Fig. 15.1
Fibular ossicle in a 15-year-old boy. Apparent irregularity (arrow) along lateral fibular metaphysis on frontal view (a) has well-corticated margins (arrowheads) on oblique view (b). There is no soft tissue swelling
The distal tibial physis is also often irregular. A focal superiorly oriented notch at the medial aspect of the distal tibial physis is normal (Kump bump) (see Chap. 16).
Additional ossification centers are often encountered at the distal ends of the medial and lateral malleoli in children and are especially common medially. Many differentiate between these centers, labeling them either secondary or accessory centers of ossification. Accessory centers may be single or multiple and are visualized adjacent to or slightly separated from the main epiphyseal center (Fig. 15.2). They will not fuse with the adjacent bone and thus persist into adulthood. Examples at the ankle include the os subtibiale and os subfibulare. In contrast, secondary ossification centers will usually coalesce with other epiphyseal or apophyseal centers, eventually contributing to adult bone contours (Fig. 15.3). At the ankle, these are usually seen inferior to the tip of the medial malleolus. These secondary centers are encountered in 17–24 % of boys and in up to 47 % of girls. They are bilateral in more than two thirds of patients and more frequently so in girls. Generally appearing between ages 7 and 8, they usually unite with the main epiphysis 1–1.5 years after initial ossification [3]. By age 12, most will have fused with the main ossific epiphysis, but 1–2 % remain separate through adulthood—especially at the fibula [4]; these eventually become persistent ossification centers.

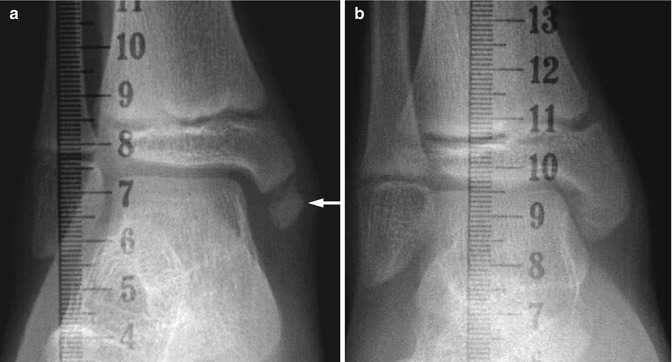

Fig. 15.2
Normal irregularity of the lateral malleolus in an asymptomatic 5-year-old girl. Oblique view shows small accessory ossification center adjacent to the distal fibula (arrow), without adjacent soft tissue swelling. This should not be mistaken for an avulsion injury
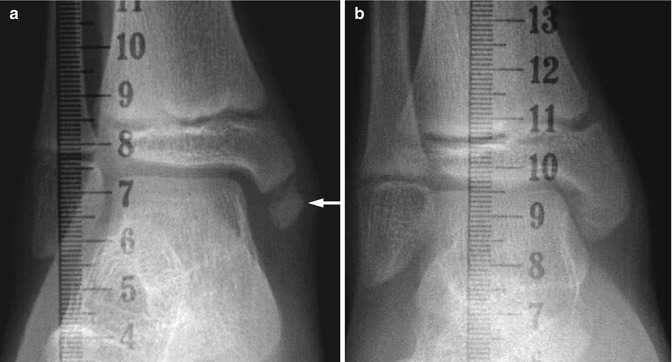
Fig. 15.3
Normal variant medial malleolar accessory ossification centers in a 12-year-old boy. (a) Frontal view shows a smoothly corticated osseous fragment (arrow) at the medial malleolus, consistent with an accessory ossification center. (b) Seven months later, the accessory ossification center has fused to the distal tibia. Both images were obtained as part of leg length studies
Old avulsion injuries, which appear as well-corticated, round ossific fragments in a similar location, are sometimes impossible to distinguish radiographically from an accessory or secondary ossification center. Indeed, some believe that these well-corticated fragments almost exclusively result from remote, unrecognized trauma [5]. Old injuries can usually be differentiated from acute fractures, in that acute fractures appear as curvilinear, irregular densities that lack corticated margins. It is possible, however, to injure the cartilaginous bridge between the accessory and main ossification centers. Clinically, there may be localized tenderness and swelling, but radiographs may not show an injury. This radiologically occult trauma will be evident on magnetic resonance imaging (MRI) as edema on T2-weighted (T2-W) sequences.
The tip of the lower fibular epiphysis is normally slightly inferior to that of the medial tibial epiphysis, with the physis of the fibula at the level of the ankle joint or slightly below it after age 4 years. The fibular growth plate should therefore be significantly more distal than the tibial growth plate. In infancy, the distal tibial and fibular growth plates initially provide most of the growth of the lower leg, but after 30 % of total bone length has been achieved, the proximal physes contribute the most longitudinal growth.
1.2 Imaging Examination and Analysis
The standard ankle series consists of anteroposterior (AP), lateral, and mortise views. Osseous detail is best evaluated on images obtained in the recumbent position. However, evaluation of ankle or hindfoot alignment requires weight-bearing views. These may be obtained with the child standing on radiolucent blocks or wood to accommodate the position of standard radiography equipment.
In order to obtain the best projection of the ankle mortise, the patient must be positioned supine with the foot in 15–20° of internal rotation. This oblique position compensates for normal external tibial rotation. For the lateral radiograph, the ankle should be parallel to the detector, with the fibula slightly posterior to the midline axis of the tibia. The standard oblique view requires medially rotating the ankle by 45°. Multiple other views have also been described but are less frequently utilized.
Radiography performed with stress applied to the ankle may be useful when chronic ligamentous injury or intrinsic malalignment is suspected. When there is an acute injury, stress views in children are quite painful and may require sedation. When stress is applied to the heel during eversion (whether by gravity or force), there should be no tilt of the talar dome in relation to the tibial plafond. With inversion the average obtainable tilt of the talar surface is 7°, with a normal range of up to 27°. With such marked change on inversion stress possible in normals, caution must be observed when using this to test for abnormal ligamentous laxity. Comparison views of both ankles can be obtained to look for asymmetry. Studies have shown that a 10° difference in inversion stress angulation between the two ankles is a specific but insensitive indicator of ligamentous injury [6]. Many consider stress radiography of the ankle unreliable and instead utilize clinical examination and dynamic imaging by ultrasound to directly evaluate the ligamentous structures.
In young children, there is normally a slight valgus angle of the distal tibial articular surface compared with the long axis of the tibia. This angle approaches 90° by age 10, when the articular surface becomes horizontal. This measurement may be altered in cases of marked developmental lower extremity bowing.
Slanting of the articular surface of the distal tibia with lateral side superior is termed “ankle valgus.” This has been reported as a feature of paralysis, sickle cell anemia, juvenile idiopathic arthritis, multiple epiphyseal dysplasia, hemophilia, and many other entities. However, the appearance of distal tibial angulation may also result from improper positioning of the foot during imaging. A well-positioned, weight-bearing AP of the ankle is necessary to measure ankle valgus. If the knee is both flexed and externally rotated more than 20°, images may give a false impression of tibiotalar obliquity. Ankle varus usually follows trauma. “Calcaneus” and “equinus” deformities at the ankle are discussed below in the sections on radiographic analysis and deformities of the foot, since these dorsi- and plantar-flexion deformities are important in the evaluation of foot alignment.
MRI is useful for directly evaluating the soft tissue structures of the ankle, including ligaments and tendons. It also provides detailed anatomic information about cartilaginous, nonossified structures that can only be inferred from radiographs. Cartilage and soft tissues may also be evaluated by US.
1.3 Congenital Abnormalities
Congenital anomalies exclusively involving the ankle are uncommon. Aberrations of normal ankle relationships may accompany fibular or tibial longitudinal deficiency, as well as midfoot and hindfoot abnormalities such as congenital tarsal fusion. Congenital diastasis of the inferior tibiofibular joint is a very rare, severe deformity that may initially clinically resemble clubfoot [7] (Fig. 15.4). This entity has been considered part of a spectrum of distal tibial dysplasia with an intact fibula [8]. Diastasis of the distal tibia and fibula results in superior migration of the talus with resulting posteromedial displacement of the medial malleolus and dislocation of the distal fibula. Other congenital anomalies may be associated, including clubfoot and congenital heart disease. Treatment aims to preserve the foot, stabilize the ankle, and correct leg length discrepancies.
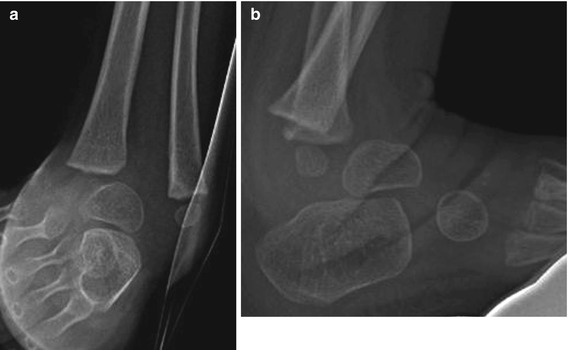
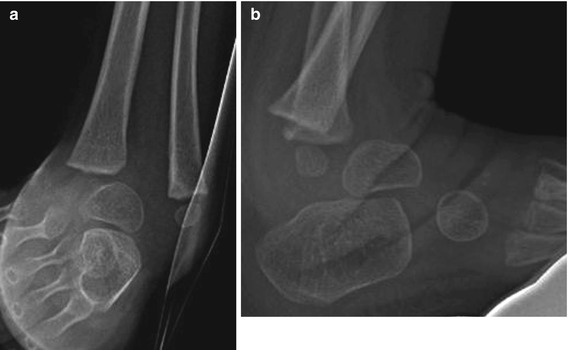
Fig. 15.4
Congenital diastasis of the inferior tibiofibular joint in a 2-year-old boy. Frontal (a) and simulated weight-bearing lateral views (b) show widening of the space between the distal tibia and fibula with superior migration of the talus, posteromedial displacement of the tibia, and dislocation of the distal fibula. This patient also had clubfoot, a commonly associated abnormality
The ball-and-socket ankle is characterized by a hemispheric configuration of the articular surface of the talus on both frontal and lateral radiographs, with corresponding congruent concavity of the distal tibial articular surface (Fig. 15.5). Congenital and acquired etiologies of ball-and-socket ankle have been suggested (Table 15.1). Two major hypotheses have been proposed to explain the mechanical development: one postulates a secondary adaptation in shape to permit inversion and eversion in an ankle that has been limited by congenital tarsal fusions; the other states that the ball-and-socket ankle may be a characteristic component of a complex malformation with both deleted and fused foot bones. Regardless of etiology, this entity may not become symptomatic during childhood. However, its association with leg length discrepancy and other congenital abnormalities makes it important to recognize [9]. More recent studies have suggested that a surgical corrective approach to limb length discrepancies and malalignment in the setting of ball-and-socket ankle may prevent chronic osteoarthrosis and pain [10].


Fig. 15.5
Ball-and-socket ankle along with talonavicular coalition in a 12-year-old boy. (a) Frontal view shows hemispheric configuration of the talar dome, with concave distal tibial articular surface. (b) Axial-reformatted computed tomographic (CT) image from the same patient shows complete talonavicular osseous fusion and ray deletion. T talus, N navicular
Table 15.1
Associations and etiologies of ball-and-socket ankle
Congenital | Acquired |
|---|---|
Short extremity | Tarsal coalitions |
Tarsal coalition | Subtalar surgical arthrodesis at very young age |
Absent or fused rays | Polio (after surgical arthrodesis at young age) |
Hypoplastic fibula | Myelomeningocele |
Skewfoot or clubfoot | Hyperlaxity |
Acrocephalosyndactyly | Congenital insensitivity to pain |
Congenital ball-and-socket ankle has been observed as early as 6 weeks of gestational age. During development, the abnormal talus ossifies more slowly than the normal side, and an abnormal shape of the talus may be detected on radiographs before 1 year of age [11]. Ball-and-socket ankle is associated with varying degrees of limb shortening. Anomalies of the forefoot rays are usually seen in conjunction with ball-and-socket ankle joint. Sixty percent of patients have some form of tarsal coalition, most commonly talonavicular or calcaneocuboid (see Fig. 15.5); occasionally all the hindfoot and midfoot structures are fused. By age 5 or 6, the ankle articulation has usually become a nearly perfectly congruent hemisphere.
Rounding of the talar dome may also be seen in older children without congenital fusions. For example, it may occur in patients with epiphyseal dysplasias or in the setting of ankle instability associated with chronic hyperlaxity from a young age, as seen in Larsen syndrome or myelomeningocele [12]. In these cases the talar trochlea is less rectangular than normal but usually does not have the near perfect rounding of congenital ball-and-socket ankle.
1.4 Developmental Abnormalities
In some situations, the plane of the ankle joint tilts into valgus. This may occur with paralytic conditions, such as myelomeningocele when growth of the distal fibula may be selectively impaired. Instead of the distal fibular physis sitting at the level of the ankle joint, undergrowth causes the distal fibular physis to be positioned above the level of the ankle joint (Fig. 15.6). Since ligaments tether the lateral edge of the distal tibial epiphysis to the fibula, poor development of the lateral malleolus may cause decreased growth and subsequent wedging of the lateral portion of the distal tibial epiphysis. Defective architecture of the ankle mortise may then lead to lateral instability of the ankle, with valgus tilt of the articular surface. Ankle valgus may occur in conjunction with genu valgum (Fig. 15.7), and in this setting the ossification of the fibular epiphysis may be delayed.



Fig. 15.6
Impaired growth of the fibula in a 9-year-old girl with myelomeningocele. Frontal view shows the fibula is relatively short compared with the tibia, since the distal fibular physis should be at or just below the level of the tibiotalar joint after age 4 years

Fig. 15.7
Bilateral ankle valgus in a 7-year-old with genu valgum (Courtesy of Rebecca Stein-Wexler; Copyright Shriners Hospital for Children Northern California)
If the fibula is not intact, lack of weight-bearing forces on the fibula may cause growth inhibition and subsequent ankle valgus. This may occur in the setting of fibular resection or with fibular pseudarthrosis. Valgus ankle deformity also commonly occurs in the setting of multiple hereditary exostosis [13]. Relative fibular overgrowth with distal tibial or ankle varus may be seen in bone dysplasias such as achondroplasia, hypochondroplasia, and dyschondrosteosis [14, 15] and also after some fractures.
2 The Foot
2.1 Normal Anatomy and Variations
Anatomy and Development
The foot is a complex anatomical structure that performs a variety of biomechanical functions. These include weight bearing, shock absorption and propulsion during walking and running, and accommodating a variety of uneven surfaces. The foot is conventionally divided into three units: hindfoot, midfoot, and forefoot. These categories are useful to understand foot function, biomechanics, and pathophysiology. The hindfoot is composed of the talus and calcaneus, and the forefoot is composed of the metatarsals and phalanges. The midfoot includes the intervening tarsal bones: the cuneiforms, the navicular, and the cuboid. Although the last two are considered by some to be part of the hindfoot, from the viewpoint of radiologic analysis they are best considered midfoot structures. A variety of complex motions and deformities occur in all three regions, discussed below in the section on analysis of normal alignment.
The development of the cartilaginous structures that form the bones of the foot begins during approximately the 7th–9th week of gestation. Ossification typically follows a normal, sequential pattern within the foot, although congenital, infectious, and pregnancy-related abnormalities may alter the timeline. Ossification starts in the forefoot, beginning with the ends of metatarsals, with subsequent ossification of the metatarsals and then—sequentially—the proximal, middle, and distal phalanges. At birth all the metatarsals and phalanges are partially ossified. The tarsal bones ossify later, beginning at 24–28 weeks of gestation; only the talus and calcaneus are consistently partially ossified at birth. The sustentaculum tali do not begin to ossify until age 1–2 years and is not fully developed until age 5. The navicular is the last to ossify, usually between age 2 and 4 years [16] (Fig. 15.8).


Fig. 15.8
Foot development. (a, b) At 1-year-old, the talus, calcaneus, cuboid, and lateral cuneiform have ossified. (c, d) At 5-year-old, all tarsal bones have ossified but their contours have not developed. (e, f) At 9-year-old, the foot has an adult configuration
Tarsal bone position is very important in evaluating foot deformities. However, limited tarsal ossification in the newborn and young child requires inference of their positions at radiography. Occasionally, US or MRI may be used to assess the developing tarsal bones before they ossify.
The foot grows rapidly from infancy to 5 years of age. It reaches one-half its adult size by age 5; growth slows and then usually ceases about age 12 years in girls and 14 years in boys, at which point the foot is considered mature. The anatomic relationship of the tarsal bones also changes during development. For example, the angle formed by the longitudinal axes of the talus and calcaneus gradually decreases with growth as the talus becomes less vertical, as indicated by a decrease in the lateral talocalcaneal angle from 45° on average in the newborn to 33° at age 4 years [17]. Similarly, the dorsiflexion-plantar flexion range of the foot decreases with age (76° at birth, 60° at age 1 year).
Normal Variants
Multipartite and Accessory Tarsal Centers
Ossification variants and accessory centers are common in the foot. Recognition of their characteristic appearance and location is important to avoid misdiagnosing a fracture or other injury. While some variants are common and readily recognized, others such as the striking vertical cleft of a bipartite talus are rare. A complete listing of the common accessory centers is provided in standard texts, but the most significant are discussed below.
It is unlikely that the presence of an ossification variant will lead to symptoms or later disability, since in most cases the multipartite or aberrantly ossifying nucleus is contained in a single normal cartilaginous anlage, with the centers fusing by maturity (Fig. 15.9).


Fig. 15.9
Bipartite navicular in a 4-year-old girl. There are two separate ossification centers (arrow and arrowhead) for the navicular
The accessory navicular (os naviculare) is a common developmental variant that may be symptomatic, causing pain and peroneal spasm. This ossicle has been reported in 4–21 % of the population; 50–90 % are bilateral [18]. It ossifies around age 7–11 years [19] and is usually discovered incidentally when a child gets radiographs for foot pain or injury.
Three subtypes are generally recognized. The Type I accessory navicular accounts for about 30 % of cases. It appears as a 2–6 mm round or oval ossicle that represents a sesamoid bone within the posterior tibial tendon (Fig. 15.10). This ossicle is completely separate and is positioned about 2–5 mm proximal to the navicular body [20]. A Type 1 ossicle is also known as an os tibiale externum or navicular secundarium.


Fig. 15.10
Type 1 accessory navicular in an 11-year-old girl. There is a rounded ossicle (arrow) proximal to the navicular body
The Type 2 accessory navicular ossicle is also known as a prehallux or bifurcated hallux. It is more common than Type I, accounting for up to 70 % of accessory navicula. It is usually larger and has a flattened anterior surface that forms a facet with the medial proximal navicular tubercle, resulting in a triangular or heart-shaped ossicle (Fig. 15.11). The 1–2 mm interval separating this ossicle from the navicular represents a cartilaginous or fibrocartilaginous connection. Injury to this area may cause fracture and secondary pseudarthrosis of the synchondrosis or painful tendonosis or synovitis in some older children [21]. Fracture or pseudarthrosis of Type 2 accessory navicular ossicles is difficult to diagnose on radiographs. When symptomatic, an MRI is useful to evaluate for reactive bone marrow edema as well as secondary soft tissue findings, replacing technetium-99m bone scan [18] (see Chap. 16).


Fig. 15.11
Type 2 accessory navicular in a 12-year-old girl. There is characteristic flattening of the anterior surface (arrow), creating a facet with the medial proximal navicular tubercle (arrowhead)
A Type 3 accessory navicular or cornuate navicular has been described as an especially prominent contiguous medial margin of the navicular, which may result from osseous bridging of a previously separate center. This causes a prominent, often symptomatic, protuberance (Fig. 15.12).


Fig. 15.12
Type 3 accessory navicular in a 16-year-old boy. The prominence of the medial margin of the navicular bone may be secondary to osseous bridging of previously separate ossification centers
Bipartite or multiple ossification centers have also been reported at the cuboid and cuneiform bones, but these are generally asymptomatic. Double ossification centers within the calcaneus create a well-defined linear lucency through the central portion of this bone (Fig. 15.13), often associated with underlying conditions, such as trisomy 21 or Larsen syndrome. The formation of multiple ossification centers within a bone may also occasionally result in the appearance of an irregular-appearing central ossification site (Fig. 15.14). When this occurs in the navicular bone, it may be difficult if not impossible to distinguish the normal variant from Kohler osteonecrosis. This painful condition resembles variant ossification of the navicular, but flattening and sclerosis are more pronounced in Kohler osteochondrosis (see Chap. 16).



Fig. 15.13
Double ossification center of the calcaneus in a normal 17-month-old boy

Fig. 15.14
Incidental irregular-appearing navicular in a 5-year-old boy, likely a normal variant given lack of focal symptoms. Frontal (a) and oblique (b) views show the margins of the navicular are sclerotic and irregular (arrows). Osteonecrosis may appear similar or the bone may appear flatter and more sclerotic; the patient will be symptomatic
A few of the many other accessory ossicles merit discussion. A normal accessory ossification center arises from the talus at the posterior ankle during normal development, ossifying around age 5 years and typically fusing with the talar body by age 20. Failure of fusion results in an ossicle called an os trigonum (Fig. 15.15). Posterior ankle impingement during plantar flexion may develop in dancers and other athletes. Chronic reactive changes from overuse or stress fracture may cause pain. MRI identifies edema, suggesting os trigonum syndrome [22] (see Chap. 16).


Fig. 15.15
Os trigonum and os supranaviculare in a 12-year-old girl. Well-corticated ossified fragment posterior to the talus is consistent with an os trigonum (arrow). Additional smooth fragment along the dorsal aspect of the talonavicular articulation is consistent with an os supranaviculare (arrowhead)
An os supratalare is a small, round ossicle along the dorsal aspect of the anterior talus on a lateral view; this may simulate a fracture (Fig. 15.16). An os supranaviculare is an irregular ossicle that typically fuses by about age 5 years; this too may look like a fracture or an accessory or bipartite navicular bone (see Fig. 15.15). Pain has been attributed to most ossicles, but aside from those highlighted above most are asymptomatic [23].


Fig. 15.16
Os supratalare in a 17-year-old boy. Small, oval ossific fragment (arrow) at the level of the talar neck is consistent with this accessory ossicle, particularly in the absence of focal symptoms or localized soft tissue swelling
Calcaneal Apophysis
In the infant and young child, the posterior cortical margin of the calcaneus is smooth. An irregular, sawtooth outline often develops before the ossification centers for the apophysis appear. The apophysis ossifies from several discrete centers, which then coalesce into one apophyseal center. The first of these appears between 4 and 7 years of age in girls and between 7 and 10 in boys. They usually demonstrate an extremely irregular outline, frequently traversed by several discrete linear lucencies. The normal ossification center(s) are often exceptionally dense, appearing more sclerotic than the calcaneal body on a lateral radiograph (Fig. 15.17).


Fig. 15.17
Normal calcaneal apophysis in a 9-year-old boy. The apophysis is more sclerotic than the other bones, and it is traversed by several lucencies (arrowheads). An os trigonum (arrow) is also present
A strikingly sclerotic, irregular calcaneal apophysis is often encountered in 8–10 year old girls and 9–12 year old boys who complain of heel pain during this period of rapid growth in length of the calcaneal tubercle. Perhaps best termed “calcaneal apophysitis,” in the past this was considered diagnostic of “osteochondrosis” or Sever disease. The normal finding of increased density of the calcaneal apophysis may in part be a response to weight bearing. With bed rest (which is not recommended for this condition), the apophysis becomes osteopenic, eventually reaching the same density as the calcaneus. After 1 month of weight bearing, density is restored [24]. Eventually, as the apophysis fuses at age 12–15, the posterior margin of the calcaneus becomes isodense to the rest of the bone.
Fifth Metatarsal Base Apophysis
This secondary ossification center parallels the lateral cortex of the fifth metatarsal. Multiple sliver-like centers may be present (Fig. 15.18). Fractures of the proximal fifth metatarsal, in contrast, are usually transverse to the metatarsal base, although oblique fractures may occur (see Chap. 16). The diagnosis of apophyseal separation should be made with caution, since the normal ossific portion of the apophysis may be quite lateral in the cartilaginous mass (Fig. 15.19). When in doubt, follow-up radiographs or images of the contralateral side may be helpful, as they may demonstrate evidence of healing or asymmetry. MRI may be performed but is usually not necessary.



Fig. 15.18
Normal base of fifth metatarsal apophysis in a 12-year-old girl. Oblique view shows the normal apophysis paralleling the lateral cortex of the fifth metatarsal (arrow). Multiple ossification centers (arrowheads) may be present

Fig. 15.19
Normal base of fifth metatarsal apophysis in a 10-year-old boy. Oblique view shows normal apparent separation of the ossific center from the adjacent metatarsal due to interposed cartilage (arrow). This should not be misinterpreted as an avulsion fracture
Metatarsals and Phalanges
The fifth toe has only two phalanges in almost half the population, due to fusion of the distal interphalangeal joint. The epiphysis of the proximal phalanx of the first toe may have a central split (bifid epiphysis), due to incomplete ossification (Fig. 15.20). The bifid epiphysis may also appear sclerotic. Occasionally, the proximal epiphyses of other toes may be affected. Pseudoepiphyses may be seen at the base of the metatarsals and at the distal aspects of the phalanges (Figs. 15.21 and 15.22). The epiphyses of the proximal phalanges are frequently cone-shaped, perhaps due to premature closure of the central physis (see Fig. 15.22). Although often a normal variant, coned epiphyses are also found in a variety of syndromes.




Fig. 15.20
Bifid epiphysis of the first toe in a 13-year-old boy. The epiphysis at the base of the proximal phalanx of the great toe is split and relatively sclerotic (arrowheads)

Fig. 15.21
Pseudoepiphysis of the first toe in a 10-year-old boy. There is an incomplete, transverse well-corticated lucency (arrow) at the distal aspect of the proximal phalanx

Fig. 15.22
Coned epiphysis in a 12-year-old girl. The epiphysis at the proximal phalanx of the fourth toe has a cone-like shape (arrow). There are also multiple pseudoepiphyses (arrowheads)
A longitudinal epiphyseal bracket is rare, occurring in 2–14 % of congenital deformities of the hand and foot. Eleven percent of these cases involve the first toe [25]. In this entity, the normally transverse epiphysis is C-shaped and oriented along the longitudinal edge of the bone, causing abnormal transverse growth and shortening of the phalanx, as well as angular deformity (Fig. 15.23). This can be identified by radiographs or MRI and requires operative resection [26].


Fig. 15.23
Bracket epiphysis in a 10-year-old girl. Abnormal and fused proximal and distal epiphyses at the first toe proximal phalanx create a C-shape (arrow), widening, shortening, and tethering the phalanx. Note bifid appearance of the tuft of the great toe (arrowhead)
2.2 Imaging Examination and Analysis
Radiographs
The basic radiographic examination in the evaluation of foot deformities comprises a weight-bearing AP and a weight-bearing lateral projection of the foot. Weight bearing stresses the foot in a reproducible manner and shows the relationship of the bones in their functional state (Fig. 15.24). In an infant or non-ambulating older child, simulated weight-bearing radiographs may be acquired by using a wooden or plastic board to apply plantar pressure or an attendant may apply direct manipulation. Although every effort should be made to avoid radiation exposure of persons other than the patient, it is often impossible to achieve the correct plantar pressure and lateral positioning of the young infant’s foot by any means other than a well-shielded assistant. Proper technique is essential.
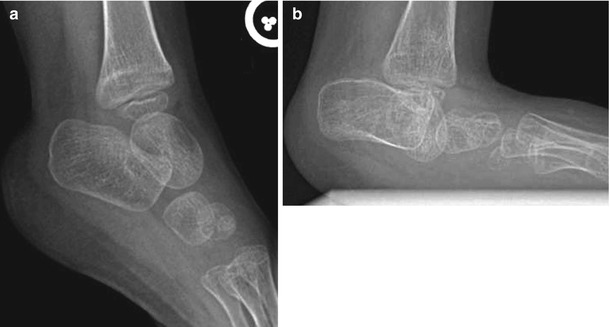
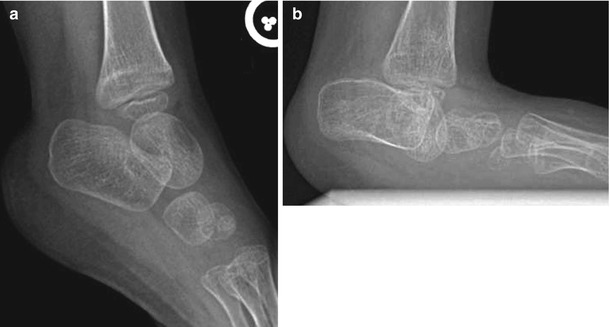
Fig. 15.24
The effect of weight bearing on hindfoot alignment. (a) Non-weight-bearing view shows markedly abnormal configuration of the hindfoot, including vertical talus in this 5-year-old with fibular longitudinal deficiency. (b) With simulated weight bearing, the configuration of the talus is even more abnormal, as it projects between the calcaneus and the cuboid. Rocker-bottom configuration becomes apparent, as well
An AP projection is obtained with the child standing, with tibias parallel to a sagittal plane perpendicular to the plane of imaging. Patients unable to stand may sit or lie supine with knees flexed and the feet plantigrade, pressed against the image receiver; the tibias should be aligned as for a standing radiograph. The central x-ray beam is angled about 15° toward the heel to eliminate overlap of the lower leg and posterior foot. Opinions vary about whether to attempt to correct alignment during imaging, as some surgeons prefer to have evidence of flexibility and the ability to correct deformity, while others prefer to view the uncorrected relationships.
A lateral projection is taken with the patient standing and leaning forward to show the foot in dorsiflexion (see Fig. 15.24). Similar positioning may be obtained in infants and non-ambulatory patients with directed plantar pressure with a radiolucent board. Care must be taken to ensure that the board used to produce plantar pressure is not tilted to produce a false impression of varus or valgus. To avoid projectional distortion of the talar dome in a medially deviated foot, the ankle and hindfoot (not the forefoot) should be placed in a true lateral position.
Oblique projections of the foot are often useful in evaluation of trauma, surgical follow-up, or tarsal coalition. However, they are not necessary in the initial or serial evaluation of the structurally deformed foot.
Dedicated radiographic techniques for imaging the subtalar joints are useful in some circumstances, although definitive diagnosis of hindfoot pathology generally requires CT or MRI. In addition to the standard AP, lateral, and oblique views of the foot, several other views may be helpful in specific cases. Lateral foot radiographs in maximum plantar flexion and maximum dorsiflexion may help in assessing rigidity of foot deformity as well as subtalar motion. The 45° axially angulated Harris-Beath projection of the heel is the most commonly performed supplemental examination to see sustentaculum tali fracture or subtalar coalition. However, due to the wide variability in the orientation of the subtalar joint, 30–60° beam angulation may be necessary if the articular facets are not shown well at first. When successful, this projection will show the posterior subtalar joint laterally as well as the medial facet located medially, superiorly, and parallel. This view is not useful in young children, since the sustentaculum tali do not fully ossify until age 5 years.
Nuclear Medicine Imaging
Bone scans utilizing technetium-99m have relatively limited use in detecting occult trauma, infection, or areas of avascular necrosis, since MRI can provide similar information while also offering more anatomic detail without radiation exposure.
Ultrasound
The advantages of US are the same when imaging any part of the body—imaging is performed rapidly and without sedation, dynamic images can be obtained, and the modality is typically readily available and relatively inexpensive. US also provides the highest resolution of soft tissue detail. However, while US readily depicts the cartilaginous portions of bones, the limited depth of beam penetration precludes complete assessment of the complex articulations between the bones of the hindfoot and midfoot.
Directed US can provide measurements or depict relationships between specific structures [27]. In the setting of clubfoot, for example, defining the relationship between the talus and navicular is essential, and this can be directly visualized by observing the distance between the medial malleolus and the navicular [28]. Dynamic imaging can show reducibility of the navicular medially with respect to the talus during manipulation [29]. It can also evaluate the reducibility of the talonavicular joint in vertical talus [30] (see subsequent sections on clubfoot, pes planus, and congenital vertical talus).
Computed Tomography
With the ongoing development of multi-slice computed tomography (CT) systems and the ability to reduce radiation dose through various new image reconstruction algorithms, CT imaging of the foot is useful in many clinical settings, including tarsal coalition, fracture evaluation, postoperative imaging, and tumor evaluation (especially osteoid osteoma). Images can be acquired rapidly, typically without sedation, while minimizing radiation exposure and maintaining image quality [31]. CT can be performed with or without simulated weight bearing using similar techniques and with similar clinical applications, as described above for radiography. Multiplanar image reconstructions are now standard. Three-dimensional (3D)-reconstructed images are easily generated on most systems and are particularly useful for surgical planning.
CT has replaced conventional radiographic tomography in the investigation of the subtalar joint, as it provides a more definitive evaluation of the osseous structures while evaluating the soft tissue and cartilaginous structures as well. When evaluating for tarsal coalition, CT reformatted in the axial and coronal planes is often most useful [32].
Magnetic Resonance Imaging
Because of the superior soft tissue contrast available with MRI, this modality is best for delineating the relationship of the partially ossified cartilage templates of the tarsal bones during childhood. While other modalities such as US can also demonstrate the cartilaginous and soft tissue structures of the immature foot, MRI provides a complete, global assessment. MRI is also useful when evaluating tarsal coalition, as it characterizes non-osseous bridging and evaluates for reactive changes in the bones and adjacent tendons [33]. For routine evaluation, standard radiographs usually provide sufficient information, and additional imaging is limited to addressing specific clinical questions. The utility of MRI remains limited by long acquisition times and need for sedation in most young children.
Arthrography
Interventional direct contrast material injection to delineate the cartilage and joint surfaces has been replaced by US and MRI, but arthrography remains the modality of choice to establish joint continuity. The posterior subtalar (facet) joint, talocalcaneonavicular (anterior and middle facets), and ankle joints are all accessible to contrast material administration. Injection into the posterior subtalar joint may be useful for therapeutic and diagnostic purposes if there is a need to establish communication with the ankle joint.
Arteriography
An abnormal size and distribution of the small arterial vessels of the foot has been described in congenital deformities. However, conventional angiography is rarely performed for operative planning. If knowledge of arterial vascular anatomy is needed, CT angiography or MRI angiography of the lower extremities provides a noninvasive means to obtain this information.
2.3 Analysis of Alignment (Figs. 15.25 and 15.26)
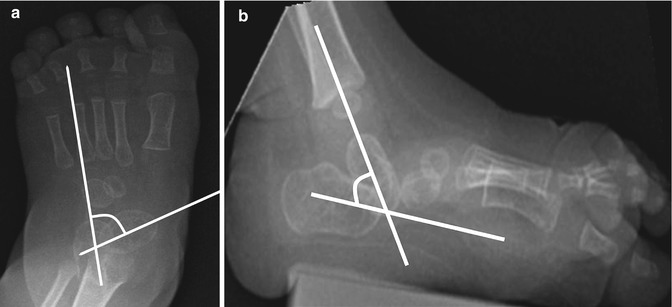
Fig. 15.25
Hindfoot relationships. In a normally aligned foot, the long axis of the calcaneus in an AP projection should pass through the base of the fourth metatarsal. A line drawn along the long axis of the talus should pass through or slightly medial to the base of the first metatarsal. In a normally aligned foot, a line drawn along the long axis of the talus on a lateral view should align with the long axis of the first metatarsal (the Meary angle). With hindfoot varus, the axis of the talus on the frontal view is laterally deviated from the midline. On a lateral view, the long axis of the talus is superior to that of the first metatarsal. The calcaneus and talus therefore appear more parallel on both views. With hindfoot valgus, the long axis of the talus is angled toward midline on the frontal view. On a lateral view, the long axis of the talus points inferior to the long axis of the first metatarsal. The calcaneus and talus therefore appear more divergent on both views
Fig. 15.26
Forefoot relationships: normal, adduction, and abduction. In the normal forefoot, the metatarsals are splayed, without significant overlap of the bases on an AP view. On a lateral view, the metatarsals converge distally. With forefoot adduction, the metatarsals are torqued so that the sole faces inward on an AP view. There is increased superimposition of the metatarsal bases, with the distal metatarsals swinging toward midline. On a lateral view, the metatarsals are generally configured in a ladder-like array due to concomitant inversion, with the fifth metatarsal being the most plantar. With forefoot abduction, the metatarsals are more parallel than normal on the frontal view, and there is less overlap at their bases, resulting in a broader forefoot. There may be a ladder-like array on a lateral view, with the first metatarsal most plantar (due to eversion), but this is rarely seen
The alignment of the ankle, hindfoot, midfoot, and forefoot is best evaluated separately, even though these structures are obviously intimately related both anatomically and functionally. The ankle, of course, consists of the distal tibia, distal fibula, and the talus. Two motions are possible: dorsiflexion and plantar flexion; the corresponding deformities consist of calcaneus and equinus. (Valgus and varus tilt are described above in the section on radiologic analysis of the ankle.)
In radiologic practice, the hindfoot unit comprises the talus and calcaneus; the midfoot consists of the navicular, cuboid, and cuneiforms; and the forefoot, the metatarsals and phalanges. At the hindfoot, varus and valgus deformities may occur. Midfoot deformities are described as cavus and planus. Forefoot deformities are adduction and (less common) abduction. Inversion and eversion are more complex, involving motion of most of the foot around an essentially stationary talus. Most of this motion occurs at the intertarsal joints.
Hindfoot
Hindfoot alignment is assessed by analyzing the relationship between the talus and calcaneus on standard AP and lateral foot radiographs. Axial lines are usually drawn along the central axis of these bones (Fig. 15.27). However, on AP views of very young children, it may be preferred to draw the central talar line parallel to the medial cortex of the ossification center and the central calcaneal line parallel to the lateral cortex of the calcaneus. Similarly, on a lateral projection it may be preferred to draw central lines (see Figs. 15.25 and 15.27), although some suggest using the undersurface of the calcaneus [34]. The calculation of actual angles is often advocated, and some studies have shown excellent interobserver agreement when assessing standard measurements [34]. The placement of lines, however, remains somewhat arbitrary, and this limitation should always be considered.
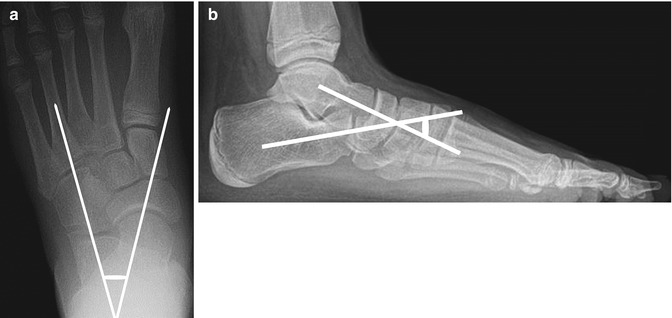
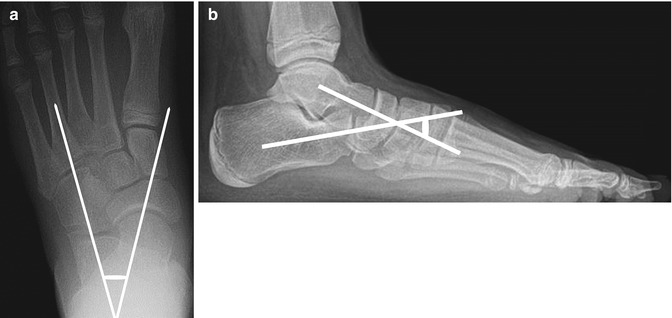
Fig. 15.27
Normal talocalcaneal relationships in a 13-year-old girl. Frontal (a) and lateral (b) views show lines drawn along the central axes of the talus and calcaneus. The intersection of these lines forms the talocalcaneal angle, which should be between 30 and 45° (weight-bearing views)
During dorsiflexion and plantar flexion, the talus moves with the foot. With varus and valgus motion of the hindfoot, the position of the talus is considered fixed with respect to the ankle, and the position of the calcaneus is described in relation to the talus. When observed from behind, the calcaneus is normally in 5–10° valgus compared to the talus in the coronal plane. This translates on AP radiographs to midtalar and midcalcaneal lines forming an angle averaging 42° (range, 27–56°) in the newborn, decreasing to an average of 34° by age 4 years. As a general rule, this angle should be 30–45°, decreasing with age.
The lateral talocalcaneal alignment in dorsiflexion is maximum from birth up to the age of 2 years, initially measuring 45° and then decreasing to a mean of about 33°. As a general guideline, this angle should also be 30–45°. A similar evolution is seen in the range of the dorsiflexion and plantarflexion gliding motion of the talus: the average range of 76° in a child less than 1 year old decreases gradually as the child grows.
The calcaneus is mechanically linked to the midfoot and forefoot bones, and it is therefore reasonable to consider the relation of the midtalar and midcalcaneal lines to the bases of the metatarsals. The midtalar line normally passes through or slightly medial to the base of the first metatarsal. The midcalcaneal line should pass through the base of the fourth metatarsal (see Figs. 15.25 and 15.27). When forefoot deformity is present, these lines do not necessarily pass down the shafts of the metatarsals.
The pitch of the calcaneus on a lateral view is measured with the tibiocalcaneal angle, which is the angle between the distal tibial shaft and the midcalcaneal line. This angle is about 77° at birth, decreasing to 67° by age 4 years. As a general rule, the tibiocalcaneal angle should be between 60 and 90°. The anterior calcaneus is therefore normally in slight dorsiflexion with respect to the tibia.
Midfoot
Ligaments link the midfoot bones to the calcaneus but not to the talus; therefore an abnormal position of the calcaneus relative to the talus should be made evident by a change in the relation of the midfoot bones to those of the hindfoot. Unfortunately, the navicular, which would be the key to this change, is the last to ossify. The navicular, when ossified, should be seen immediately distal to the middle portion of the talar head on both AP and lateral projections (Fig. 15.28); any shift in position indicates an abnormal relationship between the midfoot and the hindfoot. If the navicular is not yet ossified, assessment of alignment depends on the metatarsal bases, as discussed above. However, the lateral cuneiform, which begins to ossify between the newborn period and 19 months of age, may help indicate midfoot and hindfoot deformity.
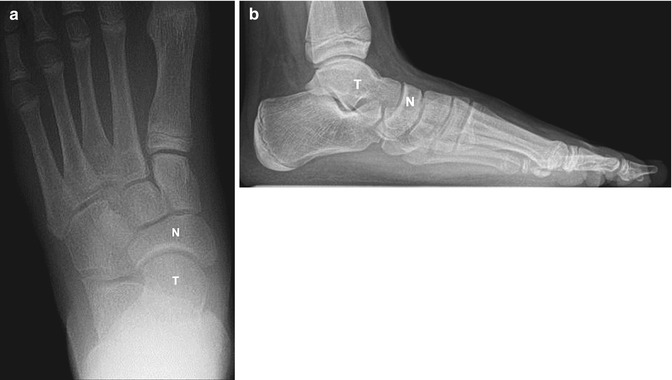
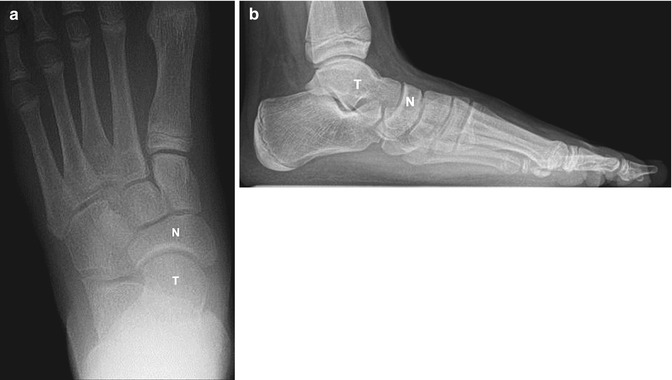
Fig. 15.28
Normal talonavicular relationship in a 13-year-old girl. The navicular is immediately distal to the middle of the talar head on frontal (a) and lateral (b) projections (weight-bearing views). T talus, N navicular
Forefoot
This portion of the foot comprises the metatarsals and phalanges, but only the metatarsals are generally useful in the analysis of forefoot alignment. The forefoot is usually flexible, and thus metatarsal alignment may be altered during imaging by variable/inconsistent degrees of weight bearing, poor patient cooperation, and active attempts to straighten the foot. Analysis of the apparent metatarsal shaft alignment is therefore not necessarily reliable. However, the metatarsal bases should have a constant relationship to the distal tarsal row and through them to the remainder of the foot.
There is normally a slight overlap or convergence of the bases of the metatarsals on AP view (see Fig. 15.28). On a lateral projection, the central metatarsals should be superimposed, making it difficult to identify specific metatarsals—other than the short first and fifth metatarsals.
Plantar Arch
The longitudinal arch of the foot is identifiable on radiographs even in an infant, although at clinical examination the soft tissues and fat in the sole of the foot suggest flatness. The transverse arch causes the central metatarsals to be located dorsal to the more easily identified fifth metatarsal.
The plantar arch is best assessed on a lateral view by measuring the alignment of the hindfoot and metatarsals. On a lateral projection, the calcaneus is slightly dorsiflexed with the anterior end higher. The plantar angulation of the distal metatarsals completes the anterior portion of the arch.
The lateral talar-first metatarsal angle, also known as the angle of Meary, is used to measure the plantar arch in older children and adults. This is the angle formed between a line drawn along the central talus and a line drawn along the first metatarsal shaft. (The first metatarsal is easily distinguished because it is the shortest, widest metatarsal.) The Meary angle should be near zero (see Fig. 15.25). Normal values vary with age (see Table 15.3). As a general rule, an angle greater than 8° convex upward results in an exaggerated arch and pes cavus. An angle greater than 4° convex downward results in flattening of the plantar arch and pes planus or flatfoot.
2.4 Analysis of Foot Malalignment (Tables 15.2 and 15.3)
Table 15.2
Foot and ankle alignment terminology
Terminology | Meaning |
|---|---|
Ankle valgus | Slanting of articular surface of distal tibia, lateral side superior |
Ankle varus | Slanting of articular surface of distal tibia, lateral side inferior |
Ankle calcaneus | Increased dorsiflexion of calcaneus, anterior end higher |
Ankle equinus | Plantar flexion of calcaneus, anterior end lower |
Hindfoot valgus | Axial reference line of calcaneus deviates away from body’s midline on AP view of foot |
Hindfoot varus | Axial reference line of calcaneus deviates toward body’s midline on AP view of foot |
Pes cavus | Increased depth of plantar arch |
Pes planus | Flattening of plantar arch |
Metatarsus abductus | Metatarsals move away from midline |
Metatarsus adductus | Metatarsals move toward midline |
Foot eversion | Plantar surface faces laterally: pronation, abduction, dorsiflexion |
Foot inversion | Plantar surface faces midline: supination, adduction, plantar flexion |
Several terms are traditionally employed to describe foot alignment, as presented in Table 15.2. The following discussion supplies specific details about each type of malalignment of the ankle, hindfoot, midfoot, and forefoot. Table 15.3 presents normative data for angular relationships between the hindfoot, forefoot, and distal tibia.
Table 15.3
Normal hindfoot-forefoot angular relationships
Angle | Newborn | 2 years | 4 years | 6 years | 9 years |
|---|---|---|---|---|---|
AP view | |||||
Talocalcaneal | 42° (27–56°) | 40° (27–50°) | 34° (24–45°) | 30° (20–40°) | 18° (5–35°) |
Calcaneal-fifth metatarsal | 3° (−9 to +14°) | 0° (−10 to +10°) | −1° (−10 to +8° | 0° (−10 to +8°) | 3°(−8 to +15°) |
Talar-first metatarsal | 20° (+12 to +31°) | 15° (+2 to +27°) | 10° (−4 to +23°) | 7° (−7 to +20°) | 4° (−9 to +17°) |
Lateral view | |||||
Talocalcaneal | 39° (23–55°) | 41° (27–56°) | 44° (31–57°) | 44° (33–56°) | 40° (28–52°) |
Talocalcaneal (maximum dorsiflexion) | 45° (35–56°) | 44° (33–54°) | 43° (32–52°) | 42° (31–51°) | 41° (31–51°) |
Tibiocalcaneal | 77° (60–95°) | 72° (57–87°) | 68° (56–81°) | 67° (58–76°) | 68° (63–74°) |
Tibiocalcaneal (maximum dorsiflexion) | 42° (25–60°) | 48° (27–68°) | 50° (30–72°) | 51° (33–71°) | 50° (33–71°) |
Tibiotalar | 115° (86–145°) | 114° (95–130°) | 113° (100–122°) | 111° (101–118°) | 108° (89–123°) |
Talar-first metatarsal (Meary angle) | 18° (−2° to +44°) | 12° (−4 to +28°) | 8° (−5 to +22°) | 7° (−5 to +18°) | 7° (−7 to +20°) |
Talar-horizontal | 34° (14–55°) | 32° (18–45°) | 30° (20–40°) | 26° (20–36°) | 25° (13–35°) |
Ankle Alignment
Equinus (Talipes Equinus)
In a lateral projection, the calcaneus is plantar flexed, anterior end down, so that the angle of the axis of the calcaneus to that of the tibia exceeds 90° (Fig. 15.29), as opposed to the normal slight dorsiflexion of the anterior calcaneus (60–90°) (see Fig. 15.28).


Fig. 15.29
Equinus foot. The angle between the long axes of the calcaneus and tibia exceeds 90° (normal ranges from 60 to 90°) (simulated weight bearing)
Calcaneus Deformity
Calcaneus deformity of the hindfoot is determined on a lateral radiograph. For clarity, when discussing “calcaneus” deformity, it is helpful to refer to the bone as the os calcis. The os calcis is fixed in excessive dorsiflexion, with the anterior end higher than normal (Fig. 15.30); the tibiocalcaneal angle is less than 60°. The calcaneal position of the os calcis may contribute to the exaggerated plantar arch of pes cavus in a calcaneocavus deformity. This is commonly seen in S1 level myelomeningocele or polio patients who have paralysis of the gastrocsoleus muscle complex.


Fig. 15.30
Bilateral pes cavus. (a) (right), (b) (left). On both feet, the plantar arch is abnormally concave. The anterior margin of the calcaneus is directed superiorly (os calcis in “calcaneus”), and the metatarsals are abnormally plantar flexed. Note that this case illustrates the apparent flattening of the talus that is seen when the technologist “straightens” the foot, inadvertently causing obliquity of the ankle. On the right (a), a true lateral view of the ankle—with the fibula projecting over the middle of the tibia—the talar dome appears normally rounded, and the calcaneus is normally rectangular. On the left (b), performed with the ankle oblique as indicated by the dorsal position of the fibula, the talar dome appears to be flattened, as its convex contours are superimposed. The calcaneus appears square (weight-bearing views) (Courtesy of Rebecca Stein-Wexler; Copyright Shriners Hospital for Children Northern California)
Hindfoot
Hindfoot Valgus
The calcaneus rotates laterally under the talus so that its anterior part is lateral to the talus on AP radiograph. Its most posterior portion would be lateral to the center of the ankle when viewed from behind. Since it is difficult to get a true AP of the hindfoot, the following changes are conventionally identified on the standard weight-bearing AP and lateral foot views.
On an AP projection, the talocalcaneal angle is increased greater than 45°, since the calcaneus is laterally rotated from the midline. This gives the impression of medial deviation of the talus, so that a line through it points medial to the abducted first metatarsal base. However, the entire foot under and distal to the talus is abducted and everted (Figs. 15.25 and 15.31). The navicular moves with the calcaneus and if ossified appears displaced laterally from its normal position at the head of the talus.