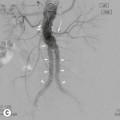
Nicholas Gourtsoyiannis, Panos Prassopoulos, Maria Daskalogiannaki, Patrick McLaughlin, Michael M. Maher The duodenum measures 20–30 cm in length. It forms an incomplete circle surrounding the head of the pancreas and is described as having first, second, third and fourth parts. The first (superior) part contains the duodenal cap or bulb and passes superiorly, posteriorly and to the right before turning down to become the second part. Posteriorly it is devoid of peritoneum. The second (descending) portion passes down anterior to the right kidney and posterior to the transverse colon. Above and below the transverse colon it is covered with peritoneum. The duodenum turns to the left and passes horizontally in front of the spine as the third (horizontal) part before it ascends in front and to the left of the aorta as the fourth (ascending) part to end at the duodenojejunal flexure (ligament of Treitz). At barium examination, parallel, or nearly parallel, folds are seen passing upwards from the base of the duodenal cap. They are effaced when the hypotonic duodenum is distended by gas at double-contrast barium examination. The mucosa of the remainder of the duodenum is thrown into numerous folds that disappear on distension. The circular folds, termed valvulae conniventes, are permanent; they begin in the second part of the duodenum and extend throughout the small intestine. The ampulla of Vater can be seen in 65% of patients during routine double-contrast barium examination and the accessory papilla of Santorini’s duct (also known as the minor duodenal papilla) in 25%. The ampulla of Vater is recognised by its fold pattern: a hooded fold and a distal longitudinal fold are usual, and oblique folds are frequently present. The accessory papilla is sited about 10 mm proximal to the ampulla. On a prone view the ampulla lies on the medial wall and the accessory papilla on the anterior wall. The barium examination is the principal radiological technique for examining the duodenal lumen, although the technique has largely been replaced by endoscopy. It is easier to detect abnormalities if the duodenum is relaxed. Hypotonia is produced by IV injection of 20 mg of hyoscine butylbromide (Buscopan) or 0.2 mg of glucagon. With the table horizontal, the patient is first turned onto their right side so that barium fills the duodenum. The patient is next rotated onto their left side and gas passes rapidly from the stomach into the duodenum. Then, with the patient in the right anterior oblique position, a number of double-contrast views of the duodenal cap and duodenal loop (Fig. 28-1) are taken. Water-soluble contrast medium should be used in patients with suspected perforation of the stomach or duodenum. The examination is best performed under fluoroscopic control; alternatively, a right decubitus radiograph is taken after a short interval. Hypotonic duodenography is performed by placing a duodenal catheter in the lower part of the descending duodenum and injecting about 40 mL of barium suspension. The smooth muscle relaxant is then injected intravenously and air is injected through the catheter to distend the duodenum and radiographs of the duodenal loop are taken. Angiography can be invaluable in the diagnosis of acute duodenal haemorrhage, when endoscopy has failed to locate the bleeding site. Ultrasound (US) and computed tomography (CT) are used to evaluate secondary involvement of the duodenum by malignant disease and CT may also be helpful in assessing the extent of duodenal neoplasms. On double-contrast barium examination, duodenal ulcer craters are shown as sharply defined, constant collections of barium (Fig. 28-2), sometimes with a surrounding zone of oedema or radiating folds. Anterior wall ulcers are normally shown best on the prone view. Postbulbar ulcers are occasionally seen, mostly on the concave border of the second part or in the immediate postbulbar area. The ulcer is shown as a typical crater, frequently with spasm of the opposite wall. There may be narrowing of the lumen and thickening of the mucosal folds. In some cases scar formation may obscure the ulcer crater. Postbulbar ulcers usually fail to heal on medical treatment. The principal complications of duodenal ulceration are perforation, bleeding, stenosis and penetration of adjacent organs. Free perforation is usually diagnosed on the clinical and plain radiographic findings. Occasionally, a water-soluble contrast examination may be necessary to confirm the diagnosis. The perforation is sometimes localised or ‘walled-off’ with marked deformity of the duodenum due to the adjacent inflammatory reaction. Bleeding caused by duodenal ulceration is diagnosed by endoscopy and/or angiography. Duodenal stenosis may become quite marked and result in obstruction. Barium examination in this situation will show an excessive amount of fluid in a dilated stomach with considerable delay in emptying. Gastric heterotopia is present in a small percentage of normal people. Irregular filling defects, varying in size from 1 to 6 mm, are seen in the duodenal cap extending from the pylorus distally (Fig. 28-3). Gastric heterotopia should be differentiated from lymphoid hyperplasia of the duodenal bulb, which usually requires endoscopy. Duodenal diverticula are present in 2–5% of barium studies; most are an incidental finding. They are usually in the descending part of the duodenum, with 85% arising from the medial surface (Fig. 28-4). Frequently they are in contact with the pancreas and may be embedded in its surface. Occasionally, a diverticulum contains aberrant pancreatic, gastric, or other functioning tissue and is the site of ulceration, perforation, or gangrene. Symptoms may also develop due to the retention of food or a foreign body. Cholangitis or pancreatitis may result from the aberrant insertion of the common bile duct or pancreatic duct into an intraluminal diverticulum. Benign neoplasms of the duodenum are uncommon and often symptomless. Brunner’s gland hyperplasia is seen as single or multiple polypoid lesions in the first part of the duodenum (Fig. 28-5), often with a characteristic cobblestone appearance. Patients usually present with typical symptoms of peptic ulceration. A single Brunner’s gland adenoma is occasionally seen. Adenomatous polyps feature as solitary, mostly sessile, polypoid, intraluminal filling defects on barium studies, or as soft-tissue masses on CT. Villous adenomas exhibit a characteristic ‘cauliflower’ or ‘soap bubble’ appearance on barium studies, caused by the trapping of barium in the crevices between the multiple frond-like projections of the tumour. Benign lymphoid hyperplasia is an occasional finding shown as multiple small rounded filling defects of uniform size (Fig. 28-6). Other benign neoplasms of the duodenum include periampullary adenomas (Fig. 28-7), gastrointestinal stromal tumours (GISTs), lipomas (Fig. 28-8) and neurogenic tumours or hamartomas exhibiting the same features as in the small intestine. Carcinoma of the papilla of Vater (also known as the ampulla of Vater) is the type most frequently encountered, usually presenting with jaundice. Barium studies show an enlarged papilla of Vater with irregular borders, sometimes with spiculation and ulceration. Non-papillary carcinomas of the duodenum are adenocarcinomas and usually present clinically as duodenal obstruction. Barium examination shows the neoplasm as an ulcerative, polypoid or annular lesion. On CT, primary carcinomas are seen mostly as focal masses with asymmetric mural thickening with varying degrees of luminal narrowing (Fig. 28-9). Coincident adenopathy or hepatic metastases may be present. Other malignant primary neoplasms occasionally encountered in the duodenum include GISTs and lymphomas. The duodenum may be invaded by malignant neoplasms from adjacent organs or be the site of metastases. Carcinoma and lymphoma of the stomach can spread directly across the pylorus to involve the duodenum. This is reported to occur in up to 40% of lymphomas and 25% of adenocarcinomas of the gastric antrum.1 Carcinoma of the head of the pancreas frequently causes changes in the duodenal loop. There may be widening of the duodenal loop, a double contour, irregularity of the inner border and stricturing or distortion of the valvulae conniventes. Carcinoma of the tail of the pancreas may compress or invade the duodenum, resulting in mucosal destruction, which may ultimately result in bleeding or obstruction clinically. Duodenal ileus may be seen on plain radiographs in acute pancreatitis. Mucosal oedema, enlargement of the duodenal loop and enlargement of the papilla of Vater are characteristic findings on barium studies. The duodenum is affected in about 4% of patients with Crohn’s disease. The radiological appearances are similar to those in the more distal parts of the small intestine. The valvulae conniventes are frequently thickened. At a more advanced stage of the disease, there may be strictures with eccentric or concentric narrowing. Cobblestoning, asymmetry and skip lesions may be seen but fissure ulcers, sinuses and fistulae are uncommon in the duodenum. The disease may cause tubular narrowing of the antrum and proximal duodenum in continuity (Fig. 28-10), resulting in the ‘pseudo post-Billroth I’ appearance. Tuberculosis of the duodenum is rare. Barium studies show narrowing of the lumen, sometimes with destruction of the mucosa and ulceration, mostly involving the descending duodenum. Tuberculous mesenteric lymphadenitis, in the absence of intrinsic duodenal tuberculosis, may produce extrinsic pressure on the duodenum and cause obstruction. In patients with neuromuscular disorders, particularly progressive systemic sclerosis and visceral myopathy, the duodenum is frequently involved. There may be dilatation, which is often more pronounced in the second, third and fourth parts. The dilated duodenum may be slow to empty and the grossly dilated, atonic organ may produce a sump effect. The most common cause of intramural haematoma is blunt abdominal trauma. Intramural haematoma is usually seen on barium studies as a concentric obstructive lesion in the duodenum. Infiltration of blood and oedema may result in thickening of the valvulae conniventes. CT shows the extent of the haematoma, seen as a large mixed-attenuation mass, surrounding the duodenum (Fig. 28-11). The most frequent site of rupture is at the junction of the second and third parts of the duodenum. CT is the primary imaging technique for assessment. Imaging findings include retroperitoneal air adjacent to the duodenum, extravasation of oral contrast in the retroperitoneum, oedema in the duodenal wall and stranding in the peripancreatic fat.1 Abdominal aortic aneurysms may compress the third part of the duodenum and they occasionally cause obstruction. The duodenum, when faintly opacified with oral contrast medium and stretched around an aneurysm, may be misinterpreted as a contained leak or as a patch of perianeurysmal inflammation. Aortoenteric fistulae most often involve the duodenum, particularly the third part of the duodenum. An aortoenteric fistula should always be suspected in patients who have undergone aortic graft surgery and present with gastrointestinal haemorrhage. The superior mesenteric artery compression syndrome is a rare form of high intestinal obstruction, which is believed to be caused by narrowing of the normal angle between the aorta and superior mesenteric artery. Strong to-and-fro peristalsis and duodenal dilatation may be seen during a symptomatic episode on barium meal examination. Superior mesenteric artery compression is seen as a sharp cut-off in the right anterior oblique position, with the compression and proximal dilatation persisting in the prone position. MDCT is useful to define the distance between aorta and superior mesenteric artery. Duodenal varices are encountered occasionally in the duodenal cap and loop. They occur mainly in patients with extrahepatic portal hypertension, but may occur in portal hypertension without evidence of extrahepatic obstruction. The small intestine measures approximately 5 m in length and extends from the duodenojejunal flexure to the ileocaecal valve. It is attached by its mesentery to the posterior abdominal wall and this allows it to be mobile. The proximal two-fifths constitute the jejunum and the distal three-fifths the ileum. The jejunum lies mainly in the left upper and lower quadrants and the ileum in the lower abdomen and the right iliac fossa. The jejunal and ileal branches of the superior mesenteric artery provide the blood supply. Normally the small intestine is in a collapsed or partially collapsed state. Its calibre diminishes as it passes distally. During peristalsis the maximum diameter of the jejunal loops is 4 cm and of the ileal loops 3 cm. The valvulae conniventes have a circular configuration and are about 2 mm thick in the distended jejunum, becoming more spiral shaped and about 1 mm thick in the ileum. They may be absent in the distended terminal ileum, resulting in a rather featureless outline. Compared to the upper gastrointestinal tract and large bowel, the small intestine is much less amenable to examination with endoscopy, and as a result, radiological investigations play a pivotal role in the diagnosis of small intestinal disease. CT, MRI, barium and US examinations all have a role in the assessment and diagnosis of small intestinal pathology. In many circumstances each of the aforementioned modalities may be used in a complementary fashion. The choice of initial examination will depend on the clinical issue in question. Plain abdominal radiography often has a limited role. Angiography and nuclear medicine studies can be of value in selected cases. Patients who present acutely with suspected perforation or obstruction of the small intestine are investigated initially with plain abdominal radiographs. The barium follow-through is performed following a barium meal examination of the oesophagus, stomach and duodenum. The small bowel meal is a modification of the follow-through, which specifically focuses on the small intestine. Five hundred millilitres of a 30–40% weight/volume suspension of barium sulphate is given to the patient, who is encouraged to drink it as fast as possible. Cold water is used in the preparation of the suspension to stimulate gastric emptying and reduce transit time. Full-length prone radiographs are exposed at 10, 30 and 60 min. All segments of the small intestine are examined fluoroscopically and compression is applied. Barium introduced directly into the small intestine gives excellent visualisation by challenging the distensibility of intestinal loops, thereby making it easier to identify the presence of morphological abnormalities. The technique the current authors use is similar to Sellink’s method.2 A 10 French (10Fr) radio-opaque Nolan tube (William Cook Europe A/S) is passed via the nasogastric route to the duodenum so that its tip lies at or just distal to the duodenojejunal flexure, or preferably 5–10 cm into the jejunum. A total of 800–1200 mL of barium suspension diluted to 20% weight/volume is infused, using a pump, at about 75 mL min−1. Radiographs of the barium-filled jejunum and ileum are then taken (Fig. 28-12). Double-contrast methods have been employed successfully, including the air-contrast method and by using barium suspension followed by an aqueous suspension of methylcellulose. Detailed mucosal changes, particularly small ulcers, are well shown by the air-contrast method. However, as air does not distend the intestine as well as dilute barium, sinuses and fistulae are often not demonstrated and stenoses may be overlooked. CT is becoming increasingly important in evaluating mural and extramural lesions and in assessing mesenteric involvement and ancillary intra-abdominal findings associated with inflammatory or neoplastic small intestinal diseases. Careful choice of CT imaging and reconstruction technique is vital to the identification and characterisation of small intestinal abnormalities. Maximising the spatial and contrast resolution by acquiring isotropic multiplanar data sets with appropriate delivery of oral and intravenous contrast agents results in significantly improved diagnostic performance. Intravenous contrast administration is essential for a comprehensive CT examination of the small intestine. Peak enhancement of the small intestinal mucosa, known as the enteric phase, occurs approximately 50 s after intravenous injection or 14 s after peak aortic enhancement.3 Multiphase CT protocols, employing combinations of unenhanced, arterial, enteric and delayed phases, may be helpful in certain clinical situations such as the evaluation of intestinal bleeding.4 For routine CT imaging, opacification of the intestinal lumen is achieved using orally administered positive contrast material such as iodinated or dilute barium solutions, starting approximately 1 h prior to the examination. CT enterography involves the use of larger volumes of neutral Hounsfield unit (0–30 HU) oral contrast agents, ingested orally at a faster rate to distend the small intestine. Many neutral Hounsfield unit oral contrast agents have been described in the literature ranging from commercial products such as polyethylene glycol-based bowel preparation medications and VoLumen (Bracco Diagnostics, Princeton, NJ, USA), a low density (0.1%) barium sulphate solution to simpler solutions such as water or milk with or without the addition of bulking agents such as methylcellulose, locust bean gum and Mucofalk (Dr F. Pharma, Freiburg, Germany), a plant husk extract. Neutral oral contrast agents are gaining widespread acceptance and are more frequently used when a detailed CT study of the small bowel wall or mesenteric vessels is required. Although the site and severity of mucosal disease and mural enhancement patterns of the small intestine are much better assessed with neutral or negative oral contrast agents,5–7 positive enteric contrast agents remain valuable in patients with suspected perforation, abscess or extramural complications of Crohn’s disease and some authors also maintain that positive enteric contrast agents may also increase the conspicuity of cystic and subtle soft-tissue disease of the mesentery and peritoneum. Adequate distension of the small bowel improves the diagnostic accuracy of CT when neutral oral contrast agents are employed.7 CT enterography typically results in greater distension than routine oral preparation techniques but studies comparing CT enterography with CT enteroclysis demonstrate that absolute bowel distension is better when enteroclysis is performed.8–11 CT enteroclysis is performed by administering contrast medium directly into the small intestine through a nasojejunal tube (Fig. 28-13). Water or methylcellulose solution is typically used as a neutral luminal contrast agent but iodinated water-soluble contrast medium or a dilute barium solution can be used to provide positive luminal contrast. Although there are few comparative studies, diagnostic accuracy rates do not seem significantly different between CT enterography and CT enteroclysis, but a majority of studies report greater patient tolerance with CT enterography.8–11 Ultrasound does not employ ionising radiation and therefore is particularly useful when imaging young patients with Crohn’s disease who often require repetitive imaging procedures during the variable clinical course of this disease.12 Ultrasound of the small intestine requires high-frequency (5–17 MHz) linear array probes, which provide increased spatial resolution of the intestinal wall.13 Colour or power Doppler imaging and contrast-enhanced US (CEUS) provide more detailed information on mural and extraintestinal vascularity, which may reflect inflammatory disease activity.14 High-resolution ultrasonography is quick and non-invasive but diagnostic accuracy is dependent on operator experience. In clinical practice, US plays a rather limited role in the diagnosis and management of other small intestinal disorders but small intestinal obstruction can also be recognised and primary intestinal neoplasms may be identified using a dedicated US technique. MR imaging (MRI) provides excellent soft-tissue contrast and three-dimensional imaging capabilities, which are of importance when studying the small intestine. Prerequisites for a state-of-the-art MRI examination of the small intestine include adequate bowel distension, homogeneous intraluminal contrast and dynamic multiphase intravenous contrast enhancement. Imaging sequences should have a high temporal resolution to reduce bowel motion artefacts and, if required, cine sequences to facilitate the dynamic assessment of intestinal motility. Good spatial resolution is fundamental and allows adequate depiction of the bowel wall and perienteric soft tissues. These prerequisites can be provided by a comprehensive MR enteroclysis (MRE) examination protocol, which includes small bowel intubation, administration of a biphasic contrast agent, heavily T2-weighted (T2W) single-shot turbo spin-echo (SSTSE) images for MR fluoroscopy and for monitoring the infusion process, T2W imaging employing half-Fourier acquisition single-shot turbo spin-echo (HASTE) and true FISP sequences (Fig. 28-14), and dynamic T1-weighted (T1W) imaging using a post-gadolinium FLASH sequence with fat suppression (Fig. 28-15). This protocol can provide anatomic demonstration of the normal intestinal wall, identification of wall thickening and neoplasms, lesion characterisation and/or evaluation of disease activity, assessment of the extent of exoenteric/mesenteric disease and information concerning intestinal motility. Selective visceral angiography of the small intestine can detect the site of obscure bleeding when extensive barium studies and endoscopy are negative. It is also used to determine the bleeding site in patients who present with massive acute bleeding from the small intestine. In acute active bleeding angiography is successful when the rate of blood loss exceeds 0.5 mL min−1. Acute lower gastrointestinal bleeding is, however, frequently intermittent rather than continuous, resulting in a high rate of negative angiographic examinations. In the clinical context of acute active bleeding, it is important to avoid barium or other fluoroscopic studies using oral contrast agents before angiographic studies, as oral contrast will significantly impact the quality of the angiographic study. Nuclear medicine studies are useful alternative and adjunctive methods in the investigation of small bowel pathology. Leucocyte scintigraphy and FDG-PET are helpful in the diagnosis of suspected inflammatory bowel disease and/or the assessment of current disease activity. Older techniques, like pertechnetate scintigraphy for the detection of a Meckel’s diverticulum, have yet to be surpassed by more modern imaging methods. Scintigraphy with labelled red cells remains a useful examination for localisation of intestinal bleeding. Carcinoid tumours of the small bowel may be elegantly demonstrated by scintigraphy and PET techniques are already proving useful in small bowel oncology. Radionuclide scintigraphy, using 99mTc-pertechnetate, is a well-established non-invasive technique for identifying a Meckel’s diverticulum that contains gastric mucosa, as this agent is concentrated in the mucus-secreting cells and the parietal cells of the gastric mucosa in both the stomach and the diverticulum. The technique is more accurate in the paediatric age group than in adults. Crohn’s disease (CD) is a chronic relapsing immune-mediated inflammatory disorder that results from a dysregulated immune response to luminal antigens including normal intestinal bacterial flora in genetically susceptible individuals.15,16 A decrease in common intestinal infections in Westernised countries is accompanied by an increase in non-infectious inflammatory bowel diseases and the prevalence of CD in the USA has dramatically increased since the 1980s.17 There is a bimodal distribution of patient age at disease onset, with a large peak at 20 years and smaller peak at 50 years.18,19 CD often manifests with non-specific symptoms such as diarrhoea, weight loss and abdominal pain but specific clinical evidence of inflammatory bowel disease may be present in up to one-third of patients including signs of perianal fistulae, tags or fissures and aphthous ulceration.20 Abdominal pain and diarrhoea, often accompanied by weight loss, are the most frequent presenting symptoms. Patients may present with an ‘acute abdomen’, indistinguishable from acute appendicitis. Other presenting symptoms are anaemia, retardation of growth, anorexia and weight loss. Acute intestinal obstruction due to stenosis is occasionally the presenting symptom, as are fistulae, particularly fistula in ano. This chronic, progressive, transmural disease may affect any part of the gastrointestinal tract, but mostly involves the small intestine. The extent of involvement varies considerably but the terminal ileum is almost always affected. Approximately 15% of CD patients initially present with features of colitis alone and 35–45% of patients may develop perinanal complications over the course of their disease.17,19 Less commonly, CD patients may present with isolated gastroduodenal and jejunal disease and this pattern is more common in CD patients who present within the paediatric age range.21 In patients with previous right hemicolectomy for Crohn’s disease, the site of anastomosis in the small bowel represents the most common site of recurrence. The most characteristic feature of Crohn’s disease of the small intestine is the variety of its radiological appearances and the multiplicity of imaging features often seen in the majority of patients (Table 28-1). TABLE 28-1 Radiological Signs of Crohn’s Disease Aphthoid ulcers, which are a characteristic feature, are usually visualised as small collections of barium with surrounding radiolucent margins due to oedema. Fissure ulcers are seen in profile, may penetrate deep into the thickened intestinal wall and may lead to abscess formation at their base and/or to the development of sinuses and fistulae. Fistulae pass to adjacent loops of ileum, the caecum, the sigmoid colon or the urinary bladder and occasionally to the skin or the vagina. Longitudinal ulcers (Fig. 28-16) running along the mesenteric border of the ileum are a characteristic but infrequent sign of the disease process. Cobblestoning (Fig. 28-17) is fairly common and is caused by a combination of longitudinal and transverse ulceration, separating intact portions of mucosa. Narrowing of the intestinal lumen is frequent, as are strictures, which may be short, long, single or multiple, the latter being virtually diagnostic of Crohn’s disease. Solitary strictures (Fig. 28-18
The Duodenum and Small Intestine
The Duodenum
Anatomy and Normal Appearances
Radiological Investigation
Barium Studies
Other Imaging Techniques
Peptic Ulceration

Postbulbar Ulceration
Complications of Peptic Ulceration
Gastric Heterotopia
Diverticula
Neoplasms
Benign Neoplasms
Malignant Neoplasms
Primary Carcinoma
Secondary Involvement
Other Conditions
Pancreatitis
Crohn’s Disease
Tuberculosis
Progressive Systemic Sclerosis
Intramural Haematoma
Traumatic Rupture
Vascular Conditions
The Small Intestine
Anatomy and Normal Appearances
Radiological Investigation
Plain Radiographs
Barium Studies
Enteroclysis

Computed Tomography
Ultrasound
Magnetic Resonance Imaging
Angiography
Nuclear Medicine Studies
Radionuclide Imaging of Meckel’s Diverticulum
The Abnormal Small Intestine
Crohn’s Disease
Radiological Appearances

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Duodenum and Small Intestine
Chapter 28