Figs. 32.1 and 32.2
SI Joint intra-articular injection before and after 1-ml nonionic contrast injection
In order to reduce the incidence of false-positives, it is appropriate to consider a series of SI joint blocks. In a prospective study of 67 patients with unilateral LBP, SI joint-compatible referral patterns, and joint tenderness, Maigne et al. [21] investigated the prevalence of SI joint pain using a series of blocks with two different local anesthetics. Of the 54 patients who completed the study, 19 obtained ≥75 % pain relief with the lidocaine screening block. After the confirmatory block with bupivacaine, only 10 of the 19 patients achieved ≥75 % pain relief lasting 2 or more hours, resulting in a prevalence rate of 18.5 %. The false-positive rate of 17 % in this study is less than that previously reported for lumbar facet blocks [59]. Since there is not another methodology to serve as a diagnostic “gold standard,” we cannot determine the true sensitivity or specificity of intra-articular blocks. However, from a practical standpoint, with a low-risk profile of SI joint blocks, it is appropriate to proceed with this methodology and base treatment plans from the information gleaned. It is important to point out that while a series of blocks to demonstrate a consistent response may represent an ideal, it also incurs increased costs and an increased length of time until the patient is adequately treated.
Treatment
Non-interventional management of SI joint pain may include the use of shoe inserts to address leg length discrepancies as well as physical therapy and osteopathic or chiropractic manipulation to address altered gait mechanics and spine malalignment [60, 61]. However, there are no prospective, controlled studies supporting these modalities. Nonsurgical stabilization programs have been advocated including the application of pelvic belts that reduce the sagittal rotation of presumed incompetent SI joints in pregnant women [62, 63] to exercise-induced pelvic stabilization programs [64]. Ankylosing spondylitis (AS), an inflammatory rheumatic disease with spine and SI joint involvement that manifests as spondylitis and sacroiliitis, has been treated with pharmacologic approaches, but the results are muddled due to systemic involvement and cannot give specific conclusions as to the SI joints.
Intra-articular injections with steroid and LA can serve the dual function of being therapeutic and aiding in diagnosis. It is beneficial to blind the patient to the local anesthetic chosen, use a pain diary to assess the first phase response to local anesthetic, and then assess the second phase response to the anti-inflammatory effect of the steroid. Controlled studies demonstrate good relief for a majority of patients from a single dose of fluoro-guided intra-articular or periarticular steroid 1–2 months after injection, with a limited number of individuals still showing benefit at 3 or 6 months. Prospective observational studies of image-guided SI joint injections to demonstrate good to excellent pain relief lasting from 6 months to 1 year. As with any pharmacologic treatment, the length of duration of response to a single-dose steroid is less of a function of the effectiveness of the drug but rather an issue of how long other factors cause symptomatic inflammation to recur. Therefore, the decision to utilize steroid injections as a long-term treatment plan depends on the interval needed to maintain improvement, quality of relief, and potential adverse effects related to the cumulative dose of corticosteroids.
Radiofrequency Denervation Procedures
Radiofrequency (RF) denervation procedures are utilized to provide prolonged pain relief to patients with injection-confirmed SI joint pain. The techniques used have ranged from denervating the joint by performing intra-articular lesions, lesioning the lateral branches that provide a portion of the SI joint innervation [65–68], to the combination of ligamentous as well as neural RF ablation [69]. All of the techniques described cannot completely denervate the SI joint, and an analysis of the methodology of the techniques is important to place the published success rates in proper perspective as well as provide insight as how to possibly improve results. It is important to remember that percutaneous RF denervation procedures should not be expected to alleviate pain emanating from the ventral SI joint. In one study [20], ventral capsular pathology was shown to account for 69 % of all CT pathology in the 13 patients with a positive response to diagnostic SI joint blocks. Also, nociceptors have been confirmed to exist on the ligamentous tissue and likely need to be addressed as well (Table 32.1).
Table 32.1
Published clinical studies of radiofrequency treatment of sacroiliac joint pain
Author, year | Technique | Study design | N | Treatment | Outcomes | Key details |
|---|---|---|---|---|---|---|
Ferrante et al. (2001) [68] | Intra-articular | Retrospective | 33 (50 joints) | Multiple, 90 °C, 90-s lesions at approx. 1-cm intervals | At 6 months, 36.4 % had >50 % pain relief, average duration of responders was 12 months | Only the postero-inferior joint was lesioned |
Cohen and Abdi (2003) [65] | Lateral branch | Retrospective | 18 (9 underwent RF) | 80 °C, 90-s lesions of L4 and L5 dorsal rami and S1–S3 lateral branches | 13/18 had 50 % pain relief from prognostic blocks, 8/9 of RF-treated patients had >50 % pain relief at 9 months | Criteria for RF treatment were >50 % pain relief from prognostic blocks |
Yin et al. (2003) [67] | Lateral branch | Retrospective | 14 | 80 °C, 60-s lesions of L5 dorsal ramus and variably the S1–S3 lateral branches | At 6 months, 64 % had >50 % pain relief, 36 % had complete relief | Criteria for RF treatment were >70 % pain relief after 2 separate SI joint deep interosseous ligament injections |
Cohen et al. (2009) [79] | Lateral branch | Retrospective | 77 | 80 °C, 90-s lesions of L4 and L5 dorsal rami and S1–S3 lateral branches | At 6 months, 52 % had ≥50 % pain relief | Criteria for RF treatment were >50 % pain relief from intra-articular SI joint block. Limitations include variable technique (conventional and cooled RF treatments) |
Burnham and Yasui (2007) [80] | Lateral branch | Prospective | 9 | 3 conventional lesions at L5 and 3 bipolar strip lesions for S1–S3 dorsal rami | 67 % success rate at both 6 months and at 12 months | Criteria for RF treatment were >50 % pain relief for both an SI joint block and a prognostic lateral branch block |
Cohen et al. (2008) [81] | Lateral branch | Randomized, placebo controlled | 28 | Conventional lesions at L4 and L5 and cooled probable lesions at S1 and S2, and some at S3 or S4 | At 6 months, 57 % had >50 % pain relief, 14 % success at 12 months | Criteria for RF treatment were >75 % pain relief from SI joint block |
Only 14 % of control patients had relief at 1 month, none beyond that | ||||||
Buijs et al. (2004) | Lateral branch | Prospective observational | 38 (43 joints) | 80 °C, 60-s lesions of S1–S3 lateral branches in all subjects, and L4–L5 dorsal rami in half of subjects | At 12 weeks, complete pain relief at 34.9 % sites and >50 % pain relief at 32.6 % sites | Criteria for RF treatment were >50 % pain relief from SI joint blocks. No difference in outcomes with or without L4 and L5 lesions |
Vallejo et al. (2006) [82] | Pulsed RF of lateral branches | Prospective | 22 | 39–42 °C, pulsed RF lesions of L4 and L5 medial branches and S1–S2 lateral branches | 16 patients (73 %) had >50 % pain relief for a short time: 6–9 weeks (4 patients), 10–16 weeks (5 patients), 17–32 weeks (7 patients) | Criteria for RF treatment were >75 % pain relief after >2 SI joint injections |
Kapural et al. (2008) [83] | Cooled RF | Retrospective case series | 26 | Lesion at L5 and 2–3 lesions at S1–S3 | At 3–4 months, 50 % had >50 % pain relief | Criteria for RF treatment were 2 SI joint blocks with >50 % pain relief |
Gevargez et al. (2002) [69] | CT-guided RF lesion of L5 dorsal ramus and posterior interosseous SI ligaments | Prospective observational | 38 | 90 °C, 90-s lesions | At 3 months, 34.2 % were pain-free, 31.6 % reported substantial decrease in pain | Criteria for RF treatment were response to CT-guided SI joint injections |
Intra-articular Approach
The first study of RF denervation of the SI joint utilized the intra-articular approach. In this study, 33 patients were treated, some on both sides, for a total of 50 joints. The patients underwent diagnostic SI joint injections to determine eligibility. RF lesions were performed with a bipolar technique with probes placed approximately 1 cm apart and leapfrogged for each lesion. Patients were assessed for VAS scores, pain diagrams, physical exam changes, and change in opioid consumption. A successful result was defined as a ≥50 % decrease in VAS for at least 6 months. With this definition, 36.4 % were considered responders, and in this group, the average duration of response was 12 months and also demonstrated a normalization of SI joint pain provocation tests as well as a reduction in opioid consumption. An in vitro study suggests that success rates could be improved upon by reducing the distance between the cannulae when performing bipolar RF lesions, as spacing the cannulae 4–6 mm apart maximized the surface area of the lesion [70]. Another factor to take into consideration is that when bipolar lesioning is performed, the power output is regulated to maintain the desired temperature at one of the cannulae, and there is often a difference in the temperature achieved at the other cannula, often being 5–10° lower, which also affects the size of the area lesioned. Therefore, monopolar lesions placed closely together may provide a more consistent result.
Lateral Branch Approach
This technique involves lesioning of the L4 and L5 dorsal rami as well as the lateral branches from S1 to S3 (or S4). Studies utilizing this approach have some variability as to the methods and results. Retrospective studies had a range of results including one with 8 of 9 patients with ≥50 % relief after 9 months and another with 64 % of 14 patients achieving >50 % relief at 6 months. A larger retrospective study had 52 % of 77 patients achieve at least 50 % relief at 6 months, but had variability in technique, as conventional as well as cooled RF treatments were included. The prospective studies performed are all very small in size (n = 9, 28) and had success rates at 6 months at 67 and 57 %, respectively. Another prospective study reported success rates as high as 70 % in 38 patients, but only reported results at 3 months post-procedure (Fig. 32.3).
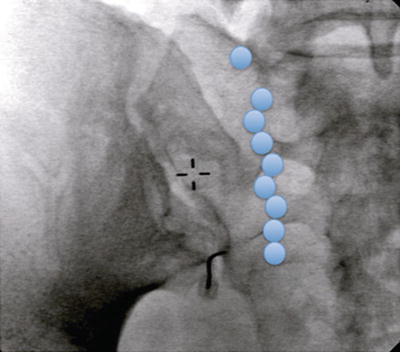
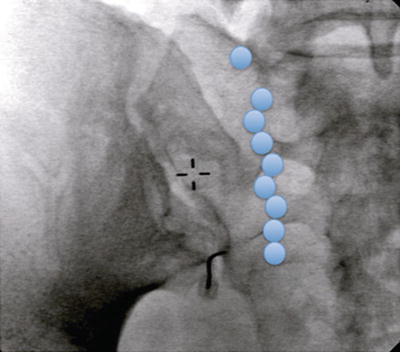
Fig. 32.3
Lesion sites on the sacrum for the lateral branch approach (sites for L5 dorsal rami and lateral branches from S1 to S3 are marked in blue)
Emerging Concepts
Other techniques which have been reported on a limited basis in the literature include a prospective trial in 22 patients of pulsed RF lesions from 39 to 42 °C of the L4 and L5 medial branches and the S1 and S2 lateral branches. A >50 % reduction in pain was achieved in 73 % of patients for a short time. Only seven patients had relief that lasted from 17 to 32 weeks. A retrospective case series of 26 patients was reported using cooled RF probes with the theoretical benefit of achieving larger sized lesions. In this study, lesions were performed at L5 and 2–3 lesions at the S1–S3 neuroforamina. This technique had 50 % of the patients achieve ≥50 % relief at 3–4 months posttreatment. There are no other reports to date that have investigated outcome at 6 months or greater. Gervagez et al. [69] utilized CT-guided RF treatment with denervation of the L5 dorsal ramus and the interosseous SI ligaments at three locations in 38 patients. After 3 months, 34.2 % of patients were pain-free, and 31.6 % had a substantial decrease in pain.
Conclusions
The SI joint is a common cause of axial low back pain which may also radiate to the hips, groin, and posteriorly to the knee in up to 30 % of patients. Historical and physical examination findings have limited reliability as tools in the diagnosis of SI joint pain, thus diagnostic blocks remain the most commonly used method for diagnosing this disorder. While there may be debate as to validity of utilizing injections as a diagnostic tool, they are useful as a prognostic tool prior to performing denervation treatments. Intraarticular and periarticular corticosteroid injections have been shown to provide benefit lasting from 1 month to 1 year in patients with and without spondylarthropathy [71–78]. Like any pharmacologic treatment, this is less a function of the duration of action of the corticosteroid but rather a reflection of the variability of recurrence of inflammation. Over the last decade, the emergence of RF denervation techniques has provided a useful option in providing longer lasting relief in patients with SI joint pain. All of the techniques described only partly denervate the SI joint and the surrounding tissue with nociceptors and can be improved upon. The concept of bipolar strip lesioning has been found to require close proximity of probe placement, which at that distance will provide equivalent lesions with monopolar lesioning at the same interval. Future research will need to be done to determine if success rates may be improved upon by utilizing this methodology to more completely denervate both the articular joint as well as the ligamentous nociceptors. This could be promising as responders to this approach have been documented to maintain benefits for at least 1 year. RF lesioning of the lateral branches results in a successful outcome in slightly greater than 50 % of patients, but follow-up has been limited, and longer term studies are needed. Pulsed radiofrequency lesioning has been unimpressive for this indication. The utilization of emerging tools to create larger lesions may simplify the denervation of a large target region but needs to be more fully investigated in regard to safety.
References
1.
Bernard TN, Cassidy JD. The sacroiliac syndrome. Pathophysiology, diagnosis and management. In: Frymoyer JW, editor. The adult spine: principles and practice. New York: Raven; 1991. p. 2107–30.
2.
3.
Ruch WJ. Atlas of common subluxations of the human spine and pelvis. Boca Raton: CRC Press; 1997.