Fig. 20.1
Chronic lateral epicondylitis. (a) Longitudinal 12-5 MHz US scan demonstrates a convex, swollen external margin of the extensor tendons (arrow). (b) Longitudinal 12-5 MHz US shows a concave, atrophic external margin of the extensor tendons (arrow); arrowhead, radial head
Fig. 20.2
Chronic lateral epicondylitis. (a) Longitudinal and (b) axial 12-7 MHz US of the common extensor origin, enthesophyte (a, arrow) and internal tendon calcification (b, arrow) and erosive cortex (curved arrow). (c) Longitudinal 12-7 MHz colour Doppler US, hypervascular extensor tendons. (d) Axial and (e) longitudinal 12-7 MHz US of the extensor carpi radialis brevis tendon tear (arrow); arrowheads, radial head
Hypoechogenicity with loss of the fibrillary pattern related to tendinosis is often found in the region of the extensor carpi radialis brevis. To discriminate this finding with anisotropy artefacts, it has to be shown in two orthogonal directions. This tendon indeed has an oblique course from depth to surface and thus is prone to anisotropy artefact, which is the well-known pitfall in US tendon assessment. A tear typically appears as an anechoic fluid-filled gap between the cortex and tendon origin (Conell et al. 2001; Jacobson and van Holsbeeck 1998). Contrary to deep calcifications, superficial linear calcifications continue with the bone at the origin of the ECR have a low specificity as it has been reported that only 39 % of all enthesophytes are symptomatic (Struijs et al. 2005).
Convex external contour, erosive cortex of the epicondyle, internal calcifications, a tear, and hypervascularity all have a specificity of 100 %, PPV 100 %, and a conclusive positive likelihood ratio (Obradov and Anderson 2012). Unfortunately, the sensitivity for these parameters is low; the respective values for the affected elbows are 33, 18, 33, and 14 %. Thus individually these findings are not sufficient as a stand-alone diagnostic criterion. Hypervascularisation has the highest sensitivity (57–95 %) in the group of individual findings, with 88–100 % specificity and with a confidence interval of approximately ±10 %(Torp-Pedersen et al. 2002; Noh et al. 2010; Obradov and Anderson 2012). Tendon hypervascularity is a relatively specific US sign for a painful tendon (Breidahl et al. 1996; Torp-Pedersen et al. 2002) (Fig. 20.2). However, the combination of grayscale and (power) colour Doppler changes is diagnostically superior to identify chronic tendinopathy.
Recently different authors concluded that the lack of both hypervascularity and grayscale changes on ultrasound examination substantially increases the probability that the condition is not present and should prompt the clinician to consider other causes for lateral elbow pain (Toit et al. 2008; Obradov and Anderson 2012). In the absence of US findings in tendinopathy in acute cases with duration of symptoms less than 6 months, it is wise to exclude other possible causes for the pain in the same region.
MRI demonstrates thickening of the tendon with increased signal intensity within the tendon on T1 and fluid-sensitive T2 sequences correlating with mucoid degeneration and neovascularisation presented with or without reactive epicondylar bone marrow oedema. Discrimination between degeneration and angiogenesis is not possible on MR imaging. In the case of partial or complete tears, signal intensity is similar to that of fluid, and a separation of the tendinous attachment from the condyle can be seen. Injury of the lateral collateral ligament complex can be associated with a tear of the extensor tendons and may result in therapy-resistant lateral tendinopathy. As the medial collateral ligament (MCL) is the primary stabiliser of the medial elbow joint, concomitant injury of the MCL and flexor tendons can occur as well. Calcifications in the tendon origin are presented as loss of the signal intensity on all sequences. Signs of the associated elbow injuries, ulnar neuritis, or secondary osteoarthritis may also be observed.
20.3 Triceps Tendinopathy
The triceps muscle consists of the long, medial, and lateral head. It originates at the scapula and humerus and is attached to the olecranon and the antebrachial fascia. Triceps tendinopathy is the result of intrinsic muscle overload in combination with fast extension of the triceps as seen in baseball pitchers and javelin throwers. Pain during resisted elbow extension or complete flexion is typical for this injury.
Distal triceps tendon rupture is the least common of all tendon ruptures and can be associated with small shell-like bone avulsion (Viegas 1990) (Fig. 20.3). The injury is caused by either a direct blow or by forceful contraction of the triceps during active extension and is seen in weight-lifting and other strength sports. Olecranon bursitis, tendinopathy, and steroid injection can lead to the triceps rupturing (Van Riet et al. 2003).
Fig. 20.3
A 25-year-old male, with shelf avulsion of triceps tendon insertion at the right elbow. (a) Lateral radiograph and (b) ultrasound examination of the right elbow with shelf-like bone fragment (arrow) with 2.5 mm diastasis from the olecranon; margins of avulsion site are marked with arrowheads
20.3.1 Radiologic Imaging of Triceps Tendinopathy
Triceps tendinopathy is an uncommon finding, which in chronic cases can demonstrate calcifications in radiographs (Fig. 20.4).US shows a thickened often hypoechoic tendon at the place of the concordant pain. The calcifications are hyperreflective with acoustic shadowing if the calcification is solid. MRI shows abnormal morphology with increased thickness and increased signal intensity on all sequences.
Fig. 20.4
Triceps tendinopathy. (a) Radiograph, axial view of the elbow demonstrates calcification (arrow) in the triceps tendon. (b) Longitudinal 12-5 MHz US of the olecranon with triceps tendon calcification (arrow); olecranon (asterisk)
The clinical diagnosis of an acute distal triceps tendon rupture can be difficult due to pain that limits the physical examination. Plain radiographs show if present a specific shell-like avulsion of the olecranon. MRI and US have a role in the early diagnosis and differentiation between partial and complete tears. US shows the retracted triceps tendon surrounded by fluid and can visualise atypical ruptures of the musculotendinous junction or tear of the muscle bellies (Kaempffe and Lerner 1996). The sagittal plane MRI with both flexed and extended elbow has been shown to most effectively distinguish between partial and complete tears (Murphy 1992). This is important as complete tears require surgery to avoid contraction; partial tears are treated conservatively. Specific MRI findings also include soft tissue oedema, reactive hyperaemia of the olecranon, bone trabecular fractures, intramuscular haemorrhages, and bursal fluid (Blease et al. 1997) (Fig. 20.5).
Fig. 20.5
Partial tear of the triceps tendon. (a) Coronal and (b) axial fat-suppressed T1-weighted MR arthrogram demonstrates intrasubstance focal areas (arrow) of the contrast corresponding to fluid-filled defects
20.4 Olecranon Bursitis
Olecranon bursitis, also known as student’s elbow or miner’s elbow, is the most common superficial bursitis in the human body (Morrey 2000). The primary cause is acute or repetitive trauma from football, ice hockey, or wrestling injuries, and secondly it is associated with systemic inflammatory diseases, such as gout, rheumatoid arthritis, hydroxyapatite deposition, and calcium pyrophosphate deposition, and with patients undergoing chronic dialysis. Infection with Staphylococcus aureus as well as a rare case of tuberculosis can also be present.
20.4.1 Radiologic Imaging of Olecranon Bursitis
Radiographs may show soft tissue swelling and, in chronic cases, calcification as an expression of an old bleeding. A cortical destruction of the olecranon in the case of the infectious involvement of the bone may also be visible.
US findings include hypo- or anechogenic fluid collections superficial to the olecranon. The olecranon bursa is a typical superficial bursa with a synovial membrane supported by dense irregular connective tissue interposed in the loose areolar tissue between the skin and bone; this causes an irregular lining with internal septations specific for distended subcutaneous bursae on ultrasound images (Fig. 20.6).
Fig. 20.6
Olecranon bursitis. (a) Transverse and (b) longitudinal 12-7 MHz US reveals distended bursa with multiple internal septations. (c) Colour Doppler 12-5 MHz US shows typically peribursal hypervascular pattern and septations with irregular lining specific for subcutaneous bursae
Fluctuating hyperechoic particles can be seen in crystal deposition disease. Colour Doppler imaging can visualise thick synovium with rim-like hypervascularisation and soft tissue hyperaemia of the subcutaneous fat.
In chronic haemorrhagic or septic bursitis, homogeneous predominant hyperechoic content is present, resulting in a complex image of the bursitis. US-guided aspiration can easily be performed in combination with corticosteroid injection in non-infectious inflammatory diseases (Fig. 20.7).
Fig. 20.7
US-guided aspiration of the chronic inflammatory olecranon bursitis. (a) Longitudinal and (b) axial 12-5 MHz US shows needle aspiration of the bursal fluid (same patient as 20.6)
MRI demonstrates localised fluid signal intensity lesions which in the case of haemorrhage get a more complex aspect. Marked enhancement of the bursal synovium and subcutaneous fat is present in septic bursitis after intravenous gadolinium DTPA administration. Oedema and infectious impairment of the underlying olecranon and eventually oedema and other abnormalities of the triceps tendon can be seen on MR imaging. Although complete differentiation between septic and nonseptic olecranon bursitis is not possible, the septic bursitis is excluded in the absence of bursal and soft tissue gadolinium DTPA enhancement (Floemer et al. 2004).
20.5 Distal Biceps Tendon Injuries
The biceps brachii has a distal tendinous insertion at the tuberositas brachii and a second distal insertion, the lacertus fibrosus, on the volar side of the superficial fascia of the forearm flexor muscle compartment. Distal biceps tendon injuries primarily involve the tendon and secondarily the lacertus fibrosus. They vary in range from tendinopathy to partial and complete tears. Distal biceps tears occur in weight-lifters, bodybuilders, and manual labourers. It happens predominantly in men in their fourth decade. Smokers have a 7.5 times higher risk of getting a distal biceps rupture than non-smokers (Safran and Graham 2002). Possible locations of the injury are at the distal musculotendinous junction, midsubstance of the tendon, and, the most common one, the avulsion from the radial tuberosity. The latter is associated with increasing pain anterior at the elbow during pronation movement. During pronation the radial tuberosity rotates posterior, eventually resulting in impingement of the biceps tendon at its distal insertion together with the peritendinous bursae (bicipitoradial bursa and interosseous bursa) between the proximal radius and ulna metaphysis. Enthesophytes or hypertrophic tuberositas radii, distended bursa, and tendinopathy reduce the interosseous space and cause or increase impingement of the tendon. In complete tear of the tendon, the lacertus fibrosus is overloaded and may become tendinopathic causing specific tenderness during biceps muscle activity against resistance at the site of its insertion on the proximal volar side of the flexor muscle compartment. Operative tendon repair within two weeks shows good long-term results.
20.5.1 Radiologic Imaging of Distal Biceps Tear
Both radiographs and US may show intratendinous calcification in chronic cases of tendinopathy (Fig. 20.8).
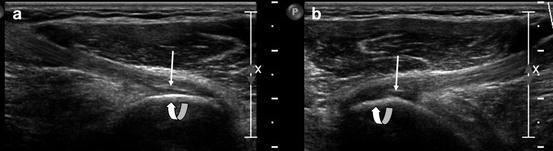
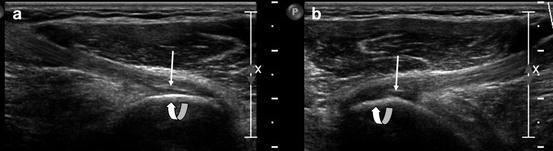
Fig. 20.8
(a, b) 12-5 MHz US, bilateral biceps insertion tendinosis with linear calcification (arrow) and minor thickening; curved arrow, tuberositas radii
In the case of (sub)acute biceps tendon tears, US shows hypoechoic fluid in the tendon bed and proximal retraction of the complete torn tendon. The tendon insertion at the tuberositas radii is not easily demonstrated on ultrasound examinations. If anterior-medial angled view is not successful, posterior evaluation in pronated position with elbow flexion (cobra position) may add to the evaluation of the distal 1 cm of the tendon (Figs. 20.9, 20.10, and 20.11). Thickening, thinning, or waving of the tendon without discontinuity can be seen in the case of partial tears (Miller and Adler 2000) (Fig. 20.12). Distension of the interosseous and bicipitoradial bursa is also demonstrated. Complete or partial fatty infiltration of the muscle belly is seen in a chronic stadium (Fig. 20.13) of tendon tear.
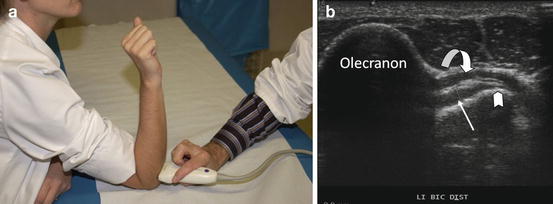
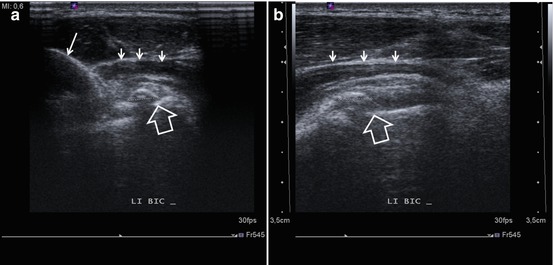
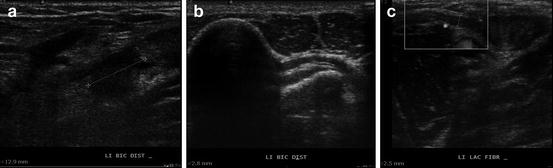
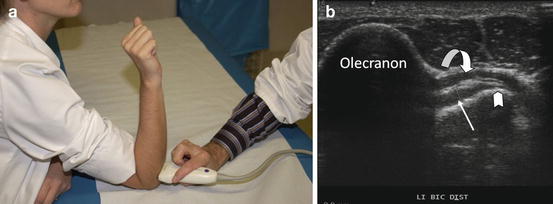
Fig. 20.9
Cobra position with elbow flexion and pronation for ultrasonographic evaluation of the distal biceps tendon at the level of the tuberositas radii insertion. (a) Probe position in cobra position. (b) 13-5 MHz US, biceps tendon (arrow), tuberositas radii (arrowhead), supinator muscle (curved arrow)
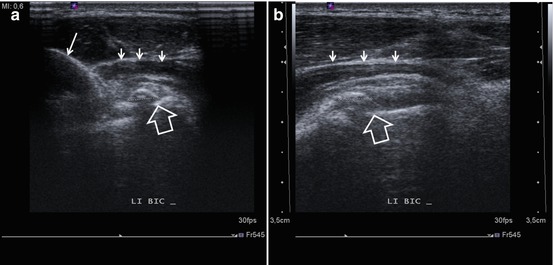
Fig. 20.10
Male patient, 33 y, painfull pronation movement at the left elbow. US 13-5 MHz ultrasound examination in cobra position with thickening of the distal biceps related to intratendinous calcification, 3.5 mm, with acoustic shadowing (calcification between marks) (a) axial imaging plane, (b) oblique axial imaging plane. Supinator muscle (small arrow), olecranon (long arrow), radial tuberosity (big arrow)
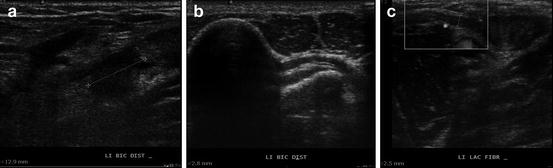
Fig. 20.11
Male patient, 56 y, painful snap at the left cubital fossa 5 days ago with residual pain at the level of the proximal ulnar flexor compartment. (a) US 13-5 MHz, longitudinal view at cubital fossa, demonstration of full-thickness tear of the biceps with minor retraction of 13 mm, between marks. (b) US 13-5 MHz, cobra view, normal distal biceps tendon with normal insertion at the tuberositas radii. (c) US 13-5 MHz, transverse view at the level of the ulnar flexor compartment, proximal third. Thickening of the lacertus fibrosus (2.5 mm) insertion on the superficial fascia of the flexor muscle compartment with localised pain during compression and elbow flexion against resistance
Fig. 20.12
Chronic distal biceps tendon rupture at the mid-portion of the tendon. (a) Longitudinal and (c) transverse 12-5 MHz US reveals proximal retracted muscle without distal tendon visualisation (arrow). (b) Longitudinal and (d) transverse 12-5 MHz US shows normal tendon (arrow) at the opposite side
Fig. 20.13
Chronic rupture of the tendon of the caput breve of the biceps. (a) Axial 12-5 MHz US and (b) axial T2-weighted MR image show fat degeneration of the caput breve muscle belly (asterisk) and normal structure of the caput longum muscle, the so-called black and white sign
MRI is performed with the patient lying prone on the imaging table and with the arm extended over the head in 90° of elbow flexion, abduction, and supination (FABS) position (Giuffrè and Moss 2004) (Fig. 20.14). Coronal T1 and fluid-sensitive T2 sequences show the distal biceps tendon in the longitudinal axis.
Fig. 20.14
Coronal T2-weighted fat-suppressed image of the elbow in flexion, abduction, and supination (FABS) position. Distal biceps tendon (arrow) is longitudinally presented till its attachment on the radial tuberosity (asterisk)
Differentiation between partial and complete tears can be made. In the case of a rupture, fluid collection in the position of the lacertus fibrosus can be identified. Bursal widening is demonstrated.
20.6 Medial Collateral Ligament Complex Injuries
Medial collateral ligament (MCL) injuries are the result of chronic repetitive valgus trauma related to throwing activities but can also be seen in posterior elbow dislocation. The MCL consists of anterior, posterior, and transverse bundles. The anterior bundle connects the medial epicondyle and sublime tubercle of the ulna and is most prone to injury.
Complete ruptures are often the result of acute trauma, while partial ruptures are often seen in throwing athletes. Tears occur proximally, distally, or at the level of the midsubstance. They can be associated with tears of the flexor digitorum superficialis due to the close relation with this muscle.
Posteromedial impingement syndrome has been seen in the setting of existing valgus instabilities which resulted from chronic repetitive microtrauma in throwing athletes (Frostick et al. 1999). These valgus extension overloads (VEO) result in MCL injuries with inflammation and partial or complete tears. The light subluxation of the elbow leads to posteromedial impingement of the olecranon with consecutive osteophyte formation and eventually intra-articular bodies (Wilson et al. 1983) (Fig. 20.15). Associated possible injuries are flexor-pronator injury and ulnar nerve entrapment as a result of cubital tunnel syndrome . In the latest stadium of the chronic valgus instability, osteochondral defects of the radiocapitellar joint can also be seen.


Fig. 20.15
Male, 27 y, javelin thrower with chronic complaints of posterior impingement. MRI, 1.5 T coronal (a) and sagittal (b) T2-WI with FS, ultrasound 15-5 MHz, oblique coronal US of MCL (c), and posterior sagittal view (d). Thickening of the anterior band of the MCL (arrowhead) with bone fragment (arrow) on (a, and c). Loose body at the olecranon fossa with marked joint effusion on sagittal images (b, d)
20.6.1 Radiologic Imaging of Medial Collateral Ligament Complex Injuries
Radiographs should be the first choice of imaging modality. Chronic MCL injuries can be associated with MCL ossification which is clearly visible on the radiographs. Ulnar traction spurs or avulsion of the sublime tubercle can be seen as well (Fig. 20.16). Reversed axial projection allows better visualisation of olecranon degenerative changes.
Fig. 20.16
Chronic overload stress of the medial collateral ligament. (a) Coronal 12-5 MHz US shows thick medial collateral ligament (arrows) and (b) frontal radiograph also shows old avulsion of the sublime tubercle (asterisk)
Stress radiographs can be used to evaluate MCL insufficiency . A side-to-side difference of >0.5 mm in the joint space was consistent with a MCL tear (Rijke et al. 1994), and in throwing athletes differences of ≥2 mm in the ulnohumeral joint space required MCL reconstruction (Thompson et al. 2001).
US shows thickened hypoechoic MCL, with effusion near the medial epicondyle (Jacobson and van Holsbeeck 1998). In chronic cases calcifications and heterotopic bone can be seen (Conway et al. 1992) (Fig. 20.17).
Fig. 20.17
Medial collateral ligament. (a) Longitudinal 12-5 MHz US of the normal, homogeneous echo pattern of the medial collateral ligament (arrow) which connects the medial epicondyle with the sublime tubercle of the ulna. (b) Longitudinal 12-5 MHz US of the chronic overuse syndrome with thick medial collateral ligament (arrows) showing a small origin calcification and low echogenicity of the intra-articular fat (asterisk)
Complete tears are presented as a hypoechoic gap. In throwing athletes, a dynamic valgus stress ultrasound examination can estimate medial joint laxity as well as stage partial tears (Nazarian et al. 2003). CT arthrography presents extravasations of the arthrography contrast beyond the medial aspect of the joint capsule indicating MCL injury. Posteromedial degenerative changes as olecranon osteophytes and loose bodies are best visualised with CT (Fig. 20.18).
Fig. 20.18
Posterior elbow impingement. (a) Axial and (b) sagittal 2D CT reconstruction shows posterior elbow impingement with osteophyte formation (arrows)
MRI has an important role in preoperative staging for ligamentoplasty in partial ligament tears in throwing athletes. Normal MCL has a uniform low signal intensity and fat signal deep to its fibres which reflect normal intra-articular fat (Nakanishi et al 1996) (Fig. 20.19).
Fig. 20.19
Medial collateral ligament. (a) Coronal T1-weighted SE MR image shows homogeneous low signal intensity MCL with high signal intensity deep to it representing normal intra-articular fat (arrow). (b) Coronal T1-weighted SE MR image and (c) coronal T2-WI FS MRI image show thickened MCL with reduced SI on T1-WI and increased SI on T2-WI of the intra-articular fat (arrow)
Partial distal MCL tears do show a “T sign” on MR arthrogram corresponding to an extension of the contrast between the distal MCL and the sublime tubercle, to >3 mm continuous with the contrast in the joint to form a “T”. Other MRI findings are thickened ligament with high signal intensity on T1 and PD weight images (Fig. 20.15a), traction spur, discontinuity of the MCL in complete tears with extravasation of the contrast, and, if applicable, associated medial and lateral impaction/impingement changes as the bone bruises lateral and secondary degenerative changes posteromedial.
20.7 Lateral Collateral Ligament Complex Injury
The lateral collateral ligament complex (LCLC) consists of the radial collateral ligament , lateral ulnar collateral ligament (LUCL), and the annular ligament (Figs. 20.20 and 20.21).
Fig. 20.20
The lateral collateral ligament (LCL). (a) Longitudinal 12-5 MHz US of the LCL in a chronic overuse syndrome with thick LCL (arrows) and proximal calcifications (curved arrow). (b) LCL reconstruction (arrows) from lateral epicondyle (asterisks) till the radius head (asterisk)
Fig. 20.21
T1-W coronal T1 MR image of a normal LUCL (arrows)
Injury of the lateral collateral ligament complex is a result of chronic varus stress overload in sports or work-related activities or from acute trauma with posterior dislocation, hyperextension, or varus stress (Safran 2004). This leads to posterolateral rotatory instability (PLRI). The pathoanatomy of the PLRI develops through three stages according to the “circle of Horii ”(O’Driscoll 2000):
Stage I – disruption of the LUCL resulting in posterolateral rotatory subluxation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree