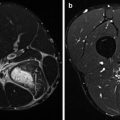
Fig. 34.1
Plantaris. In patients with a painful nodular thickening in the Achilles tendon, the pain is often most prominent on the medial side of the midportion Achilles tendon. At this level, the plantaris tendon runs closely with and parallel to the Achilles tendon and can have circular adhesions as seen in this endoscopic image (a before release, b after adhesiolysis).
The plantaris muscle-tendon complex not only causes flexion but also inversion, whereas the triceps surae is a flexor only. Adhesions between both tendons obstruct the opposite forces of these two bi- and triarticular muscle groups. Although the movement between the two will be limited, traction onto the surrounding paratenon will take place with every step with a mean of 5,000–12,500 steps/day in people with a low active to active lifestyle (Tudor-Locke and Bassett 2004; Tudor-Locke et al. 2008). Chronic painful tendons have been shown to exhibit new ingrowth of sensory nerve fibres from the paratenon (Schubert et al. 2005). Repetitive traction onto this richly innervated area might contribute to the medially located pain and stiffness during and after walking.
34.2.3.3 Clinical Presentation and Evaluation
It is hypothesised that the main cause of the pain in patients with symptomatic midportion Achilles tendinopathy does not arise from the tendon proper but is generated by its surrounding tissues.
Symptoms of a patient with midportion Achilles tendinopathy include painful swelling typically 2–7 cm proximal to the insertion and stiffness especially when getting up after a period of rest. Pain is the main symptom in Achilles tendinopathy that leads a patient to seek medical help. It is often most prominent 2–7 cm from the insertion onto the calcaneus on the medial side (Segesser et al. 1995; van Sterkenburg and van Dijk 2011). Tendinopathy and paratendinopathy often coexist (Saxena 1995; van Sterkenburg and van Dijk 2011). Intratendinous changes most often remain asymptomatic (Kannus and Józsa 1991). In these cases, a painless swelling at 2–7 cm proximal to the insertion is the only finding. In isolated paratendinopathy, there is local thickening of the paratenon. The area of swelling does not move with dorsiflexion and plantar flexion of the ankle, where it does in isolated tendinopathy (Steenstra and van Dijk 2006; van Sterkenburg and van Dijk 2011). Paratendinopathy can be acute or chronic. Acute isolated paratendinopathy manifests itself as painful peritendinous crepitus as the tendon glides within the inflamed covering. Areas of increased erythema, local heat and asymptomatic palpable tendon nodules or defects may also be present at clinical examination. In chronic paratendinopathy, exercise-induced pain is the main symptom while crepitation and swelling diminish.
It has been described that the location of the pain in patients with Achilles tendinopathy is most often located on the medial side (Segesser et al. 1995; Steenstra and van Dijk 2006; van Sterkenburg and van Dijk 2011). During Achilles tendoscopy in patients with Achilles tendinopathy, it has been observed that at the level of complaints, the plantaris tendon is affixed onto the Achilles tendon on the medial side (19) (Fig. 34.1). Some authors describe a higher medial stress onto the Achilles tendon due to hyperpronation. This is supported by the finding that most ultrasonographic midportion disorders (91 %) are found in the posteromedial segment of the tendon (Gibbon et al. 2000; de Jonge et al. 2011a).
34.2.4 Flexor Hallucis Longus Tendon
Flexor hallucis longus (FHL) tendinopathy is a typical injury in ballet dancers. It is characterised by posteromedial located pain, especially at relevée and grand plié. During active or passive flexion movements of the first toe with the ankle in 10–20° plantar flexion, the moving FHL can be palpated posterior to the medial malleolus. With tendinopathy there is pain on palpation and active resistance testing. Crepitus might be present and is suggestive for FHL tenosynovitis. Flexor hallucis longus tendinopathy is frequently seen together with the posterior ankle impingement syndrome.
34.2.5 Peroneus Tendon
This is the most common cause of posterolateral ankle pain in athletes. Most athletes will present with a history of ankle sprains. Posterolateral-located clicking sensations are suggestive for peroneal tendon luxations. Athletes with a varus hindfoot and/or restricted range of motion (ROM) of the subtalar joint are more prone to peroneal tendon overload. Pain on palpation is found just posterior to the lateral malleolus and can extent more distally. Swelling and slightly increased skin temperature might be present and should be compared to the contralateral site. Peroneal luxations should be tested by active resisted eversion. The tendon will luxate laterally and anteriorly.
34.2.6 Tibialis Posterior Tendon
Athletes with a clear pes planovalgus or with a forefoot abduction are prone to place greater strain on the muscle (Rabbito et al. 2011). Posteromedial palpation will reveal tenderness, discrete swelling and occasionally crepitus. Resisted supinations provoke the pain.
34.3 Achilles Tendon Ruptures
34.3.1 Epidemiology
Achilles tendon rupture occurs relatively common (de Jonge et al. 2011b). Although it is the thickest and strongest tendon in the human body, it remains susceptible to injury. During the last decades, the incidence of spontaneous ruptures has been rising, which may be due to the increasing keep-fit culture. Ruptures occur most frequently in patients between the age of 30 and 50 years old, with a male predominance. Approximately 75 % of Achilles tendon ruptures occur during sports activities, especially racket games, soccer and handball. Diagnosis is clinical. However, there is still a lack of consensus on the best management of the Achilles tendon rupture. Generally, open operative management is used, although over the past few years, percutaneous techniques are performed more commonly. Conservative management seems to be a good alternative for those with great co-morbidity or patients who do not wish to have surgery. Recent systematic reviews have concluded that operative management has a lower re-rupture rate but must be balanced by the risks associated with surgery (Khan and Carey Smith 2010).
34.3.2 Functional Anatomy
The Achilles tendon consists of the fibres of two muscle units in the superficial compartment of the posterior leg: the gastrocnemius muscle (medial and lateral head) and the soleus muscle. At about the level where the soleus contributes fibres to the Achilles tendon, rotation of the tendon begins and becomes more marked in the distal 5–6 cm. This rotation results in a relatively hypovascular area. The Achilles tendon inserts crescent-shaped halfway the posterior tuberosity of the calcaneus (Lohrer et al. 2008). The blood supply to the tendon is poor, and there is decrease in its nutrition with advancing age. Unlike other tendons in the leg, the Achilles tendon is a type 1 tendon that lacks a synovial sheath. Instead, it has a paratenon, which is an array of thin connective tissue containing blood vessels (Saxena and Bareither 2001). Together with the bone-tendon and the muscle-tendon junction, the paratenon forms the sole vascular supply of the Achilles tendon. A recurrent branch of the posterior peroneal artery mostly supplies the paratenon, whereas the peroneal artery makes small contributions.
The sural nerve is located to the lateral border of the Achilles tendon at its midportion, but many variations have been described (Apaydin et al. 2009). It is especially vulnerable to iatrogenic damage, most often Achilles tendon surgery, resulting in hypo- or hyperaesthesia of the lateral side of the affected foot.
34.3.3 Aetiology and Injury Mechanism
There is little agreement on the aetiology of spontaneous Achilles tendon ruptures. Several hypotheses have been proposed, such as poor tendon vascularity, the adverse effect of the use of corticosteroids and fluoroquinolones and exercise-induced hyperthermia in a relatively avascular tendon. Mechanical factors such as overpronation of the foot on heel strike, training errors, malfunction or suppression of propriocepsis of skeletal muscle have also been suggested. Histologically, spontaneously ruptured Achilles tendons might show degeneration of the fibres near the rupture site. There is a decrease in the maximum diameter and density of collagen fibrils. However, there is little evidence of a failed healing response. Aetiology is probably multifactorial.
The mechanism of injury includes a sudden pushing off from the weight-bearing forefoot with the knee in extension, unexpected ankle dorsiflexion and violent dorsiflexion of a plantar-flexed foot (Arner and Lindholm 1959).
34.3.3.1 Clinical Presentation and Evaluation
Achilles tendon rupture is a clinical diagnosis. Patients report sudden intense pain in the midportion of the Achilles tendon, often stating that someone might have struck their heel. On clinical examination, a positive calf squeeze test, the so-called Thompson test, and a gap in the Achilles tendon are consistently found. If any diagnostic doubt still exists, the next step is to perform ultrasonography of the tendon and its insertion.
34.4 Ligament Injuries
34.4.1 Acute Lateral Ankle Ligament Injuries
34.4.1.1 Epidemiology
Injury to the lateral ligament complex of the ankle is a common problem in the emergency department. It is estimated that 1 ankle sprain occurs per 10,000 people per day. Overall, injuries of the lateral ligament complex of the ankle form a quarter of all sports injuries. Some sports (e.g. basketball, soccer and volleyball) have a particularly high incidence of ankle injuries (Lindenfeld et al. 1994; Luidinga and Rogmans 1985). The treatment of inversion injuries is performed by emergency and primary health-care physicians as well as by orthopaedic and trauma surgeons (Kannus and Renström 1991). The total annual cost to society for ankle injuries has been estimated to be approximately 40 million Euro per 1 million people.
34.4.1.2 Functional Anatomy
Together, the anterior talofibular, calcaneofibular and posterior talofibular form the lateral ligament complex of the ankle. The anterior and posterior talofibular ligaments run horizontally from the lateral malleolus to the talus and are capsular ligaments that represent discrete thickenings of the ankle joint capsule. The calcaneofibular ligament runs from the fibula down- and backwards directly to the calcaneus and is extracapsular, and in close approximation to the inferior sheath of the peroneal tendons, it is regarded a stabiliser of the ankle (talocrural) and subtalar joints.
Relevant nerves for the ankle originate from the lower lumbar and higher sacral spinal roots (L4–S2). Efferent fibres of the deep peroneal nerve innervate the anterior muscles of the leg, the superficial peroneal nerve innervates the peroneal muscles on the lateral side and the tibial nerve innervates the muscles on the posterior side of the leg. The afferent path consists of all nerves that send proprioceptive information from mechanoreceptors around the ankle to the central nervous system.
34.4.1.3 Aetiology and Injury Mechanism
There are predisposing factors for sustaining an acute lateral ligament injury. A high longitudinal arch, greater foot width, cavovarus deformity, gait on the lateral side of the foot and congenital joint hypermobility have been described.
The most common mechanism of injury is supination and adduction (usually referred to as inversion) of the plantar-flexed foot (Lauge-Hansen 1949). In sports involving jumping, a major cause of lateral ligament injury is a player landing on the foot of an opponent; in contact sports, most injuries occur during tackling where the opponent hits the medial side of the lower leg, causing outward rotation of the knee and forcing the ankle into an inverted position. It is known that the anterior talofibular ligament is the first ligament to crack and is torn in 97 % of cases (Broström 1965; Steenstra and van Dijk 2006; Verhagen et al. 1995). The subsequent ligament to crack is the calcaneofibular ligament; indeed isolated rupture of the calcaneofibular ligament occurs in only 3 %. Brostrom found that combined ruptures of the anterior talofibular ligament and the calcaneofibular ligament occurred in 20 % of the cases (Broström 1965). The last ligament to crack is the posterior talofibular ligament which is usually uninjured unless there is a frank dislocation of the ankle.
34.4.1.4 Clinical Presentation and Evaluation
On presentation, patients mostly recall the accident as a twisting injury to their ankle and present with pain and swelling. Differentiation between an ankle fracture and a lateral ligament rupture is not always easy. The Ottawa ankle decision rules are helpful in saving unnecessary radiographic investigation in about 30 % of cases, using bony tenderness and inability to bear weight as positive indicators for radiography (Stiell et al. 1993). When no osseous injury is present, the degree of injury can traditionally be graded I to III (Bernett and Schirmann 1979). Grade I is a mild stretching of the ligament without instability, grade II is a partial rupture with mild instability of the joint (such as isolated rupture of the anterior talofibular ligament) and grade III involves complete rupture of the ligaments with instability of the joint. Due to the strong character of pain and swelling, the patient will contract the muscles around the ankle, which hinder reliable anterior drawer testing. It has become a common practice to wait a few days; to advice the patient according to the rest, ice, compression and elevation (RICE) protocol; and to perform a delayed physical examination after 5–7 days. Swelling, local tenderness, a positive anterior drawer test and hematoma indicate the presence of a lateral ligament rupture.
34.4.2 Chronic Lateral Ankle Ligament Injuries/Instability
Although surgical treatment for acute injuries of the lateral ankle ligaments probably gives slightly better functional results than conservative treatment, it is unclear whether this compensates for a higher risk of complications, higher costs and required operation time (Kerkhoffs et al. 2007; Pijnenburg et al. 2000). Conservative treatment leads to full functional recovery in most people. However, up to 20 % continue to suffer from lateral ankle instability, characterised by recurrent ankle sprains or a feeling of apprehension in the ankle (giving way). If this persists for longer than 6 months, the term ‘chronic (lateral) ankle instability’ (CAI) is used (Karlsson et al. 1996).
34.4.2.1 Aetiology and Injury Mechanism
Prior to the 1960s, it was assumed that chronic ankle instability was mechanical in origin, resulting from structural laxity of the injured ankle ligaments. This ‘mechanical instability’ (MI) can be assessed by physical and radiological examination, using the anterior drawer test and the ankle inversion test (Karlsson et al. 1996). However, it is now clear that chronic ankle instability may occur with or without increased ligament laxity. Increased ligament laxity does not always result in symptomatic instability. These observations have led to the concept that functional instability (FI) resulting from a neuromuscular deficit is implicated along with mechanical instability in people with symptoms of chronic ankle instability (Halasi et al. 2005; Hertel 2002; Hubbard et al. 2007).
34.4.2.2 Clinical Presentation and Evaluation
The diagnosis is based on the patient’s history. Pure lateral instability is characterised by recurrent inversion sprains or giving way as the main symptom. Pain and swelling may accompany an episode of recurrent spraining but is not present in between. The location of pain gives an indication of what structure is affected. Deep ankle pain on weight-bearing fits the diagnosis of an osteochondral defect. In long-standing ankle instability, there are signs of posttraumatic osteoarthritis of the talocrural joint. Duration of symptoms should be evaluated, as 6 months is more or less the time for rehabilitation of an acute lateral ligament injury. It is important to clarify the type of physiotherapy a patient has had, e.g. whether instability training has been performed. The use of ankle supports gives an idea of the severity of the instability. Furthermore, level of sports and work should be assessed, as compared to pre-injury levels.
Gait and stance examination may show a lateral gait or a cavovarus foot that predisposes for inversion injuries. General swelling indicates intra-articular pathology or recent injury. Range of motion of the ankle and subtalar joints should be assessed for pain, crepitus, restrictions and locking. The ankle region should be carefully palpated for tenderness. Increased laxity of the lateral ligaments is best tested with the anterior drawer test, comparing it to the contralateral side.
For lateral ankle ligament instability, plain ankle radiographs (AP, lateral and mortise) are usually sufficient to rule out displaced fractures; it is important to recognise that in 30 % of cases, occult fractures, i.e. not visible on radiographs, are described in literature. Ankle stress radiographs may help to confirm mechanical instability but have a low sensitivity and positive predictive value. Stress radiographs are mostly used in research, to quantify the effect of a (surgical) treatment. The clinical application remains questionable. Additional investigation is usually not part of clinical practice.
34.4.3 Acute Medial Ankle Ligament Injuries
34.4.3.1 Functional Anatomy
The deltoid ligament inserts from the medial malleolus and attaches to the medial talus, calcaneus and navicular bone. It can be differentiated into the anterior tibiotalar ligament, the tibiocalcaneal ligament, the posterior tibiotalar ligament and the tibionavicular ligament. The deltoid ligament is a strong ligament and less frequently injured than the lateral ligaments.
34.4.3.2 Aetiology and Injury Mechanism
The classical injury mechanism of a deltoid ligament lesion is forced eversion of the foot, such as a direct trauma to the lateral aspect of the foot and ankle (Hintermann et al. 2006). It is relatively uncommon that an inversion trauma induces combined lateral ligament injury and deltoid lesions.
34.4.3.3 Clinical Presentation and Evaluation
Physical examination reveals swelling and pain on palpation of the medial ligament with signs of talar subluxation in complete lesions. Standard radiographs are frequently normal. The sensitivity of MRI to detect deltoid lesions is high (Schneck et al. 1992). However, there is a risk of overdiagnosing deltoid ligament lesions – deltoid ligament abnormalities after a classical inversion trauma (with lateral ligaments injuries) are reported to be present in 60 % of the cases, but this frequently does not align with the clinical findings.
The therapy of deltoid lesions is dependent on associated injuries, such as syndesmotic injuries and ankle fractures. Combined lateral and deltoid ligament injuries can frequently be treated in the same manner as a lateral ligament injury. Simple isolated deltoid sprains can be treated with functional treatment. Isolated deltoid ruptures are mostly treated conservatively by 4–6 weeks of immobilisation and progressive rehabilitation; however, high-level athletes can be advised to consider a surgical option.
34.4.4 Syndesmotic Injury
34.4.4.1 Epidemiology
Injuries to the distal tibiofibular syndesmosis can range from stable minor sprains to significant fractures of the distal fibula with combined syndesmotic disruption; they are typically related to eversion-type ankle injury. When compared with its clinical disability, a syndesmotic injury presents worse than a typical lateral ankle sprain. When patients present with a classic ankle sprain, it is noted that up to 18 % of them also suffer from a syndesmotic lesion.
34.4.4.2 Functional Anatomy
The syndesmosis consists of the anterior and posterior inferior tibiofibular ligament and the interosseous tibiofibular ligament. The inferior transverse tibiofibular ligament is sometimes considered as a fourth ligament, but it is not a separate structure, since it is really a continuation of the distal aspect of the posterior inferior tibiofibular ligament. In almost 75 % of the cases, there are contact facets with articular cartilage jointing the distal tibia and fibula, forming a true synovial joint.
The posterior inferior tibiofibular ligament provides approximately 40 % of the resistance towards lateral displacement, the anterior inferior tibiofibular ligament 35 % and the interosseous ligament 22 %. The remaining stability is provided by the interosseous membrane.
34.4.4.3 Aetiology and Injury Mechanism
The mechanism of injury in a syndesmotic sprain can be an isolated hyperdorsiflexion force, but it occurs most commonly due to an external rotation injury, in combination with axial loading of the ankle. However, in patients with a combined deltoid injury or medial malleolar fracture, an abduction force is mainly the cause of the associated syndesmotic lesion.
Isolated total ruptures are relatively infrequent, and acute syndesmotic injuries have been reported especially in football and skiing.
34.4.4.4 Clinical Presentation and Evaluation
Direct palpation pain onto the syndesmosis and more proximally is the key to a good clinical assessment. It is also important to check the entire fibula up to the knee for any suspected syndesmotic injury. Swelling is much less noted in a syndesmotic injury when compared with a traditional ankle sprain, and the ecchymosis is usually more proximal to the ankle joint compared with a usually more distally localised ecchymosis in a lateral ankle sprain (Kerkhoffs et al. 2012; McCollum et al. 2013).
The test is performed by stabilising the leg with the knee flexed at 90° and then rotating the foot externally. When acutely injured, this test will elicit pain at the syndesmosis. Other tests to determine the integrity of the syndesmotic ligaments are the squeeze test, the cotton test and the fibular translation test. The cotton test and the fibular translation tests are more useful for chronic syndesmotic lesions (McCollum et al. 2013).
During a squeeze test, the examiner grasps the supine patient’s middle part of the tibia and fibula and applies compression and release motion. A positive test is considered if the patient experiences pain in the syndesmotic area. The cotton test can be performed by steadying the distal leg with one hand while grasping the plantar heel with the opposite hand and moving the heel directly from side to side.
Any lateral translation during this test indicates potential syndesmotic instability. The fibular translation manoeuvre tests anteroposterior pain and stability of the distal fibula.
During physical examination, it is important to palpate the medial ankle in addition to determine the integrity of the deltoid ligament, since it can highlight a more significant unstable syndesmotic injury.
Imaging
A mortise or AP and lateral weight-bearing radiograph should be used to evaluate the tibiofibular clear space and to rule out any ankle fracture. Also stress radiographs are recommended. With these ‘conventional’ diagnostics, still syndesmotic ligament injuries easily can be missed. For this reason, magnetic resonance imaging (MRI) is recommended, which has been reported to have a sensitivity and specificity of, respectively, 95 and 90%.
When performing a mortise view, 1 mm overlap or more is predictive of an intact syndesmosis.
The use of stress radiographs, compared with the contralateral side, is essential when plain radiographs are equivocal. Imaging modalities with advanced ultrasound of the anterior tibiofibular ligament, bone scan and arthrography have been used in the assessment of syndesmotic injuries, but magnetic resonance imaging provides a more accurate evaluation of the ligamentous anatomy of the syndesmosis, since MRI demonstrates also the posterior inferior tibiofibular ligament and can nicely elucidate associated injuries such as deltoid ligament injuries, bone bruises, fractures and osteochondral injuries. Arthrography has demonstrated a high sensitivity of 90 % with a specificity of 67 % when performed within 48 h after trauma. However, arthrography has – in most instances – been replaced by MRI since it is expected to have a similar high sensitivity and specificity, and MRI has the advantage of being a non-invasive technique.
In summary, distal syndesmotic sprains are related to eversion-type ankle injury and are less frequent than typical lateral ankle sprains that are related to inversion-type ankle injury, but they are easily recognised when associated with a fracture of the fibula at the level of the distal metaphysic or diaphysis.
Increased awareness and a thorough history, clinical examination and detailed radiographic evaluation including the whole length of the diaphysis and distal syndesmotic sprains – not associated with a fracture – can be astutely diagnosed following the appropriate above-mentioned reasonable guidelines.
34.5 Ankle Impingement Syndromes
34.5.1 Anterior Ankle Impingement
34.5.1.1 Epidemiology
One of the most common causes of chronic anterior ankle pain in athletes is the anterior ankle impingement syndrome. The anterior ankle impingement syndrome is typically characterised by anteriorly located ankle pain, which increases by forced hyperdorsiflexion.
It can be differentiated in soft tissue and bony impingement.
34.5.1.2 Aetiology and Injury Mechanism
Contrary to other joints, osteophytic formation of articular cartilage can typically develop in athletes without pathologic changes of the weight-bearing articular cartilage and should therefore be differentiated from osteophytes in degenerative osteoarthritis. It is questionable if the osteophytes develop due to repetitive capsular traction during hyper-plantar flexion movements. Post-ankle trauma cartilage damage and subsequently recurrent instability are supposed to enhance the osteophytic formation. In football and soccer players, the osteophytes are a manifestation of anterior medial ankle contact trauma in combination with recurrent kicking of the ball (Tol and van Dijk 2004; Tol et al. 2002).
The cause of pain is hypothesised to be due not to the osteophyte itself, but it is the inflamed soft tissue impingement that occurs between the osteophytes (Cheng and Ferkel 1998; McMurray 1950). During forced dorsiflexion movements, this soft tissue component gets squeezed between the anterior distal tibia and the talus. Recurrent trauma to this soft tissue component may lead to hypertrophy of the synovial layer, subsynovial fibrotic tissue formation and infiltration of inflammatory cells. In theory, arthroscopic excision of the soft tissue could relieve pain. Talar and tibial osteophytes, however, decline the anterior space, and compression of this soft tissue component is more likely to occur (van Dijk et al. 1997; Tol et al. 2001).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree