Fig. 16.1
Juvenile Tillaux fracture in an 11-year-old boy. (a, b) There is a nondisplaced Salter-Harris III fracture, with the vertical epiphyseal fracture line (arrow) lateral to Kump bump (arrowhead). The physis anterolateral to Kump bump is widened
Salter-Harris I fractures are limited to young children, whose physes are still smooth; these fractures, along with Salter-Harris II fractures, are the most common distal tibia fractures in children (see Chap. 17 for further discussion of the Salter-Harris and Ogden classification systems). Salter-Harris II fractures tend to occur after age 10. Older children, who have an undulating or partly fused physis, are prone to more complex Salter-Harris fractures. Focal physeal fusion or undulation may alter fracture force propagation. Fractures propagate along the path of least resistance; therefore, the open physis is usually first to fail, rather than the metaphyseal or epiphyseal bone. Similarly, fractures are more likely to propagate along an open, smooth physis than along an undulating physis. Physeal fracture propagation will usually terminate at sites of undulation, such as Kump bump, or at sites where there is already bony physeal fusion. These areas resist transmission of force more than the open, smooth physis.
The juvenile Tillaux and triplane fractures are affected by the contour of the distal tibial physis (Box 16.1). Both of these fractures usually occur when the foot is in supination and subject to external rotational forces [4], usually during a fall. They are most common between ages 12 and 15, especially during the approximately 18-month transitional period when the distal tibial physis begins closure [5, 6].
Box 16.1: Tibial Fractures
Accompany about 25 % of fibular fractures |
Juvenile Tillaux and triplane fractures |
Twelve to fifteen years old, especially as distal tibial physeal closure begins |
Operative reduction if >2 mm displaced |
Juvenile Tillaux fracture (Salter-Harris III) |
Fracture through the anterolateral smooth distal tibial physis to Kump bump |
Vertical fracture line in the epiphysis anterolateral to Kump bump |
Distal tibial fragment may rotate |
Triplane fracture (Salter-Harris IV) |
At least three orthogonal planes; two-, three-, or four-part fractures (two-part most common) |
Classic two-part: sagittal in epiphysis, axial in physis, coronal in metaphysis |
Distal fibula also fractured in about 50 % |
The Salter-Harris III juvenile Tillaux fracture occurs in early adolescence and is most common in girls. The force initially propagates along the anterolateral smooth distal tibial physis. However, physeal fracture propagation stops at Kump bump, where the force deviates vertically into the epiphyseal bone anterolateral to Kump bump [6]. The older the child, the more lateral the epiphyseal fracture line, since more of the physis is fused. The anterior tibiofibular ligament inserts into the epiphyseal fragment, and therefore some degree of separation of the fracture fragments is common.
Triplane fractures are Salter-Harris IV fractures; the degree of physeal undulation and fusion affects propagation of this fracture and the resultant number of bone fragments. As a general rule, there is a sagittal component in the epiphysis, an axial component through the physis, and a coronal component in the metaphysis [5]. The distal fibula is fractured in about 50 % of cases.
Distal fibular physeal fractures have been described with any mechanism of injury. Tibial fractures accompany approximately 25 % of fibular fractures [7], so if there is a fibular fracture the tibia should be closely examined.
Periosteal avulsion fractures about the ankle may occur at the medial or lateral collateral ligament insertion sites (Fig. 16.2). These are frequently seen in skeletally immature children, in whom the periosteum where ligaments attach is less resilient than are ligaments and tendons [8]. Maisonneuve fractures result from pronation/external rotation of the ankle and consist of the combination of proximal tibial/tibiofibular injury and ligamentous injury at the medial ankle.


Fig. 16.2
Avulsion fracture at attachment site of anterior talofibular ligament in a 12-year-old girl. A thin, linear bone fragment (arrow) is separated from the talus
The objective of treatment of ankle physeal fractures is to avoid premature physeal fusion by minimizing the degree of physeal injury and displacement. If the epiphysis is involved, incongruity at the articular surface may lead to early osteoarthritis if left untreated. Therefore, the threshold for operative intervention is relatively low for epiphyseal fractures. In addition, Salter-Harris fractures may lead to physeal bars, especially those that are higher grade. When physeal bars are eccentrically located in the tibia, varus or valgus deformity of the ankle may result, whereas central physeal bars may lead to restricted growth without angular deformity [7].
Operative reduction is indicated for juvenile Tillaux and triplane fractures when the gap between fragments exceeds 2 mm [4]. If the gap is less than or equal to 2 mm, the fracture may be treated conservatively with 4 weeks of non-weight bearing with a long leg cast followed by 4 weeks of relative non-weight bearing in a boot [9]. Maisonneuve fractures are considered unstable and require operative reduction.
Imaging
Radiography is the first-line imaging in children with suspected ankle fractures. The Ottawa ankle rules have been validated in children over 5 years of age and are useful in limiting the number of unnecessary radiographic exams [10] (see Chap. 1). The Ottawa ankle rules recommend that radiographs should be ordered if the child complains of pain over the malleoli and if there is either bony tenderness along the distal 6 cm of the posterior edge of either malleolus or if the child cannot bear weight for four steps both immediately after the injury and at the time of clinical examination. The standard views for the ankle include frontal, mortise, and lateral views, preferably with weight bearing if the child is capable since this stresses the ankle and foot and may make subtle fractures more obvious.
Computed tomography (CT) is helpful for comprehensive delineation of the fracture pattern, particularly if operative reduction is planned. CT allows more accurate measurement of fracture displacement, assessment of articular surface congruity as well as location and extent of physeal involvement, and determination of the number and location of fracture fragments.
Salter-Harris I and II distal tibial and fibular fractures are the most common ankle fractures. It is important to search for a metaphyseal fragment or small flake (the so-called Thurston Holland fragment) in order to differentiate between a Salter-Harris I and a subtle Salter-Harris II. The degree of displacement and extent of physeal widening determine operative versus nonoperative management. Isolated Salter-Harris I and II fractures at the level of the distal fibular physis are not uncommon (Fig. 16.3).


Fig. 16.3
Salter-Harris I fracture of the distal fibula in a 13-year-old girl. There is extensive soft tissue swelling centered at the level of the widened fibular physis
It can be difficult to identify Salter-Harris I fractures of the distal fibula (or elsewhere). Isolated soft tissue swelling centered at the level of the open physis should be considered a Salter-Harris I fracture until proven otherwise (Fig. 16.3). However, in children younger than 10, the cartilaginous epiphysis of the medial or lateral malleolus may be confused with soft tissue swelling. If there is any question, comparison views of the asymptomatic distal fibula may help assess for physeal widening on the affected side.
The juvenile Tillaux fracture subgroup of distal tibial Salter-Harris III fractures has a vertical epiphyseal fracture line that is usually anterolateral to Kump bump (see Fig. 16.1) [9]. The older the child, the more lateral this vertical epiphyseal fracture line tends to be. The distal tibial epiphyseal fragment may rotate anterolaterally due to traction from the anterior syndesmosis (or tibiofibular ligament) at the level of the tibial plafond (Fig. 16.4). Although the anterolateral physis is fractured, it does not always appear widened.


Fig. 16.4
Juvenile Tillaux fracture in a 12-year-old girl. (a) There is a minimally displaced vertical epiphyseal fracture (arrowhead), and the lateral tibial physis is widened. (b) Axial computed tomography (CT) shows an avulsion injury with lateral rotation of the anterolateral tibial epiphyseal fracture fragment (arrow) due to traction from the anterior syndesmosis
The triplane subgroup of Salter-Harris IV fractures of the distal tibia must have at least three orthogonal fracture planes. These fractures can be divided into two-, three-, and even four-part fractures. Each category has several subtypes, which creates a confusing classification system [5]. Rather than trying to label these fractures according to their type and subtype, it is useful to define and describe the fracture components and extent of displacement. The two-part fracture is most common, followed by the three-part [11]. The classic two-part triplane fracture consists of a sagittal fracture plane through the tibial epiphysis, an axial fracture plane through the physis, and a coronal fracture plane through the metaphysis (Fig. 16.5). The posterolateral epiphyseal fracture fragment usually moves with the distal fibula, whereas the distal tibial epiphysis between the medial malleolus and Kump bump (or the anteromedially fused physis) follows the rest of the tibia. In younger patients, a three-part medial triplane fracture may have an axial fracture plane that extends through the anteromedial physis where Kump bump will develop. Once Kump bump appears, the medial fracture fragment in a three-part triplane fracture may include the medial epiphysis as well as Kump bump (Fig. 16.6).



Fig. 16.5
Two-part triplane fracture in a 14-year-old boy. (a, b) There is a vertical epiphyseal component (white arrow), an axial component extending through the plane of the physis (black arrow), and a metaphyseal oblique component (arrowhead). This is a Salter-Harris IV fracture

Fig. 16.6
Classic three-part triplane fracture in a 10-year-old girl. Axial (a), coronal (b), and sagittal (c) reformatted CT shows that the medial main fracture fragment includes the anteromedial epiphysis and Kump bump (arrowhead). The lateral physeal fracture (arrow) stops at Kump bump (arrowhead)
Additional fractures about the ankle include avulsion fractures related to the lateral collateral ligament, syndesmosis (anterior or posterior tibiofibular ligament) (see Fig. 16.4), and peroneal sheath. Lateral and medial avulsion fractures usually appear as sharply defined flecks of bone along the tibia or talus (see Fig. 16.2); these should not be confused with the normal fragmentary ossification pattern of the malleoli or accessory ossicles such as the os subfibulare, which are corticated and round or ovoid in shape.
The Maisonneuve fracture has several components (Box 16.2). There is a medial malleolar fracture or deltoid ligament injury (Fig. 16.7), along with injury to the syndesmosis and interosseous tibiofibular ligament, which results in widening of the medial tibiotalar joint. In addition, there is a proximal fibular fracture or proximal tibiofibular dislocation. Therefore, if the medial tibiotalar joint is widened or there is a medial malleolar fracture on ankle radiographs, radiographs of the upper tibia and fibula near the knee are recommended to evaluate for a concomitant proximal fibular fracture or proximal tibiofibular dislocation.
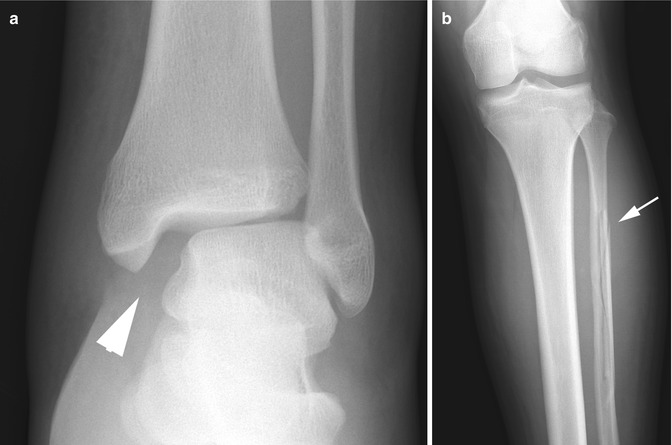
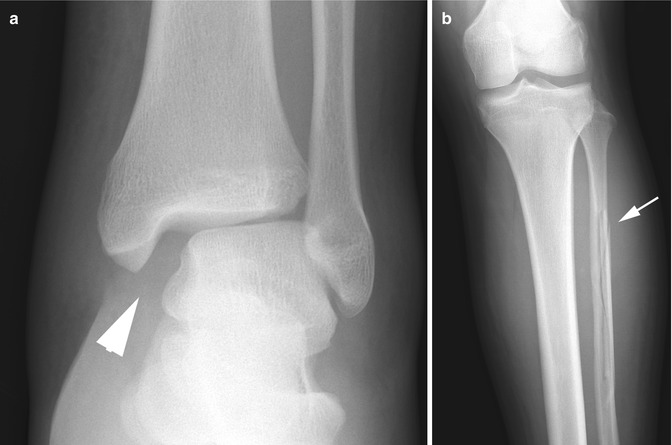
Fig. 16.7
Maisonneuve fracture in a 14-year-old boy. (a) Ankle radiograph shows medial tibiotalar joint space widening (arrowhead) consistent with a deltoid ligament injury. (b) Leg radiograph in the same patient demonstrates an oblique longitudinal fracture of the proximal fibular diaphysis (arrow)
Box 16.2: Maisonneuve Fracture
Mechanism: pronation/external rotation |
Associated with medial malleolar fracture or deltoid ligament injury |
Injury to syndesmosis and interosseous tibiofibular ligament |
Proximal fibular fracture or proximal tibiofibular dislocation |
Key: if there is medial malleolar fracture/deltoid ligament injury, evaluate the proximal fibula |
1.2 Midfoot and Hindfoot Fractures
The toddler spectrum of fractures may affect the bones of the midfoot and hindfoot, especially the cuboid (Fig. 16.8) [12]. The most likely mechanism is forced plantar flexion of the foot resulting in compression force at the cuboid.


Fig. 16.8
Toddler’s fracture of the cuboid in a 3-year-old boy. There is a transverse band of sclerosis at the proximal cuboid (arrow)
Fractures of the talus most often affect the neck [13] (Box 16.3). The usual mechanism is forced dorsiflexion of the foot, resulting in abutment of the anterior lip of the tibial plafond and the talar neck. Since most of the arteries to the talus (which include branches from the posterior tibial, dorsalis pedis, and peroneal) enter the talus at the level of the neck, there is a relatively high incidence of osteonecrosis after this type of fracture. The likelihood of post-traumatic osteonecrosis increases with the degree of talar neck displacement and increasing patient age [14, 15].
Box 16.3: Talar Fracture
Mechanism: forced dorsiflexion of the foot |
Usually affects the neck |
High incidence of osteonecrosis (tenuous blood supply) |
More likely with greater talar neck displacement and increasing patient age |
Follow for 18 months |
Calcaneal fractures usually result from falls from a height or direct injury (such as from a lawn mower) [13, 16]. Fractures that result from falls are usually less severe in skeletally immature patients because cartilage is plastic compared with adult bone. Stress fractures are fairly common in the calcaneus [17].
The navicular bone is affected by stress fractures [18] as well as avulsion injuries. Avulsion injuries generally occur at the insertion of the tibialis posterior tendon along the medial pole of the navicular. This is also the location of accessory ossicles, which are relatively mobile, leading to avulsion and/or symptomatic stress reaction. Accessory navicular ossicles are categorized according to the position of the ossicle with respect to the tendon. The type 1 ossicle is embedded in the tibialis posterior tendon, whereas the tendon fibers insert on the type 2 ossicle, which has a synchondrosis with the navicular [18].
Displaced talar neck fractures should be reduced to anatomic alignment. Nondisplaced fractures should be followed for at least 18 months to monitor for talar dome osteonecrosis [13]. Calcaneal fractures in children carry a better prognosis compared with adults and are likely to remodel without operative fixation. Symptomatic accessory navicular ossicles may be resected if conservative management fails to alleviate symptoms [19].
Imaging
Frontal, lateral, and oblique radiographs should be performed, preferably with weight bearing. The stress placed on the bones with weight bearing may help reveal subtle nondisplaced fractures, assess for longitudinal alignment of the foot, and—if there is a calcaneal fracture—provide a more accurate estimate of Bohler angle. Ankle radiographs should include the base of the metatarsals to assess the tarsometatarsal joints.
Calcaneal fractures are more likely to be extra-articular in children than in adults [18]. A Harris-Beath view may help evaluate fracture displacement in the mediolateral direction as well as intra-articular extension to the middle and posterior facets of the subtalar joint (Fig. 16.9). CT complements radiography and facilitates preoperative planning by quantifying the extent of displacement and intra-articular extension.
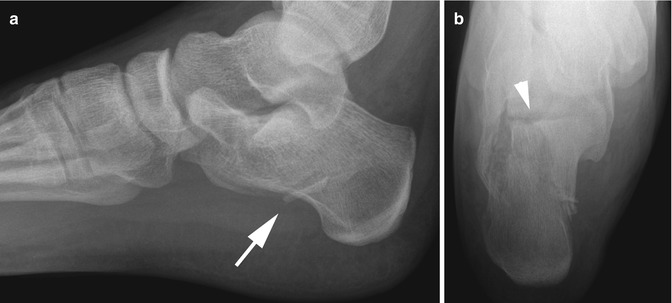
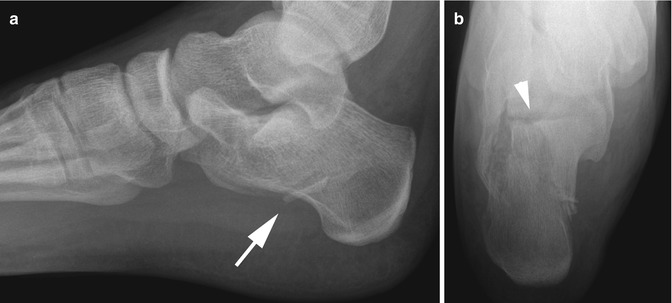
Fig. 16.9
Intra-articular calcaneal body fracture in a 15-year-old boy. (a) Lateral view shows a nondisplaced calcaneal body fracture (arrow). (b) Subtalar involvement is often apparent on the Harris-Beath view (arrowhead)
Follow-up of talar neck fractures should include evaluation for talar dome osteonecrosis, which appears as subchondral sclerosis, collapse, and fragmentation. Hawkins sign, which is first seen from 6 to 8 weeks after injury, indicates that there is adequate blood supply to the talar dome and low probability of osteonecrosis [20]. This sign appears as subchondral lucency that parallels the talar dome, and it results from imbalanced bone resorption relative to bone formation in the setting of hyperemia [21]. Determining the presence of Hawkins sign is probably less important in the era of MRI (magnetic resonance imaging).
MRI is helpful when radiographic findings are normal and an occult fracture or stress reaction is suspected (Fig. 16.10). MRI is also helpful in the evaluation of a symptomatic accessory navicular to assess for associated marrow edema and juxtacortical soft tissue edema (Fig. 16.11) [22].
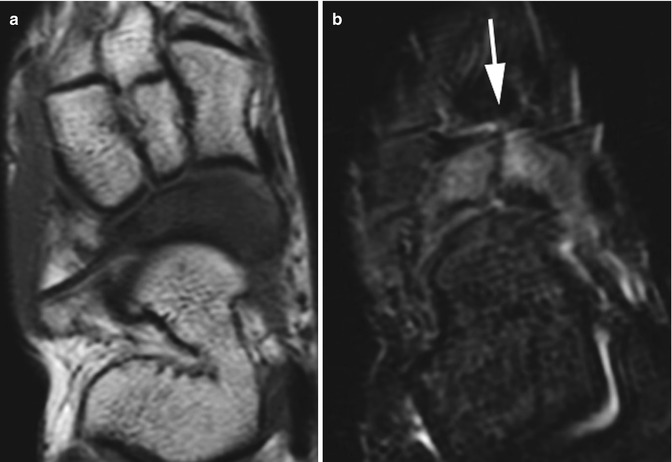
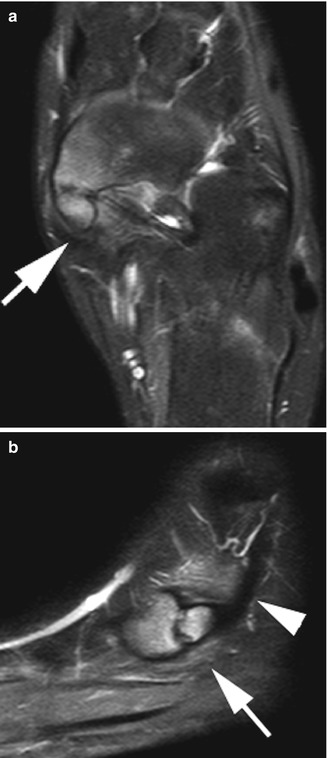
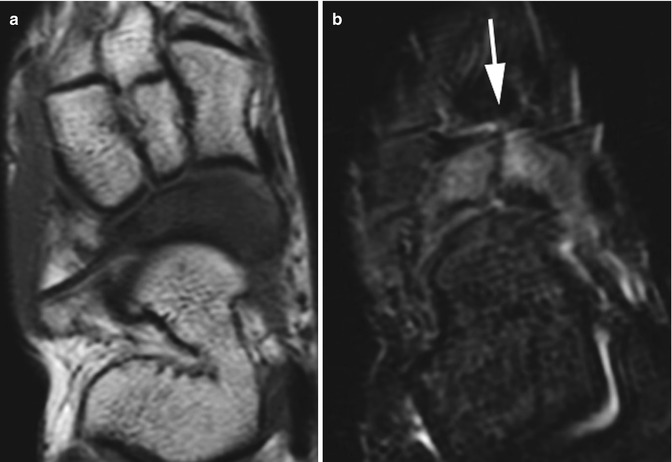
Fig. 16.10
Nondisplaced navicular stress fracture in a 14-year-old boy. (a) Axial T1-weighted (T1-W) image shows diffuse decreased signal throughout the navicular. (b) Axial short tau inversion recovery (STIR) image shows diffuse navicular marrow edema and a nondisplaced longitudinal fracture (arrow)
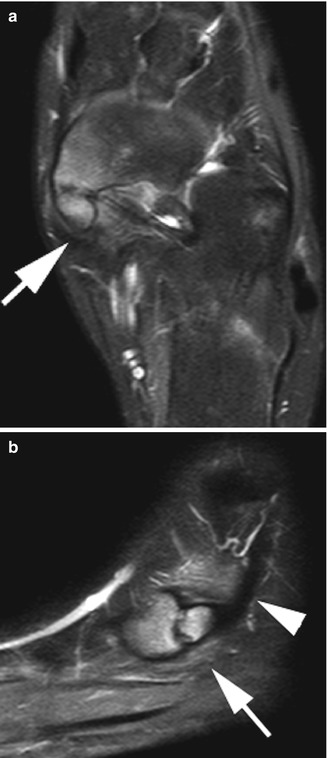
Fig. 16.11
Symptomatic type 2 accessory navicular in an 11-year-old girl. Axial T2-weighted (T2-W) fat-suppressed (FS) (a) and sagittal proton density (PD) FS (b) views show marrow edema at the navicular and accessory navicular as well as juxtacortical soft tissues (arrows). Tibialis posterior tendon (arrowhead)
1.3 Metatarsal Fractures (Box 16.4)
Box 16.4: Metatarsal Fractures
First metatarsal |
Pediatric bunk bed fracture, common in young children |
Flexion force wedges oblique first cuneiform-first MT epiphysis into first MT-second MR interspace |
Salter-Harris type II or buckle fracture at metatarsal base |
Pathogenesis similar to adult-type Lisfranc injury to ligaments |
Fifth metatarsal |
Fifth metatarsal tuberosity avulsion fracture: tubercle at the peroneus brevis tendon insertion |
Most common metatarsal fracture in children >5 years old |
Mechanism: ankle rotation with fixed forefoot |
Proximal fifth metatarsal diaphyseal fracture |
Overuse stress injury in adolescent athletes |
In vascular watershed, so heals poorly without screw fixation |
Jones fracture is more proximal |
Toddler-type fractures can affect the metatarsals due to either impaction or twisting forces [12]. Stress fractures of the foot are especially common in athletes and dancers, most often affecting the metatarsals [23]. The pediatric bunk bed fracture is thought to be the pediatric equivalent of an adult Lisfranc fracture-dislocation injury [24]. This injury occurs when a child jumps or falls from a height, landing with the foot plantar flexed. The vertical impaction force is transmitted to the proximal first metatarsal, possibly causing ligamentous injury along with fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree