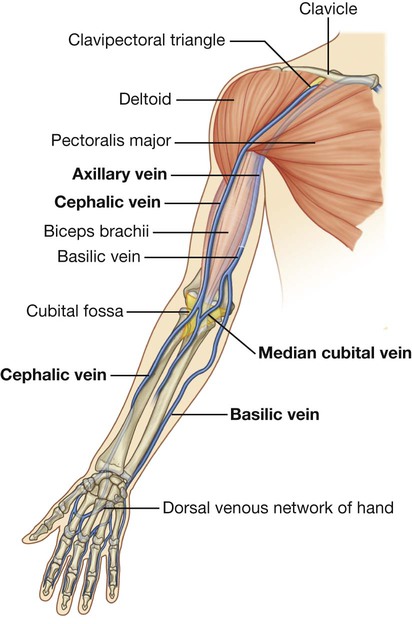
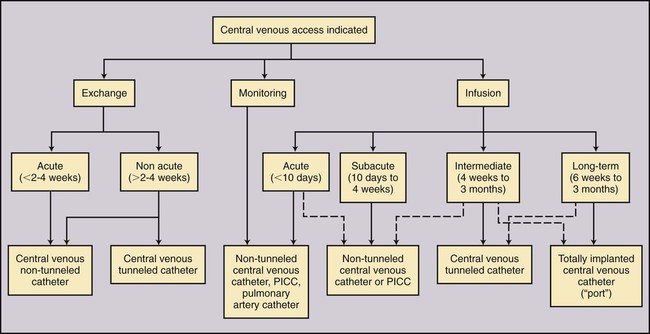
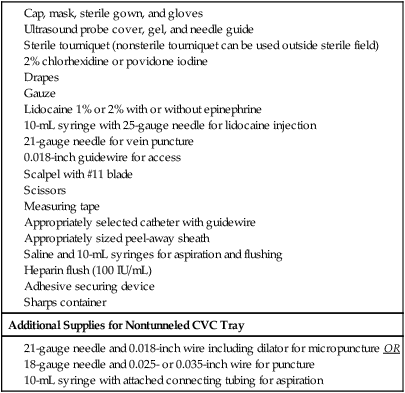
Indications for placement of a PICC or nontunneled CVC for infusion therapy include (1) rapid infusion of fluids or blood products to maintain hemodynamic stability, (2) infusion of vesicant solutions such as chemotherapeutic, cytotoxic, or inotropic medications or infusates with pH less than 5 or above 9, more than 500-600 mOsm, more than 10% dextrose, or more than 5% amino acids, (3) total parenteral nutrition, (4) active infection that prevents placement of a more permanent device, and (5) coagulopathy that prevents placement of a more permanent device.1–3 Catheter choice should be made with expected length of treatment in mind. For short-term access (<2-4 weeks) for infusion, monitoring, or exchange therapy, a PICC or small-bore nontunneled CVC would be indicated. Some studies have reported PICCs functioning for longer than 1 year, and some anecdotal reports have noted functioning PICCs that have been present for longer than 2 years.4–6 However, such reports represent the exception rather than the rule. For long-term access (>2-4 weeks) a tunneled catheter or implantable port may be indicated. A selection algorithm for choosing among PICCs, nontunneled CVCs, tunneled CVCs, and ports is provided in Figure 118-1. Indications for pediatric PICCs may include the need for venous access of 6 days or more or the need to administer vesicants or other infusates requiring dilution in the central venous system.3 Early PICC placement may spare patients numerous venipunctures. Selection criteria for catheter placement in pediatrics are otherwise similar to adults: PICC placement may be precluded in patients in whom a suitable peripheral vein cannot be identified. Central venous thrombosis or occlusion also poses a relative contraindication. Occasionally a guidewire can be used to traverse the thrombosed vein, or access to the central veins can be achieved through collaterals, thus permitting central venous placement of the catheter tip. When this fails, PICCs may be positioned peripheral to the occluded central veins, thereby resulting in subclavian or axillary placement of the catheter tip. This position may be adequate provided fluids to be administered are not hyperosmolar or vesicant fluids. It has been shown that PICCs placed in a noncentral vein can provide reliable safe intravenous access for administration of many medications for up to 2 weeks’ duration.7 Placement of a PICC is contraindicated in any person undergoing hemodialysis or in whom hemodialysis is anticipated, including patients with renal transplants. PICCs are associated with a significant rate of peripheral venous thrombosis.8 To preserve peripheral veins for future hemodialysis access, the National Kidney Foundation Kidney Disease Outcomes Quality Initiative (NKF KDOQI) advises against placement of PICCs in this patient population.9,10 • End-hole catheters are the most common catheter design, with all lumina opening within close proximity of the catheter tip. These devices may be trimmed at the tip to achieve an appropriate length. • Staggered-tip dual-lumen catheters are specifically designed for therapies that require simultaneous rapid aspiration and infusion with limited mixing (hemodialysis and apheresis). These devices should not be trimmed, so their staggered-tip configuration is maintained. • Valve-tipped catheters have a specially designed slitlike two-way valve at the catheter tip that is closed in the resting state. The valve opens inward with aspiration and outward for infusion, with the potential advantage of not requiring routine heparinization to prevent catheter thrombosis. The Groshong catheter (C.R. Bard Access Systems Inc., Salt Lake City, Utah) is a valve-tipped catheter. Valve-tipped catheters cannot be trimmed at the tip, but they have a removable external connection that allows the back end to be trimmed for adjustment of length. The Vaxcel catheter with pressure activated safety valve (PASV) (Boston Scientific Corp., Natick, Mass.) incorporates a valve into the hub of the catheter, allowing the tip to be trimmed. PASV catheters have a lower recorded rate of infection, thrombosis, and phlebitis compared to distal valve-tipped catheters.11–13 Required supplies for PICC and nontunneled IJ, subclavian, and femoral CVC placement are listed in Table 118-1. TABLE 118-1 Standard Ultrasound-Guided PICC Tray CVC, central venous catheter; PICC, peripherally inserted central catheter. Accuracy of bedside placement is also increased using electrocardiogram (ECG)-assisted techniques and is being used in lieu of radiographic tip verification.14 Traditional bedside ECG monitors can be used, but dedicated systems are now coming to market to emphasize this technique. At our institution, we use the Sapiens Tip Confirmation System (TCS) (C.R. Bard Access Systems) that uses external ECG electrodes to detect intravascular ECG P-wave changes as the catheter approaches the cavoatrial junction. The preferred location for PICC placement is in the nondominant arm. Placement above the antecubital fossa is preferred and may lower the risk of phlebitis. The order of preference is the basilic, brachial, cephalic, then median cubital vein. The preferred location for nontunneled CVC placement in order of preference is the right IJ, left IJ, subclavian, then femoral vein. Anatomic reference is provided in Figure 118-2. The appropriate length of catheter should be calculated before sterile prep and venipuncture. This is critical in the absence of fluoroscopy. The desired tip position is in the distal third of the SVC or at the cavoatrial junction. Measurements are taken from the venipuncture site to the ipsilateral axillary crease to the right sternoclavicular joint and inferiorly to the third intercostal space at the right parasternal border (Fig. 118-3). Lower extremity PICCs are measured from the venipuncture site along the course of the vein to the right of the umbilicus to the xiphoid. Adding the estimated depth of subcutaneous fat to the measurement will increase accuracy. When approaching from the left, adding 1 to 2 cm may increase accuracy as well, owing to catheter flexibility as it courses from left to right in the left brachiocephalic vein. Evaluating a chest radiograph prior to measurement may also help judge the tortuosity of the venous system. Lum’s CVC Measurement guide provides an estimated catheter length based on patient height (Table 118-2). TABLE 118-2 Lum’s Central Venous Catheter Measurement Guide
Peripherally Inserted Central Catheters and Nontunneled Central Venous Catheters
Indications
Contraindications
Equipment
Catheter Types
Procedural Supplies
Technique
Anatomy and Approach
Technical Aspects
Ultrasound-Guided Placement of a Peripherally Inserted Central Catheter
Height (in)
R. PICC (cm)
L. PICC (cm)
R. JC (cm)
L. SC (cm)
R. SC (cm)
Height (cm)
4 ft 8 in
42.5
46.5
13.0
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access