Timothy Beale, Jackie Brown, John Rout The anatomy of the head, neck and dental regions is complex. The continued advances in imaging (in particular computed tomography (CT), cone beam computed tomography (CBCT) and magnetic resonance imaging (MRI)) with ever faster imaging times and higher resolution studies have resulted in more anatomical detail revealing itself, none more so than in the head, neck and dental region where identifying subtle changes in the normal anatomy such as middle ear ossicular erosion in cholesteatoma, widening of the cranial nerve foramina in perineural/intracranial extension of disease and subtle erosion of the laryngeal cartilages in squamous cell carcinoma (SCC) of the larynx is crucial in the accurate diagnosis and staging of head and neck pathology and the planning of appropriate treatment. Knowledge of the normal anatomy and anatomical variants is the essential foundation required to support the recognition and accurate assessment of pathology in this complex region, even more so with the advent of more targeted treatment such as intensity-modulated radiotherapy (IMRT), brachytherapy or proton beam therapy.
ENT, Neck and Dental Radiology
Introduction
The Ear, Paranasal Sinuses And Nasal Cavity
The Auricle and External Auditory Canal
Anatomy
The auricle and external auditory canal (EAC) funnel the sound to the tympanic membrane. The EAC is approximately 25 mm in length, lined by squamous epithelium, has an S-shaped course and consists of a fibrocartilaginous lateral third and an osseous medial two-thirds (Fig. 67-1). In cross-section the canal has an oval configuration. The fibrocartilaginous portion is deficient inferiorly (fissures of Santorini) that act as conduits for infection and malignancy (see below).
Pathology
High-resolution axial CT (HRCT) or cone beam CT CBCT with multiplanar reformats (MPR) in the coronal and sagittal planes is essential for assessing the bony EAC.
Chronic Stenosing Otitis Externa
Recurrent otitis externa (Fig. 67-2) may result in a fibrotic band of soft tissue occluding the medial EAC. It is important for the radiologist to answer the following questions: Is there any erosion of the adjacent bony walls to suggest a more aggressive process? What is the depth of the occluding soft tissue? Does the fibrotic tissue extend to involve the tympanic membrane (TM)? Is there a normally pneumatised middle ear cleft deep to the occluding soft tissue? Always review the contralateral side as this pathology is commonly bilateral.
Exostoses and Osteoma of the External Auditory Canal
The EAC osteoma usually arises spontaneously, but exostoses are associated with repeated exposure to cold water and are also known as ‘surfer’s ear’. The two pathologies (Fig. 67-3) cannot be distinguished histopathologically; however, exostoses are usually broad-based and bilateral, whereas osteoma are pedunculated, unilateral and lateral to the bony isthmus of the canal. They may cause sufficient narrowing of the EAC to require surgery. It is important when assessing EAC exostoses and osteoma to answer the following questions: What is the maximum depth and transverse diameter of the exostosis? What is the exact site of origin of the osteoma? What is the distance between the medial aspect of the exostosis and the TM and the deep aspect of the exostosis and the descending facial nerve canal? Are there any associated obstructed secretions in the medial EAC and is the middle ear cleft normally pneumatised?
Keratosis Obturans
Keratosis obturans (Fig. 67-4) is usually a bilateral accumulation of keratin within the EAC. The CT appearances are of soft tissue filling the EAC that may be associated with expansion of the canal and remodelling but not erosion of the bony canal walls. Keratosis obturans is associated with otalgia and conductive hearing loss and most frequently occurs in young men.
External Auditory Canal Cholesteatoma
An EAC cholesteatoma (Fig. 67-5) can be differentiated from keratosis obturans as it is associated with erosion of the floor/posterior wall of the bony EAC and is usually seen in an older population (>40 years).
It may be indistinguishable on CT from SCC and otoscopy ± biopsy is suggested.
Necrotising Otitis Externa (NOE)
Also known as malignant otitis externa, a misleading term used because of what used to be the high mortality associated with this condition. The pathology is a necrosis usually of the walls and in particular floor of the EAC at the bony cartilaginous junction typically in the elderly diabetic patient who presents with severe otalgia. Pseudomonas is the usual organism. The infection commonly extends inferiorly via the fissures of Santorini (see the section ‘Anatomy’, above), causing a skull base osteomyelitis, and involves the soft tissues inferior to the skull base where the lower cranial nerves (VII to XII) may be affected (Fig. 67-6). Anterior extension into the temporomandibular joint may cause destruction of the mandibular condyle.
HRCT of temporal bone is the usual initial imaging technique. MR will more clearly assess any soft-tissue involvement, meningeal enhancement or oedema of the bone marrow. Nuclear medicine (gallium 67) is helpful in confirming the location of the infection and monitoring its response to treatment.
It is important to answer the following questions when assessing patients with NOE: Is there any erosion of the bony walls of the EAC? Is there any inflammatory change in the soft tissues inferior to the skull base, in particular around the stylomastoid opening of the facial nerve, and is there involvement/effacement of the normal parapharyngeal fat? Is there erosion of the skull base (look for loss of the normal dense line of the bony cortex of the clivus, petroclival region and petrous apex)? Is there anterior extension to involve the mandibular condyle or involvement of the contralateral side via the prevertebral and retropharyngeal soft tissues anterior to the clivus? Has the differential of an SCC of the EAC or a nasopharyngeal tumour with extension to the skull base been excluded?
Squamous Cell Carcinoma of the Auricle and External Auditory Canal
These are rare tumours presenting in the elderly (F > M) with a painful, discharging ulcerative lesion of the EAC that most frequently extends inferiorly. CT is the usual imaging technique (Fig. 67-7), but MRI is recommended if there is suspected superior extension into the middle cranial fossa or medial extension into the middle ear cleft (both are rare).
It is important to answer the following questions: As with all soft tissue noted within the bony EAC, is there any associated bony erosion? Is there extension outside of the EAC? Is there any nodal involvement (in particular, review the intraparotid and upper deep cervical nodes)?
Congenital Atresia/Stenosis of the External Auditory Canal
The EAC may be stenosed or completely atretic (absent). The atresia may be membranous, bony or a mixture of the two. The atresia is usually unilateral in non-syndromic and bilateral in syndromic patients (Fig. 67-8). The rule of thumb is the more severe the EAC abnormality, the greater the auricular deformity (microtia/anotia). The inner ear structures are usually not affected unless there is severe EAC atresia with an absent auricle, small middle ear cleft and absent ossicles. If surgery is being considered it is important to assess the following on CT:
• The severity and type of the atresia.
• The size and degree of pneumatisation of the middle ear cleft.
• The appearance of the ossicles, in particular:
• Is a stapes superstructure present?
The Middle Ear
Anatomy and Physiology
The tympanic membrane (TM) is inclined at an angle of 140° in relation to the superior border of the EAC, measures 9–10 mm in diameter and separates the middle ear from the external ear (Fig. 67-9). The lateral (short) process of the malleus is attached to the TM at the malleal prominence and the handle at the umbo. Extending both anterior and posterior from the malleal prominence are folds separating the TM into a superior, thinner and more flexible pars flaccida and the more inferior pars tensa. The middle ear cleft is divided from superior to inferior into epitympanum (attic), mesotympanum and hypotympanum and contains three ossicles (the malleus, incus and stapes), two muscles (tensor tympani attached to the neck of the malleus and stapedius to the head of the stapes). Part of the intrapetrous course of the facial nerve and one of its branches (the chorda tympani) also pass through the middle ear cleft.
HRCT including CBCT is the most common technique used for assessing the middle ear cleft usually in the clinical setting of conductive or mixed hearing loss. MRI is a complementary investigation used to assess possible intracranial complications arising from middle ear pathology, the rare middle ear tumours such as glomus tympanicum or where a recurrence of cholesteatoma is suspected (see below).
Pathology
Cholesteatoma
Cholesteatoma is a poor term for this pathology as it neither is a tumour nor does it contain cholesterol. It is actually skin in the wrong place. There are two types: the common acquired (98%) and the rarer congenital (2%) cholesteatoma. In acquired cholesteatoma, as a consequence of negative middle ear pressure, a retraction pocket develops usually in the more flexible pars flaccida (superior aspect) of the TM (Fig. 67-10A), but occasionally in the pars tensa (inferior aspect). Desquamated skin accumulates in the retraction pocket and can enlarge, causing bony destruction most frequently of the scutum and long process of the incus, but may extend to involve the otic capsule overlying the lateral semicircular canal (Fig. 67-10B), that may be associated with symptoms of dizziness, the tegmen tympani and the tympanic facial nerve canal (causing facial palsy).
Usually the diagnosis of cholesteatoma is apparent from the otoscopic appearances of a retraction pocket in acquired and a retrotympanic ‘pearl’ of cholesteatoma behind an intact TM in congenital cholesteatoma (Fig. 67-11). The clinician needs to know how extensive the cholesteatoma is, which can be assessed by the degree of ossicular or bony erosion.
In particular, answer the following questions:
• Is the bony roof (tegmen tympani or mastoideum) eroded?
• Is the otic capsule overlying the lateral semicircular canal eroded?
• Is there ossicular erosion (in particular, is the stapes eroded)?
• Does the cholesteatoma abut the tympanic facial nerve canal?
A pars flaccida cholesteatoma is identified by a mass in the attic (epitympanium) lateral to the head of malleus and body of incus associated with ossicular erosion in 70%. A pars tensa cholesteatoma is identified as soft tissue in the posterior mesotympanum often extending medial to the ossicles. HRCT is used for assessing any bony involvement. Non-echo planar diffusion-weighted MR (non-EPI DWI) is increasingly used for assessing whether there is any recurrent or residual cholesteatoma in patients who have undergone canal wall preservation surgery where otoscopy provides limited visualisation. Cholesteatoma consisting of desquamated skin shows markedly restricted diffusion (Fig. 67-12) and can be differentiated from other soft tissue (granulation tissue, etc.).
Tympanosclerosis
The CT appearance is of foci of calcification, punctate or web-like in the middle ear cleft (Fig. 67-13) and tympanic membrane. Usually this is associated with a long history of otitis media (OM). The suspensory ligaments and muscles may also calcify. There is varying conductive hearing loss depending on the degree of ossicular fixation. If the tympanic membrane only is involved (calcified), the condition is known as myringosclerosis.
Otosclerosis
The diagnosis is usually suggested clinically. The hearing loss may be conductive, mixed or sensorineural. Otospongiosis is a term also used and describes the spongiform changes within the involved bone. In patients with otosclerosis the normal dense bone is replaced by foci of spongy less dense bone. Patients usually present in the third decade. The CT appearances are commonly bilateral (85%) and there may be a family history. There are two main types: fenestral and retrofenestral.
Fenestral.
The spongiotic foci occur in the lateral wall of the otic capsule in the fissula antefenestram (anterior to the oval window; Fig. 67-14) where it extends posteriorly to involve the footplate, fixing the anterior crus of the stapes causing CHL. The round window and cochlear promontory may also be involved.
Retrofenestral or Cochlear.
Spongiotic foci replace the normal dense bone of the otic capsule surrounding the cochlea (Fig. 67-14) and may encroach on the cochlea and, less commonly, the vestibule and semicircular canals, causing mixed or sensorineural hearing loss. The most frequent location for a spongiotic focus is between the middle turn of the cochlea and the anterior aspect of the lateral internal auditory canal. In severe cases the cochlea is encircled, giving the appearance is of a cochlea within a cochlea. CT is used for assessing otosclerosis although the foci may be visible on MR as high signal areas on T2 that enhance post-gadolinium.
Cochlear otosclerosis is rare in the absence of fenestral disease.
Questions to answer when reviewing the CT are the following:
• Is there fenestral or pericochlear otosclerosis or both?
• Is there bilateral involvement (in 85% on CT) that may only be clinically evident on one side?
• Is the round window also involved? Round window involvement may reduce the effectiveness of surgery.
• Is the facial nerve dehiscent as this may complicate surgery?
Ossicular Disruption
Nearly all ossicular disruption is associated with a temporal bone fracture. Incudostapedial joint (ISJ) disruption is the commonest derangement. Malleoincudal disruption results in loss of the normal ‘ice cream cone’ appearance on axial images of the head of malleus articulating with the body of the incus (Fig. 67-15). Complete dislocation of the incus is the next most common finding. Much more rarely found are fractures of the individual ossicles. The incus is the ossicle most frequently disrupted as the malleus is supported by three ligaments and the tensor tympani muscle and the stapes by the annular ligament and the stapedius muscle.

When assessing ossicular trauma, look first for the normal ‘ice cream cone’ appearance of the malleoincudal joint and then closely assess the alignment of the distal long process of the incus with the head of stapes at the ISJ and compare with the normal contralateral side.
Venous Sinus Thrombosis
The sigmoid sinus is an immediate posterior relation to the mastoid air cells and mastoiditis may result in sinus thrombosis with occasionally severe intracranial complications (Fig. 67-16). The transverse sinus and jugular bulb may also be involved, although the latter is usually thrombosed due to retrograde extension from the neck.

Always assess the bony dural sinus plate overlying the sigmoid sinus if adjacent air cells are opacified. If there is bony erosion, MRV or CT venography may be helpful to exclude thrombosis.
Intracranial Complications
Fortunately, intracranial complications from petromastoid infection are now rare. The commonest is extradural empyema in the posterior fossa often associated with sigmoid sinus thrombosis. Very rarely subdural empyema and intracranial abscesses may occur.
The Inner Ear
Anatomy and Physiology
The inner ear consists of endolymph containing the functional sensory epithelium surrounded by perilymph and covered by a bony labyrinth (otic capsule). Sound is transmitted from the TM via the ossicles to the oval window. The mechanical vibrations via the vestibule then pass to the perilymph containing scala vestibuli up to the apical turn of the cochlea, returning via the perilymph containing scala tympani to the round window (Fig. 67-17A). Both perilymph scala surround the endolymphatic scala media or cochlear duct that contains the hair cell receptors of the organ of Corti. It is movement of these hair cells that generates electronic impulses in the cochlear nerve fibres. Higher frequencies up to 20 kHz are perceived in the basal turn and 20 Hz at the apex. The range of intensity of sound is huge and is expressed in alogorithmic decibel scale of 0–120 dB. A quiet whisper is 30 dB, a lawnmower is 90 dB and a jet plane take-off is 120 dB.
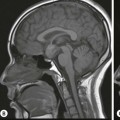
The electrical output of the hair cells passes to the spiral ganglion in the cochlea and then the cochlea division (Fig. 67-17B) and main trunk of the vestibulocochlear nerve to enter the brainstem in the upper lateral medulla synapsing with two cochlear nuclei, the latter forming a bulge in the lateral recess of the fourth ventricle and the foramen of Luschka. Within the brainstem, nerves pass in ipsi- and contralateral pathways to the inferior colliculus of the mid-brain, medial geniculate body of the thalamus and from there to the posterior aspect of the superior temporal gyrus. Ipsilateral hearing loss results when there is damage to the auditory pathway between the hair cells in the cochlea and the brainstem nuclei and bilateral hearing loss between the brainstem nuclei and inferior colliculi.
The semicircular canals consist of three rings, each orthogonal to the others, again containing perilymph bathing the endolymph. The superior and lateral canals are innervated by the superior vestibular nerve and the posterior by the inferior vestibular nerve. The semicircular canals form the kinetic labyrinth as they respond to rotational movement and acceleration. The dilated component of the semicircular canals called ampullae contains the hair cells forming the electronic impulses.
The vestibule consists of the utricle and macule (static labyrinth) and detects the position of the head relative to gravity.
Pathology
Vestibular Schwannoma
Vestibular schwannomas are the most common cerebello-pontine angle (CPA) tumour and the most common pathology causing asymmetrical sensorineural hearing loss (SNHL). The majority are centred within the internal auditory canal, or at the porus acusticus and occur sporadically. When bilateral they indicate the diagnosis of neurofibromatosis type 2. Only a minority (approximately 2.5%) of patients who present with tinnitus or asymmetrical hearing loss have a vestibular schwanomma. There is no relationship between the size of the tumour and degree of hearing loss. The management approach is ‘wait and scan’ for the majority of vestibular schwannomas as approximately 60–70% do not increase in size on follow-up (MR) imaging. Those that require intervention have two options: surgery via retrosigmoid, translabyrinthine or subtemporal middle cranial fossa approach, or gamma-knife (radiation) treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree