all patients presenting with signs and/or symptoms of hip instability. In addition, palpation of relevant landmarks should also be undertaken to identify potential sources of pain. Range of motion should always be tested bilaterally to assess capsular laxity and to potentially reproduce the patient’s symptoms. Mechanical crepitation, snapping, or popping with range-of-motion testing may suggest the presence of a labral tear or flap, a chondral defect with or without an intra-articular loose body or snapping hip, especially when these sounds are associated with pain and apprehension.
There are numerous provocative maneuvers that can be performed to help solidify the differential diagnosis. For capsular laxity, the posterior impingement test and dial test are particularly useful. The posterior impingement test is performed by gently extending and externally rotating the hip with the patient supine. Reproduction of pain or apprehension with this maneuver suggests that posterosuperior osseous impingement may be the result of anterior capsular laxity [16]. Safran et al. demonstrated that the posterior impingement test may also be helpful in identifying abnormal stresses across the anterolateral labrum [17]. A positive test can also occur in patients with normal joint laxity; however, these patients often have abnormal skeletal morphology (e.g., coxa profunda). The dial test is performed by first passively internally rotating the affected hip. The limb is then released which allows the hip to externally rotate back toward the neutral position. Capsular laxity may be suspected when the extremity passively externally rotates >45° from the midline in the axial plane and/or lacks a definitive end point [7]. Pain or apprehension with gentle limb traction and/or hyperexternal rotation may also be suggestive of capsular laxity.
Standard radiographic analysis includes an anteroposterior (AP) view of the pelvis and a lateral view of the affected hip. An additional Judet view and/or a false-profile view may be helpful to assess acetabular coverage in cases where clinical instability is suspected. The center-edge angle is used to objectively measure femoral head coverage by the acetabulum. Additional measurement can be made to assess the presence of dysplasia (Table 31.1). In some cases, a traction view may be necessary to identify a “vacuum sign” which is often indicative of increased inferior capsular distraction.
Table 31.1
Radiographic signs of dysplasia
Signs of dysplasia | Measurement | Definition |
|---|---|---|
Tonnis angle >10° (Tonnis 1999) | Acetabular inclination | Angle of the horizontal line of the pelvis and the line connecting the most lateral and most medial parts of the acetabular weight-bearing sourcil |
<25° (Wiberg 1939) | CE angle | Angle of a vertical line (in relation to the pelvis) and a line connecting the femoral head center |
>42° (Sharp 1961) | Sharp’s acetabular angle | Angle of a horizontal line of the pelvis connecting both teardrop signs and the line of the teardrop to the most lateral point of the acetabular articular surface |
<20° (Lequesne 1961) | Anterior center-edge angle (VCA) | Angle of a line connecting the center of both femoral heads and the one between the center of the femoral head and the anteriormost edge of the acetabulum articular surface |
Magnetic resonance imaging (MRI) is used to evaluate the patency of surrounding soft tissue structures such as the acetabular labrum, joint capsule, and associated ligaments in cases of either traumatic or atraumatic hip instability. MRI with or without arthrography also plays an important role in locating chondral defects and labral tears that may require surgical treatment. In addition, the alpha angle is measured on MRI to assess abnormal bony growth on the femoral head–neck junction. Femoroacetabular impingement related to capsular laxity can lead to secondary chondral injury [18].
Computed tomography (CT) is routinely performed after reduction of traumatic hip dislocations (1) to assess the adequacy of reduction, (2) to identify acetabular fractures that may not have been visible on initial radiographs, (3) to identify intra-articular loose bodies, and (4) to plan the subsequent surgical approach (if indicated). CT scanning is not often indicated in patients with atraumatic instability due to the lack of significant clinical benefit coupled with the risks associated with exposure to excessive radiation.
Case 1: Traumatic Hip Instability
History/Exam
A 16-year-old high school student with no previous surgical history was playing football after school when he was tackled from behind and suffered an acute posterior dislocation of his left hip. The patient was taken to the emergency room where the hip was immediately reduced approximately 1 h after the initial incident. After being sent home on crutches, the patient presented to our clinic several days later for further evaluation of the injury. On physical examination of his left hip, there were no signs of abrasions, open wounds, ecchymoses, or neurovascular injuries. Only limited range-of-motion testing was performed given the nature of the injury and his level of pain at the time of examination.
Imaging
Following reduction in the emergency room, standard AP and lateral radiographs of the left hip revealed intra-articular loose bodies and fractures of both the posterior wall of the acetabulum and the right ischial tuberosity (Fig. 31.4). CT scanning was then performed which confirmed the diagnosis of a posterior wall fracture with lateral displacement (size, 2.2 cm anteroposteriorly × 0.6 cm mediolaterally × 2.6 cm superoinferiorly). An osseous fragment of approximately 1.5 cm in diameter was also noted adjacent to the anterior aspect of the femoral head. An MRI scan was also obtained (Fig. 31.5a–d) in which an avulsion fracture of the right ischial tuberosity was discovered with 3.0 cm of inferior displacement. Additionally, posterior labral tear, large joint effusion, and extensive soft tissue edema were identified (Fig. 31.5a, b). Given the findings on history, physical examination, and diagnostic imaging, left hip arthroscopy with possible open reduction and internal fixation was performed the following day.

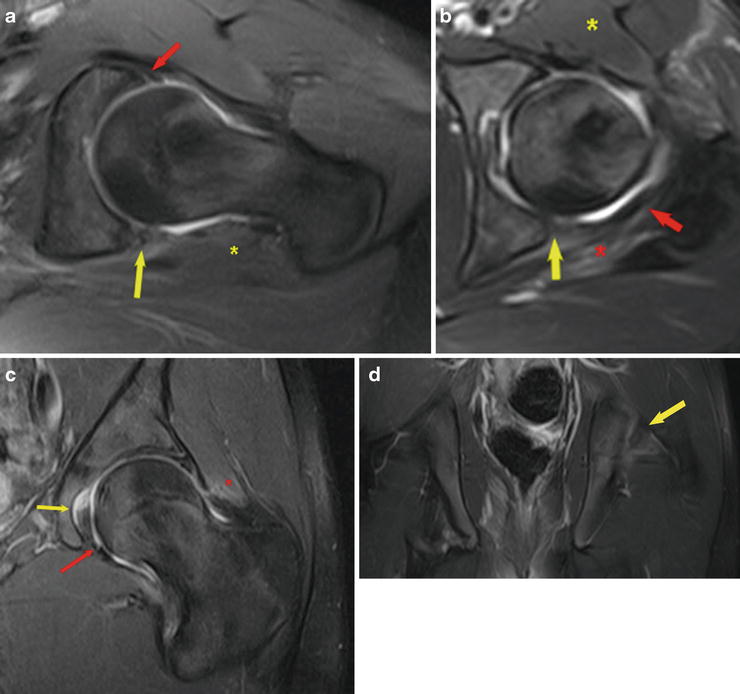

Fig. 31.4
AP radiograph following left hip dislocation showing posterior wall fracture on the left hip and an avulsion fracture of the right ischial tuberosity
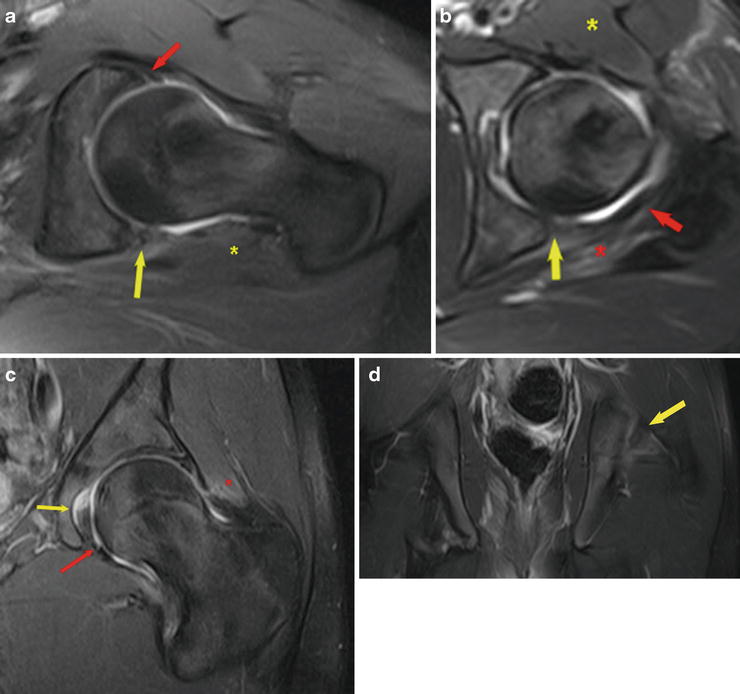
Fig. 31.5
(a–d) 3T MRI scan following left hip dislocation. (a) This image demonstrates a posterior labral tear with possible avulsion of the posterior acetabular wall (yellow arrow) along with increased soft tissue edema posteriorly (yellow asterisk). Partial detachment of the anterior labrum can also be seen (red arrow). (b) In this image, truncation of the posterior labrum can be seen along with irregularity or strain of the posterior capsule. Increased soft tissue edema can also be seen anteriorly and posteriorly (red and yellow asterisks) with the addition of a muscle strain (red asterisk). (c) This image demonstrates a high-grade partial tear or full-thickness tear of the ligamentum teres (yellow arrow). Strain of the gluteus minimus (red asterisk) and a mild joint effusion (red arrow) can also be seen. (d) Avulsion fracture involving the posterior acetabular wall of the left hip (yellow arrow)
Arthroscopy
The patient was positioned in the modified supine position on a traction table with a well-padded perineal post. Three loose bodies were discovered within the joint and were subsequently removed with an arthroscopic grasper and pituitary rongeur (Fig. 31.6a). Diagnostic arthroscopy revealed a posterior acetabular fracture between the 2 o’clock and 5 o’clock positions which involved approximately 10 % of the acetabulum (Fig. 31.6b). Tearing of the posterior labrum was found; however, the labrum was still firmly attached to the fracture fragment. Bruising of the anterosuperior labrum suggestive of CAM-type femoroacetabular impingement was found (Fig. 31.6c). The ligamentum teres was also completely torn (Fig. 31.6d).
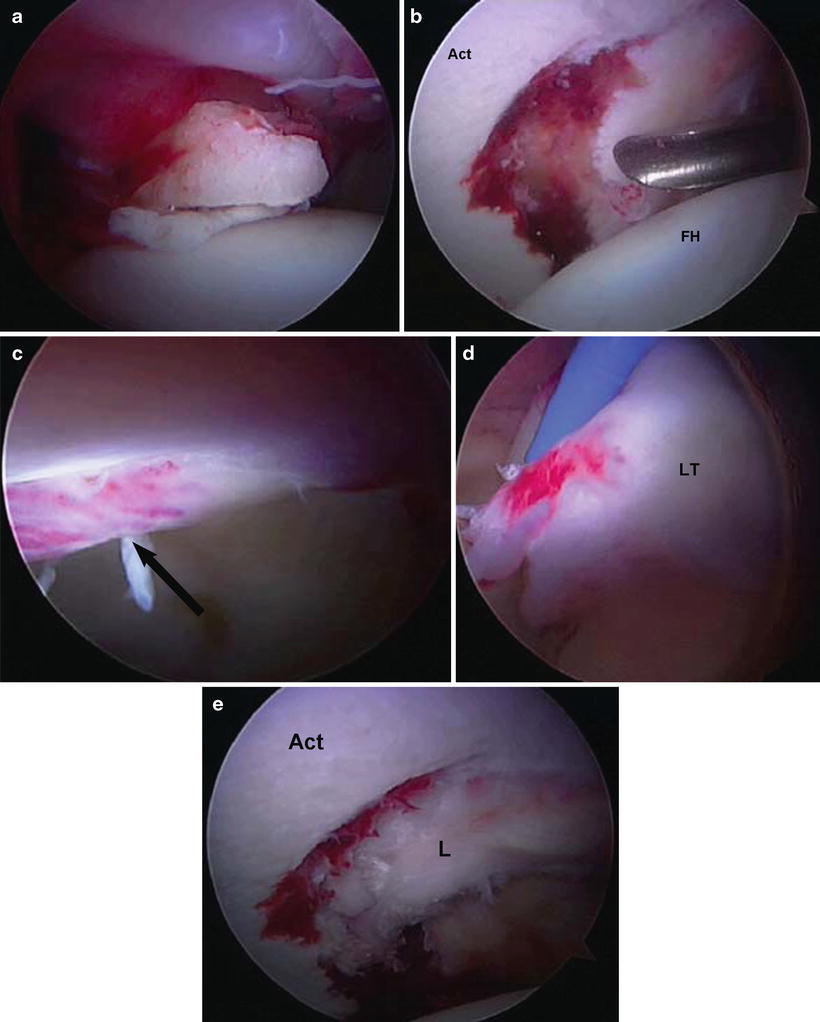
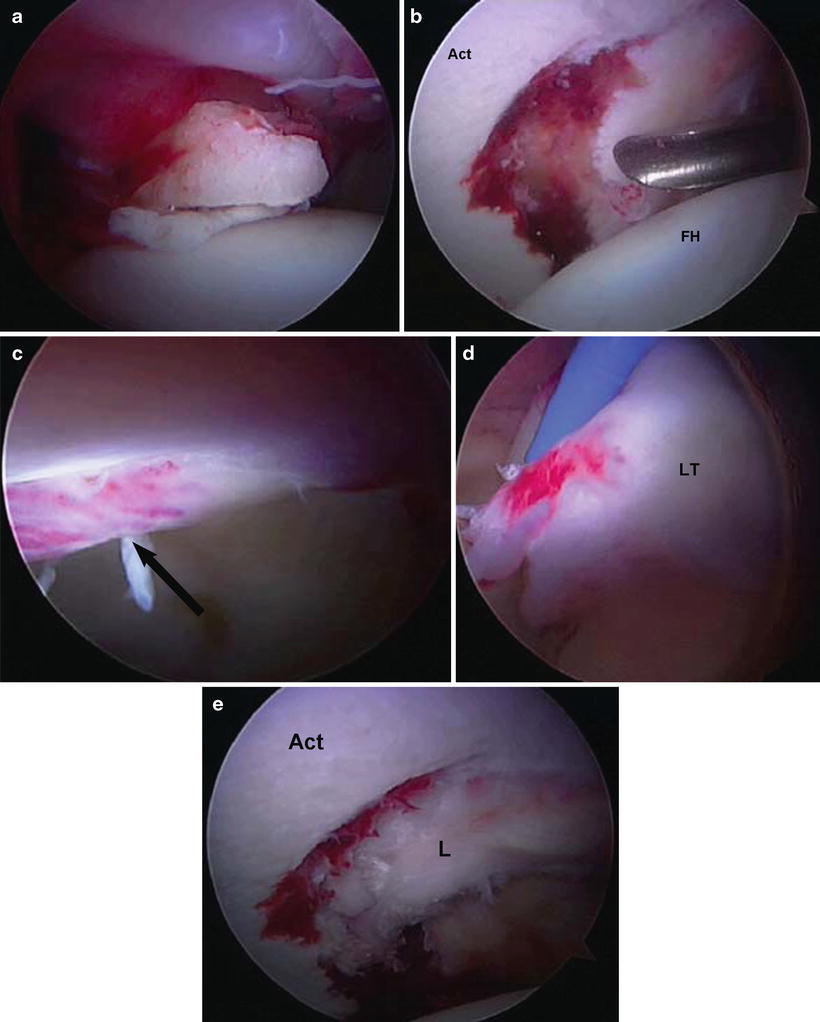
Fig. 31.6
(a–e) Arthroscopic images. (a) Loose bodies in the joint at the time of arthroscopy. (b) Cartilage damage associated with posterior acetabular rim fracture (Act acetabulum, FH femoral head). (c) Bruising of the anterosuperior labrum suggestive of CAM-type femoroacetabular impingement. (d) Torn ligamentum teres (LT). (e) View of acetabular rim fracture following fixation (Act acetabulum, L labrum)
Fragment fixation was undertaken given the increased risk of postoperative instability when a fracture fragment of this size is removed. Two 2.3 mm suture anchors were placed into the fracture site and the suture limbs were passed around the fracture fragment and firmly attached labrum. This method sufficiently reduced the fracture and restored the anatomy of the posterior acetabulum (Fig. 31.6e). The area of grade 4 chondromalacia was sufficiently debrided with a motorized arthroscopic shaver. Debridement of the labrum was then performed using a combination of radiofrequency ablation and arthroscopic shaving between the 2 o’clock and 5 o’clock positions. Debridement of the inflamed synovium and the completely torn ligamentum teres was also performed using the same instrumentation.
Traction was then removed and osteoplasty of the femoral head and neck was performed. After dynamic examination confirmed the site of the CAM lesion and labral impingement, an arthroscopic bur was used to resect excess bone from the 12 o’clock to the 6 o’clock position, thus reestablishing a normal femoral head–neck offset. The lateral epiphyseal vessels were identified and protected throughout the procedure. Dynamic examination was performed once again to confirm adequate osteoplasty, acetabuloplasty, and fracture fixation. The central and peripheral compartments were copiously lavaged with arthroscopic fluid. The capsulotomy was closed using two #2 sutures in a double-limb fashion and secured with a racking half-hitch knot. The arthroscopic instruments were removed and the portal sites were closed using 3-0 nylon sutures in a vertical mattress configuration.
Discussion
The femoral head should be immediately reduced in all cases of acute traumatic hip dislocations to prevent the development of avascular necrosis (AVN) [19]. Following reduction, stability should be assessed through an evaluation of passive range of motion. Stress radiography and/or fluoroscopic examination under anesthesia may be necessary in cases where physical examination reveals residual instability despite adequate closed reduction. In all patients, a postreduction CT scan of the pelvis is necessary to rule out the presence of an acetabular wall fracture, intra-articular loose bodies, and other injuries to the femoral head and/or neck. Aspiration of the joint may be necessary when significant hemarthrosis is visible on imaging studies to prevent femoral head osteonecrosis and to provide symptomatic relief [20, 21].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








