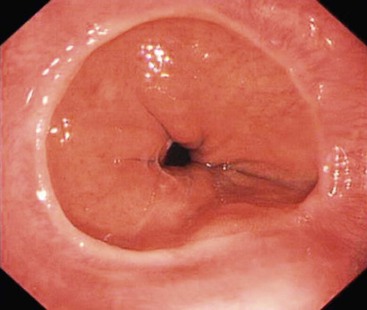
Edmund M. Godfrey, Alan H. Freeman The oesophagus is a fibromuscular tube that connects the pharynx in the neck to the stomach in the abdomen, traversing the thorax via the superior and posterior mediastinum. It begins below the cricopharyngeus muscle, at the lower edge of the cricoid cartilage and at the level of C6. In the neck, the oesophagus lies posterior to the trachea. As it descends through the mediastinum, it passes posterior to the aortic arch, the left main bronchus and the left atrium. At the diaphragm the oesophagus passes through the diaphragmatic hiatus at T10 accompanied by the vagus nerves, and ends at the gastric cardia at the level of T11. The abdominal oesophagus lies posterior to the left lobe of the liver. The oesophagus is therefore composed of a short cervical, a long thoracic, and short abdominal segments.1 In health, the oesophagus is lined by stratified, non-keratinising squamous epithelium. At the gastro-oesophageal junction there is an abrupt transition to columnar epithelium termed the ‘Z-line’ because of the irregular interdigitations between pale pink squamous and the darker columnar epithelia (Fig. 26-1). The gastro-oesophageal junction is usually found at a surprisingly constant 40 cm from the teeth. The wall of the oesophagus is made up of five layers: the mucosa, the muscularis mucosa, the submucosa, the muscularis propria and adventitia. The stratified squamous epithelium of the oesophagus, together with its associated submucosal glands, is derived from the endoderm of the foregut. The striated muscle of the upper oesophagus is derived from branchial arches 4 and 6, whereas the smooth muscle of the lower oesophagus is derived from somite mesenchyme. The myenteric plexus is derived from neural crest cells. The oesophagus actively moves ingested material from the pharynx to the stomach, and to prevent reflux of stomach contents. Ingested material may also pass in the opposite direction during vomiting. Passage of a food bolus is regulated by the upper and lower oesophageal sphincters. The upper oesophageal sphincter is a high-pressure zone at the pharyngo-oesophageal junction and comprises cricopharyngeus, thyropharyngeus and the superior part of the cervical oesophagus.2 The lower oesophageal sphincter is a 2- to 3-cm high pressure zone at the gastro-oesophageal junction and is composed of the lower oesophageal muscle fibres and the diaphragmatic hiatus.3 The gastro-oesophageal junction is anchored by the phreno-oesophageal, gastrosplenic, phrenicolienal and gastrophrenic ligaments. The important phreno-oesophageal ligament (or membrane) allows the oesophagus to slide longitudinally through the diaphragmatic hiatus whilst acting as a seal between the thoracic and abdominal cavities.4 Unlike the upper and lower oesophageal sphincters, the muscle of the interposed oesophageal ‘body’ is relaxed in the resting state. The swallowing reflex induces so-called primary peristaltic (or stripping) waves that travel at 3–4 cm/s. Secondary peristalsis occurs when oesophageal sensory receptors are activated by material persisting in the oesophagus after primary peristalsis. Tertiary contractions are non-propulsive and are seen in a variety of motility disorders5 (Fig. 26-2). A further motility disturbance is the so-called feline oesophagus (Fig. 26-3). This takes the form of small horizontal transient contractions that are thought to arise from the muscularis mucosa. This finding, also known as the oesophageal shiver, is a normal feature of the cat’s oesophagus, hence the term. The oesophagus can be examined with any of the commonly used imaging techniques. The initial test of choice is usually endoscopy, with fluoroscopy reserved for frail patients, those with suspected motility disorders, or after surgery. Computed tomography (CT) is often the first-line test in the context of trauma. Imaging is extensively used in the staging of oesophageal malignancy, particularly CT, positron emission tomography CT (PET-CT) and endoscopic ultrasound (EUS). In most circumstances, plain radiographs reveal little useful information regarding the oesophagus, except in the context of foreign body ingestion.6 Foreign bodies tend to lodge at one of the oesophageal constriction points: Otherwise a dilated, gas- or fluid-filled oesophagus (Fig. 26-4) may be identified incidentally during chest radiography for other indications. The majority of the oesophagus is inaccessible to conventional ultrasound examination. The short cervical and abdominal segments are amenable to imaging in this way, but this is rarely used in clinical practice. Fluoroscopic examination of the oesophagus is frequently performed for a wide variety of indications. Barium suspensions are preferred for most indications; a density of 100% w/v is often used to provide a balance between good mucosal coating and not being too dense. If possible, double-contrast images should be obtained using an effervescent agent, usually in the erect position. These are complimentary to prone, single-contrast images. Water-soluble contrast medium is used initially when a tear, perforation or anastomotic leak is suspected. Low osmolar agents such as Gastromiro (iopamidol) should always be used to prevent pulmonary oedema, which can occur following aspiration of high osmolar agents such as Gastrografin (meglumine diatrizoate). In some institutions, when a leak is suspected, water-soluble contrast medium is followed with a barium suspension. Using barium in this way has been shown to be more sensitive for contained perforations, although it adds nothing in the detection of free leakage into the neck or mediastinum.7 Fluoroscopic examination of the oesophagus is tailored to the indication, but a suggested technique is as follows: control images should be obtained if the patient has had oesophageal or gastric surgery. In the erect position, double-contrast images are obtained in the lateral and PA projections of the cervical and upper oesophagus at 4 images per second. Right anterior oblique images of the mid and lower oesophagus are obtained at 2/s, also in double contrast. The patient is then moved to the prone position and images are obtained at 1/s during three separate, single bolus swallows to assess oesophageal motility and fully distend the gastro-oesophageal junction. The images obtained in the prone position are usually single contrast. Finally, a static image of the stomach to include the gastric fundus is obtained in the erect position. The standard fluoroscopic examination may be augmented with additional procedures. As an example, where a patient describes a clear history of dysphagia but the images obtained appear normal, a swallow of biscuit dipped in barium or a barium tablet may uncover an occult stricture. If there are pharyngeal symptoms, images of the pharynx obtained during phonation are obtained. Although no longer the first-line test for dysphagia, fluoroscopy remains an important test. It is well suited to evaluate motility disorders, the oesophagus following trauma or surgery, complex hiatal herniae and as a less invasive alternative to endoscopy in the frail, elderly patient (Fig. 26-5). Oesophagogastroduodenoscopy or ‘endoscopy’ is the initial investigation of choice for most oesophageal indications, particularly dysphagia. It permits the direct visualisation of the mucosa and, crucially, biopsies can be taken. In patients with high dysphagia, preliminary fluoroscopic assessment can be used to forewarn the endoscopist of a pharyngeal pouch, which hopefully reduces the risk of perforation. For the procedure the patient is placed in the left lateral position. Increasingly, diagnostic endoscopy is performed without sedation, using pharyngeal local anaesthetic spray. Sedation with a short-acting benzodiazepine (e.g. midazolam) is an alternative for diagnostic procedures, and is preferred when intervention is planned. In addition to a detailed diagnostic assessment of the mucosa, a wide variety of therapeutic manoeuvres may be carried out endoscopically. The most common of these is the treatment of upper GI haemorrhage, which may be carried out using a variety of different techniques. Elective procedures include balloon dilatation and/or stenting of strictures, radiofrequency ablation (RFA) of dysplastic or malignant epithelium and injection of botulinum toxin for motility disorders. Endoscopic mucosal resection (EMR) deserves special note, as it is both therapeutic and the preferred method for staging early oesophageal tumours.8 In the context of oesophageal disease, CT is most widely used in the staging of oesophageal cancer. A CT of the thorax, abdomen and pelvis should be acquired.8 Good oesophageal and gastric distension is important: the patient should be given 1–1.5 L of water to drink as well as effervescent granules, and be imaged in the prone position. Intravenous contrast medium should be used whenever possible, with the upper abdomen imaged in both the arterial and portal venous phases. For the investigation of patients with suspected oesophageal trauma (including Boerhaave’s syndrome) and in the postoperative setting, positive oral contrast medium is required. As for fluoroscopic examinations, this should always be a low osmolar agent. For suspected tracheo-oesophageal fistula, an initial acquisition without the use of oral contrast medium is usually diagnostic (Fig. 26-6). In current clinical practice, magnetic resonance imaging (MRI) is not used for imaging the oesophagus. Whether MRI may be useful for tumour or nodal staging in oesophageal cancer is an area of current research (Fig. 26-7). The highest spatial resolution imaging of the oesophagus is obtained using endoscopic ultrasound. This technique uses a high-frequency (7–12 MHz) ultrasound probe mounted at the end of an endoscope (an ‘echoendoscope’). A radial echoendoscope produces ultrasound images that are perpendicular to the axis of the scope and is used for oesophageal cancer staging. A linear echoendoscope produces images parallel to its axis and it is this type of instrument that is used for EUS-guided fine needle aspiration (EUS-FNA).9 EUS is generally used to characterise abnormalities identified using other imaging techniques, in particular the staging of oesophageal cancer. Less frequently, EUS is used for the assessment of submucosal lesions of the oesophagus. The high frequency and close proximity of the ultrasound probe allow the delineation of five layers of the oesophageal wall: mucosa, muscularis mucosa, submucosa, muscularis propria and adventitia. The muscular layers are hypoechoic; hence, there is a five-layered alternating pattern. EUS-FNA allows sampling of structures deep to the oesophageal mucosa, particularly thoracic and upper abdominal lymph nodes. This can be particularly useful in the staging of oesophageal and lung malignancy, and in the diagnosis of tuberculosis. For patients with oesophageal cancer, F18-fluorodeoxyglucose (FDG) PET-CT is now the standard of care if radical treatment is intended.8 This is largely because of the high proportion of patients that have unsuspected metastatic disease at presentation (Fig. 26-8), and the superiority of PET-CT over other techniques for identifying it.10 The improved anatomic localisation of integrated PET-CT means that it is preferable to separate PET and CT acquisitions. Technetium-based radionuclide imaging of the oesophagus can be used for the identification of oesophageal motility disorders and gastro-oesophageal reflux disease (GORD). Patients can be imaged swallowing both liquid and solid material (usually 99mTc-labelled sulphur colloid and scrambled egg, respectively) (Fig. 26-9). Oesophageal cancer is the sixth most common cause of death from cancer in the UK. There are two major histological types: squamous cell carcinoma and adenocarcinoma. Although the squamous type has been more common historically (and still is worldwide), in the West it has been overtaken by adenocarcinoma due to the rise in obesity.11 Accurate preoperative staging of oesophageal cancer is difficult. The mobility of the oesophagus and its proximity to other organs make the assessment of local invasion problematic. Malignant lymph nodes are usually not enlarged,12 and may first arise some distance from the tumour.13 Furthermore, unsuspected metastases may be present in up to 30% of patients at diagnosis.14 It is not surprising then that a variety of different tests are required for accurate staging. The patient with oesophageal cancer can face a whirlwind of tests, including endoscopy, CT, EUS and PET-CT. This combination is crucial for determining appropriate therapy. Initial diagnosis is usually with endoscopy as it permits histological confirmation with biopsy (Fig. 26-10). Despite this, a good-quality fluoroscopic examination can detect even early tumours (Fig. 26-11). If a stricture is identified using fluoroscopy and appears unequivocally benign, with symmetrical, smooth narrowing and a gradual tapering to normal calibre, malignancy can be confidently excluded.15 The converse is also true: strictures with an ulcerated, irregular mucosa and shouldered, shelf-like margins can be considered malignant on imaging appearances alone. The vast majority of patients will go on to CT as their initial staging investigation. Although less sensitive than EUS and PET-CT, it is relatively specific for identifying locally advanced or metastatic disease. Patients with these findings on CT are therefore spared further staging investigations. In the case of early tumours that appear to be T1 endoscopically, endoscopic mucosal resection (EMR) is the preferred initial staging technique.8 The introduction of the seventh edition of the TNM classification has resulted in a number of changes to oesophageal cancer staging: 2. T4 disease has been subdivided into resectable (T4a) and non-resectable (T4b) disease. 3. Positive nodal disease has been subdivided into N1, N2, and N3. 4. Coeliac axis (Fig. 26-12) and perioesophageal cervical lymph nodes (Fig. 26-13) have been reclassified as regional nodes rather than metastases.
The Oesophagus
Anatomy and Function
Anatomy (Table 26-1)
Embryology
Function
Examination
Plain Radiography
Ultrasound
Fluoroscopy
Endoscopy
CT
MRI
Endoscopic Ultrasound
Radionuclide Radiology Including PET-CT
Pathological Features
Oesophageal Cancer

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


The Oesophagus
Chapter 26