The role for neuroimaging in the management of patients with tremor is gradually increasing, particularly with respect to stereotactic neurosurgery and deep brain stimulation where less than 2-mm tolerance is required for accurate electrode placement. The routine use of single photon emission CT technology to image the nigrostriatal dopaminergic system is proving helpful in distinguishing essential and dystonic tremors from neurodegenerative forms of parkinsonism and in improving our understanding of the pathophysiology of rarer tremors.
Standard magnetic resonance (MR) and CT imaging has had a limited role in the routine management of tremulous patients except mainly for people with Holmes tremor syndrome and other secondary causes of tremor (multiple sclerosis or Wilson disease).
The new millennium has seen the introduction of single photon emission CT (SPECT) imaging techniques, particularly 123 I-FP-CIT (iodine 123-labelled N-ω-fluoropropyl-2β-carbomethoxy-3β-[4-iodophenyl]nortropane) SPECT (DaTSCAN), into routine clinical practice as a means of assessing the integrity of the nigrostriatal dopaminergic system in patients with tremor. Care is required in the analysis of DaTSCAN scans, which can be reported visually; semiquantitatively, using a region of interest approach; or quantitatively, using statistical parametric mapping. Furthermore, caution should be exercised when interpreting an abnormal DaTSCAN result and scan findings should be compared to clinical signs to determine whether or not they are congruous.
The introduction of first 18 F-dopa ([fluorine-18] fluorodopa) positron emission tomography (PET) and then DaTSCAN scanning into clinical trial work has even led to a new class of “parkinsonian” patient termed a subject with a scan without evidence of dopaminergic deficits (SWEDDs). These patients have subsequently been carefully assessed and preliminary information indicates that many of these SWEDDs patients have underlying dystonic tremor syndromes, an area of considerable clinical interest.
Essential tremor
Classical essential tremor consists of a bilateral, visible, persistent, and largely symmetrical postural and/or kinetic tremor involving the hands and forearms. Essential tremor should not be diagnosed in the presence of other abnormal signs, except for subtle cognitive deficits and mildly impaired tandem gait, which have been documented in some cases. Routine CT and MR imaging of patients with essential tremor have not shown any consistent abnormalities, whilst voxel-based morphometry revealed adaptive changes in brain structure but no signs of cerebellar degeneration in essential tremor. In addition, diffusion-weighted imaging of patients with essential tremor found no differences in any of the regions of interest compared with healthy control subjects. DaTSCAN studies demonstrate similar results in essential tremor to those for healthy control subjects, making it possible to distinguish essential tremor from Parkinson disease, as tracer uptake into the putamen and caudate is abnormal in the latter. In a phase III multicenter study of DaTSCAN involving 158 patients with a clinical diagnosis of parkinsonism, 27 with essential tremor, and 35 healthy volunteers, the sensitivity for parkinsonism was 95% and specificity for essential tremor 93% (based on a consensus blinded read by a five-person panel). Thus current experience indicates that DaTSCAN is a valuable tool in the differentiation of essential tremor from Parkinson disease ( Fig. 1 ).

PET and functional MR imaging studies have demonstrated bilateral activation in the cerebellum, red nucleus, and thalamus of patients with essential tremor, meanwhile, two 1 H-MRS (proton MR spectroscopy) studies have indicated that there is a selective reduction of the neuronal marker N-acetyl-aspartate in the cerebellum of essential tremor patients, in keeping with a converging view that a disturbance of the corticocerebellothalmocortical loop is the pathophysiological mechanism underlying essential tremor.
Using 123 I-metaiodobenzylguanidine (MIBG) cardiac scintigraphy, abnormalities have been recently detected in patients with Parkinson disease. However, this technique revealed no abnormalities in essential tremor patients.
A difficult clinical scenario involves patients with long-standing essential tremor (decades) who then develop features of parkinsonism. The issue then arises as to whether mild parkinsonian features are manifestations of long-standing essential tremor, superimposed age-related changes, or Parkinson disease that has developed on top of essential tremor. Hensman and colleagues (2006) evaluated the role of DaTSCAN imaging in 20 patients with essential tremor and features of parkinsonism and found that 50%had abnormal scans ( Fig. 2 ). The clinical features of these patients were similar to those with normal DaTSCANs except that they had rest-tremor magnitudes that exceeded that of their intention tremors or had bradykinesia, rest tremor, and rigidity.
Isolated rest tremors and long-duration asymmetric postural tremors
Patients with isolated unilateral tremor, without other features of parkinsonism, provide a difficult diagnostic problem. These patients could have a dystonic tremor syndrome; a highly atypical variant of essential tremor, which is classically symmetric; or benign tremulous Parkinson disease. A 18 F-dopa PET study involving 8 patients with hereditary essential tremor, 12 with sporadic essential tremor, and 11 with predominantly rest tremor demonstrated normal tracer uptake into the putamen in all the hereditary and 10 of the 12 sporadic essential tremor cases. However, in all the patients with rest tremor, there was a marked reduction of the 18 F-dopa influx constant (Ki) to levels associated with Parkinson disease.
A long-term study of 13 patients originally presenting with an asymmetric postural tremor (diagnosed as “essential tremor” with or without mild rest tremor) revealed that these patients subsequently developed Parkinson disease. The clinical findings were supported in 5 of the 13 patients using β-CIT (Iodine 123 labelled 2β-carboxymethyl-3β-[4-iodophenyl]tropane) SPECT, indicating that at least some cases of “essential tremor” do develop Parkinson disease. However, the study was subject to bias because the development of Parkinson disease was an entry criterion for the study. More recently, a study clarified this issue showing that about 50% of essential tremor patients who developed features of parkinsonism have abnormal DaTSCAN scans, suggesting that either they have had underlying Parkinson disease or have developed Parkinson disease. However, 40% had normal DaTSCAN imaging and in 20% the scan was equivocal.
Isolated rest tremors and long-duration asymmetric postural tremors
Patients with isolated unilateral tremor, without other features of parkinsonism, provide a difficult diagnostic problem. These patients could have a dystonic tremor syndrome; a highly atypical variant of essential tremor, which is classically symmetric; or benign tremulous Parkinson disease. A 18 F-dopa PET study involving 8 patients with hereditary essential tremor, 12 with sporadic essential tremor, and 11 with predominantly rest tremor demonstrated normal tracer uptake into the putamen in all the hereditary and 10 of the 12 sporadic essential tremor cases. However, in all the patients with rest tremor, there was a marked reduction of the 18 F-dopa influx constant (Ki) to levels associated with Parkinson disease.
A long-term study of 13 patients originally presenting with an asymmetric postural tremor (diagnosed as “essential tremor” with or without mild rest tremor) revealed that these patients subsequently developed Parkinson disease. The clinical findings were supported in 5 of the 13 patients using β-CIT (Iodine 123 labelled 2β-carboxymethyl-3β-[4-iodophenyl]tropane) SPECT, indicating that at least some cases of “essential tremor” do develop Parkinson disease. However, the study was subject to bias because the development of Parkinson disease was an entry criterion for the study. More recently, a study clarified this issue showing that about 50% of essential tremor patients who developed features of parkinsonism have abnormal DaTSCAN scans, suggesting that either they have had underlying Parkinson disease or have developed Parkinson disease. However, 40% had normal DaTSCAN imaging and in 20% the scan was equivocal.
Dystonic tremor syndromes
Tremor is often apparent in patients with primary or secondary dystonia. It is termed dystonic tremor if the tremor occurs in a body part also affected by dystonia and tremor associated with dystonia when tremor occurs in a body part not affected by dystonia but dystonia is present elsewhere. These two types of tremor commonly coexist in patients with a dystonic tremor syndrome.
In the primary dystonic tremor syndromes, routine cerebral MR and CT imaging are usually normal. Although dystonic tremor and tremor associated with dystonia are typically action tremors, with a tendency to enhance during attempts to perform fine manual tasks, these conditions can cause a rest tremor and a clinical picture that resembles Parkinson disease. Some patients with a dystonic tremor have parkinsonian signs that include hypomimia, reduced arm swing, asymmetric rest and postural tremor, increased limb tone, and abnormally slow and small repetitive finger movements. Consequently, differentiation of patients with dystonic tremor syndromes from those with Parkinson disease becomes an important clinical issue. Perhaps this is where DaTSCAN imaging can be particularly helpful, as it is abnormal in Parkinson disease and reported normal in the dystonic tremor syndromes.
Dystonic tremor may be associated with an underlying condition (eg, Wilson disease [see below]) or, rarely, a structural cerebral lesion, as in the case of a focal parietal lesion (posttraumatic cerebromalacia) reported to result in dystonic head tremor and an anterior thalamic infarct contralateral dystonic hand tremor.
Subjects with scans without evidence of dopaminergic deficits
Four to fifteen percent of patients entered into several randomized trials of dopaminergic medication for Parkinson disease were found to have normal presynaptic nigrostriatal dopaminergic imaging and were termed SWEDDs . These patients had several features of parkinsonism that had lead neurologists to not only diagnose but to enter these patients into randomized controlled trials involving medical treatments for Parkinson disease. However, dopaminergic imaging of these patients, up to 4 years later, was normal and withdrawal of levodopa had no deleterious effect on their clinical state. Consequently, this has led to considerable interest about the nature of the condition or conditions underlying these SWEDDs patients.
Recently, data has emerged that at least some of these SWEDDs patients have dystonic tremor and that this had been misdiagnosed as Parkinson disease. However, whether this proves to be the case for the majority of SWEDDs patients remains to be seen.
Primary orthostatic tremor
Primary orthostatic tremor is a high-frequency tremor that predominantly involves the legs and trunk whilst in the standing position. Electrophysiology plays a major role in the diagnosis of orthostatic tremor as it has a characteristic frequency (13–18 Hz). Four modalities of imaging have been used to investigate orthostatic tremor: PET, SPECT, MR imaging, and transcranial sonography. The interpretation of both sonography and functional imaging depends on whether primary orthostatic tremor is thought to be associated with dopaminergic deficit: a controversial topic.
In a study of four patients with primary orthostatic tremor in which PET was coregistered with MR imaging, bilateral cerebellar hemisphere activation and significant activation of the cerebellar vermis, left lentiform nucleus, and left thalamus were detected. The investigators postulated that cerebellar activation is a feature common to all tremors, and that tremors may be associated with overactivity of a common circuit involving cerebellothalamic connections.
Functional imaging of the nigrostriatal dopaminergic pathway using DaTSCAN has in some studies suggested that orthostatic tremor was associated with a dopaminergic deficit and hence changes on SPECT. However, recent reports indicate that this is not always the case. Katzenschlager and colleagues detected a dopaminergic deficit in orthostatic tremor. This was more evenly distributed than in Parkinson disease and affected all parts of the striatum nearly evenly. They found that, unlike in Parkinson disease, there was no correlation between the extent or distribution of tracer uptake and disease duration or severity. However, it is possible that there was some suppression of tracer uptake, as these patients were on co-beneldopa prior to investigation. Nevertheless, the investigators suggest that a presynaptic dopaminergic deficit is unlikely to be the primary underlying cause of the pathophysiology of orthostatic tremor and speculate that a central primary generator causes orthostatic tremor and a modulation of the dopaminergic system. In this regard, Trocello and colleagues found no significant difference between the controls and patients with orthostatic tremor and postulate that there are different subtypes of orthostatic tremor:
Type A—without dopaminergic loss
Type B—with mild dopaminergic loss without parkinsonian symptoms
Type C—orthostatic tremor associated with Parkinson disease
The concept of a disease spectrum in orthostatic tremor is supported by the variable response of patients to levodopa.
No MR image changes characteristic of orthostatic tremor have been described. In a study of the clinical and neurophysiologic findings in 26 subjects with orthostatic tremor, 13 patients had MR imaging scans. Of these 13 cases, the MR image scans were normal in 9, showed microvascular ischemic disease in 2, an old infarct in the right posterior temporoparietal lobe in 1, and mild diffuse atrophy in 1.
A transcranial sonographic study of four orthostatic tremor patients found hyperechogenic substantia nigra, a finding that also occurs in Parkinson disease.
Neuropathic tremor
Neuropathic tremor is most commonly seen in patients with demyelinating peripheral neuropathies. It is usually a postural or kinetic tremor affecting distal rather than proximal muscles. It is most frequently seen in patients with IgM demyelinating paraproteinaemic neuropathy. These patients had normal cerebral MR imaging and most had normal central motor conduction times assessed with magnetic brain stimulation.
Detailed neurophysiological studies of patients with IgM demyelinating paraproteinaemic neuropathy have suggested that tremor arises because a central processor is misled by distorted mistimed peripheral inputs into producing tremor. PET activation studies have shown that the cerebellar hemispheres are hyperactive bilaterally, both during tremor and at rest, in these patients. There are no other reports of detectable abnormalities on neuroimaging of patients with neuropathic tremor.
Drug-induced tremors
Tremors occur in the context of drug-induced parkinsonism (DIP), which may result from centrally acting antiemetics and antipsychotics. Differentiating DIP from Parkinson disease can be difficult, particularly as clinical descriptions of DIP differ. Postsynaptic imaging shows D2 receptor blockade and it was expected that presynaptic imaging would be normal, as found in three DIP patients. However, in one DaTSCAN study, 5 of 7 patients with a differential diagnosis of DIP versus Parkinson disease had abnormal scans. In another report, 11 of 20 patients with DIP had abnormal scans, which were characterized by diminished binding in the caudate and putamen. Reversibility of parkinsonism after neuroleptic withdrawal is variable and three clinical scenarios have been proposed:
DIP with no relationship to Parkinson disease
DIP that unmasks Parkinson disease
DIP that antedates Parkinson disease
The latter two scenarios may account for the dopaminergic deficits described.
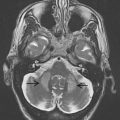
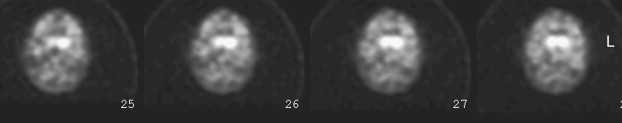
Holmes tremor syndrome
Holmes tremor syndrome has in the past been labeled rubral tremor , midbrain tremor , thalamic tremor , myorythmia , and Benedikt syndrome . It is named after Gordon Holmes, who first gave an accurate description of the characteristics of this type of tremor. It may arise from various underlying structural disorders, including stroke, vascular malformations, tumors, nonketotic hyperglycemia, and infections (eg, herpes simplex type 1 cerebral pedunculitis or a toxoplasma abscess in the context of HIV). It is rarely present in multiple sclerosis, which tends to induce an action tremor. In Holmes tremor syndromes, the lesions are most usually sited in the midbrain ( Fig. 3 ), although lesions in the thalamus have also been described. There is a variable delay (typically 2 weeks to 2 years) between that lesion and the first appearance of Holmes tremor, which often involves proximal and distal upper limb muscles and consists of an irregular low-frequency (<4.5 Hz) rest and intention tremor and, in many cases, a postural tremor. DaTSCAN and 18 F-dopa PET studies have demonstrated reduced tracer uptake in the ipsilateral putamen and caudate nuclei ( Fig. 4 ), and current evidence suggests that, in most cases, Holmes tremor arises from lesions that interrupt the dentate-thalamic and also the nigrostriatal tracts, thus causing both an action and a rest tremor.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree