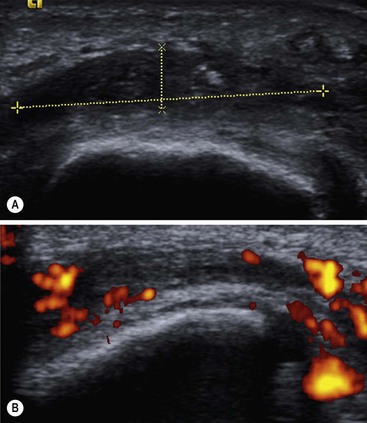
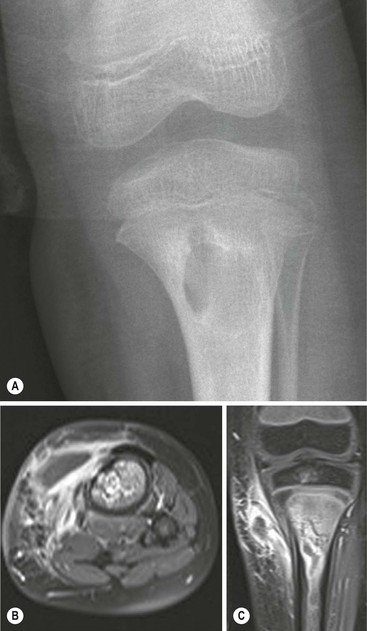
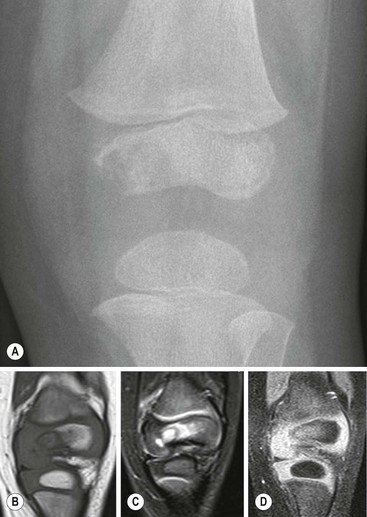
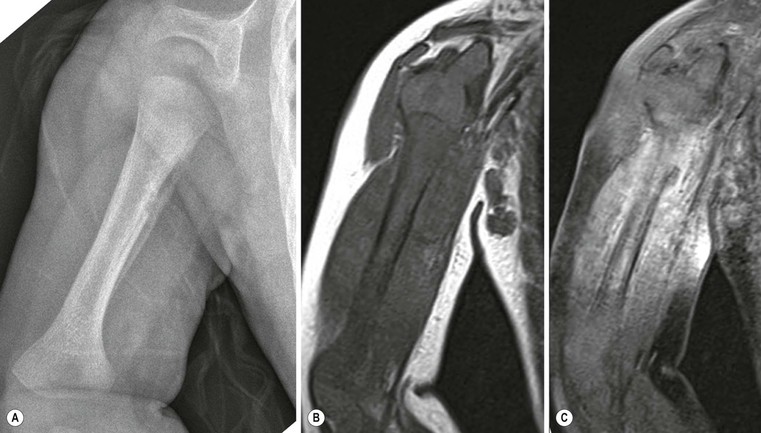
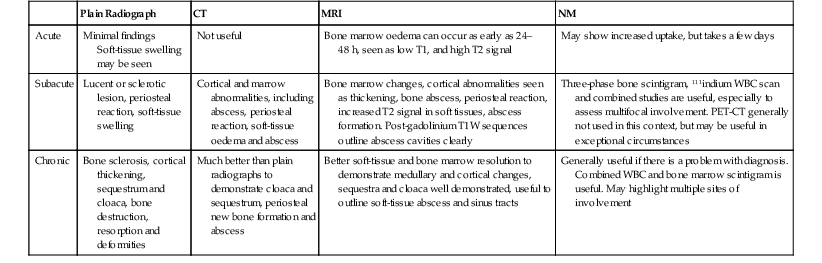
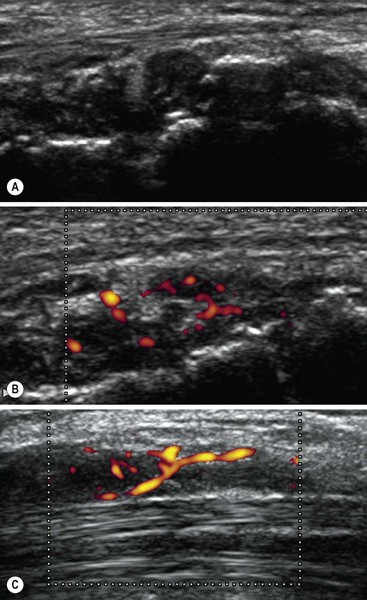
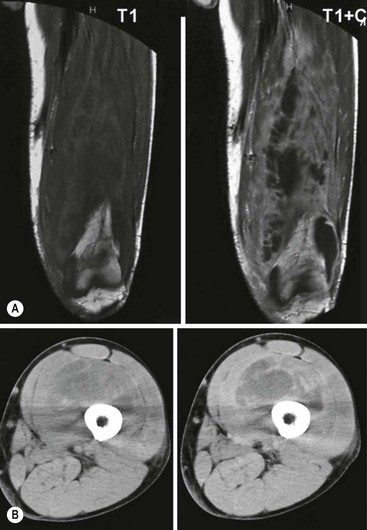
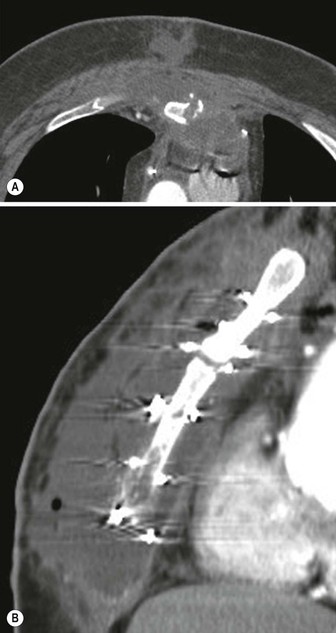
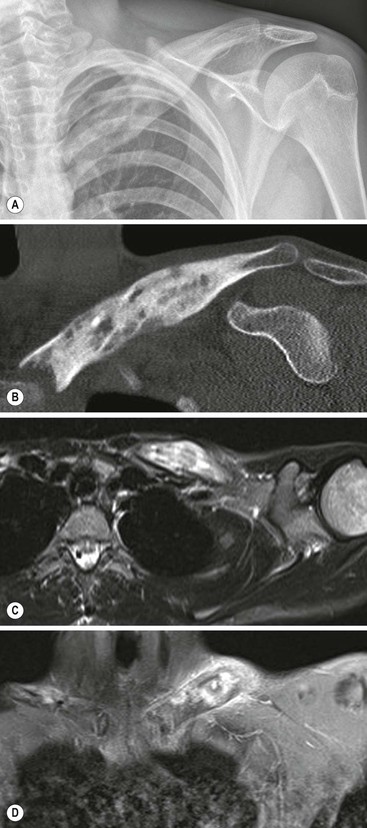
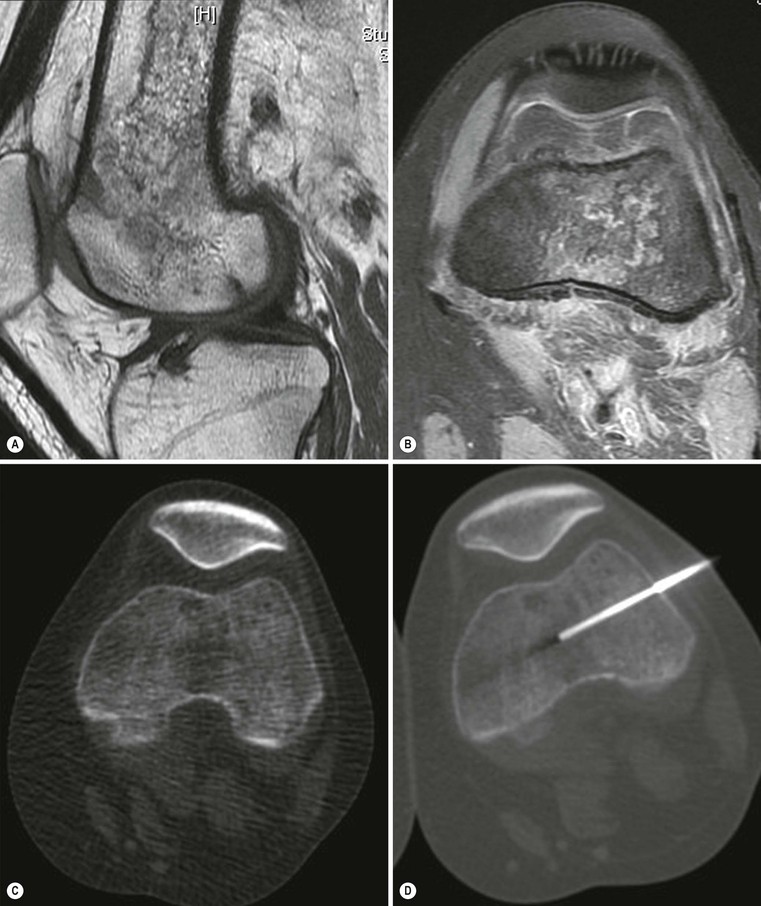
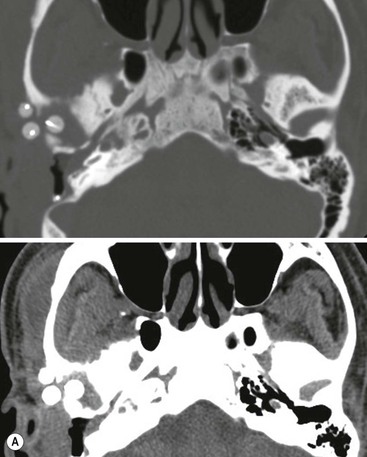
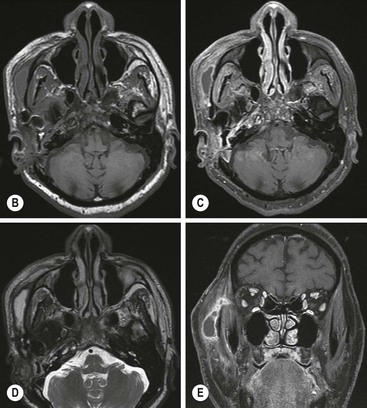
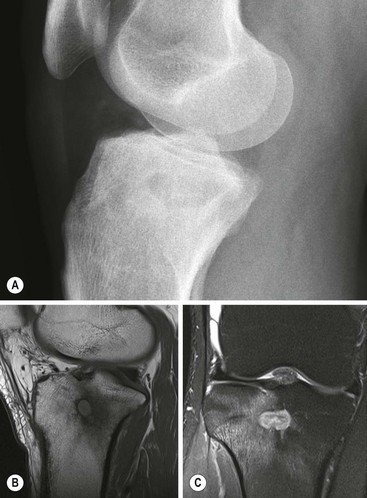
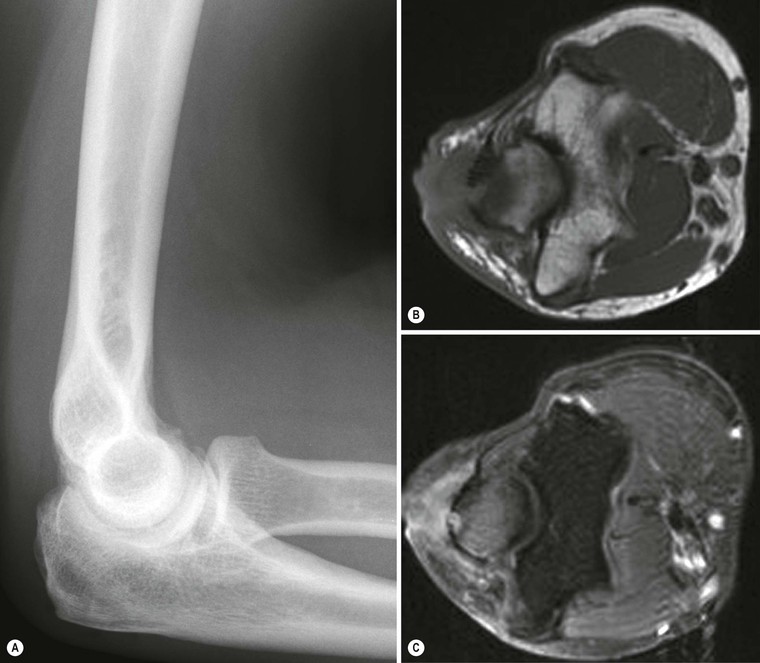
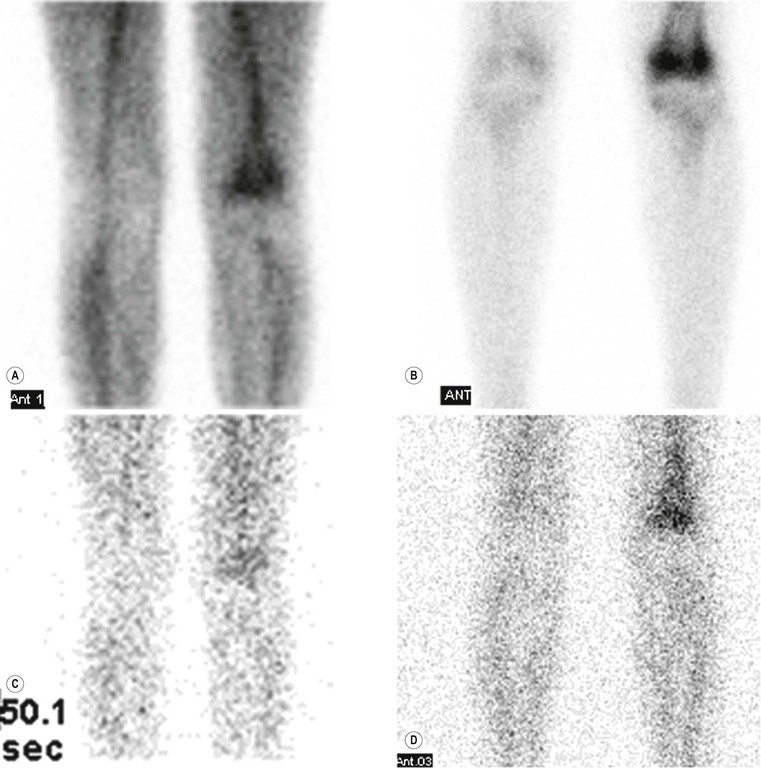
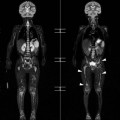
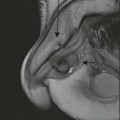
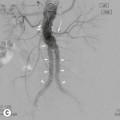
Balashanmugam Rajashanker, Richard W. Whitehouse Bone and joint infections have high rates of morbidity and occasional mortality. A wide range of microbial infections can affect bones and joints, including pyogenic, mycobacterial and fungal organisms. Patients usually present with a high temperature, pain and swelling in the affected bones and/or joints. In younger patients concomitant systemic illness more often occurs. Early diagnosis at acute presentation is important to prevent chronic and recurrent infections, long-term disabilities and treatment failures. Prompt diagnosis is needed particularly in children and also after orthopaedic implant surgeries to prevent the risk of developing serious infections. A multidisciplinary team approach is necessary for effective management of these conditions. Soft-tissue and muscle infections present more acutely and may be potentially life threatening. It can be difficult to diagnose bone infection early, especially in diabetic patients with pre-existing neuropathic bone and joint changes and in the presence of skin ulceration and cellulitis. A high degree of suspicion and use of appropriate investigations will assist diagnosis. Tuberculous infection of bones and joints pose a particular diagnostic challenge. Septic arthritis is a serious condition, which if untreated leads to destruction of cartilage and adjacent osteomyelitis, with subsequent joint ankylosis and disability. Laboratory tests including white cell count, C-reactive protein, ESR and blood culture are mandatory in the early stages to diagnose these infections. A range of radiological investigations are available currently to enable a prompt diagnosis. It is important that the radiologist is familiar with the clinical spectrum of presentations, appropriate diagnostic tests and the need to perform these without delay to enable prompt management. Staphylococcus aureus is the commonest organism causing bone and joint infections in any age group, accounting for up to 80% of cases of osteomyelitis. Gram-negative organisms including Pseudomonas and Enterobacter are responsible for most of the remaining 20% of cases. Acute infections of prosthetic implants are usually caused by S. aureus. Coagulate-negative staphylococci such as Staphylococcus epidermidis account for the majority of chronic osteomyelitis associated with orthopaedic implants and account for approximately 90% of pin tract infections. Bacteria adhere to bone matrix and orthopaedic implants via receptors to fibronectin and other receptor proteins. They form a slimy coat and elude the host defence mechanisms by hiding intracellularly and by developing a slow metabolic rate.1 Osteoarticular Listeria infections are rare but do occur in immunocompromised patients and in prosthetic joints.2 Polymicrobial infection occurs in the majority of osteomyelitidies occurring in the diabetic foot, comprising of mixed Gram-positive and -negative bacteria. Wound swabs are often inaccurate and dominated by contaminants. Cultures from bone biopsy or operative specimens are more reliable in planning appropriate antibiotic treatment.3 Brodie’s abscess, a true small, focal intraosseous collection of pus, is an uncommon manifestation of bone infection, except in East Africa, where reportedly it is a common occurrence.4 Staphylococcus aureus is again the predominant organism cultured in these patients. Vertebral osteomyelitis usually results from haematogenous seeding or by direct inoculation at the time of spinal surgery. Staphylococcus aureus is the commonest microorganism amongst others that include methicillin-resistant S. aureus (MRSA), streptococci and E coli.5 As with other orthopaedic implants, coagulase-negative staphylococcal infections are seen after usage of fixation devices.6 In children, other than staphylococci, Haemophilus influenzae type b, Streptococcus pneumoniae and Streptococcus pyogenes also occur.7 One of the significant changes in the epidemiology of bone and joint infections is the increasing incidence of MRSA and the emergence of multidrug resistant (MDR) organisms.8,9 Osteomyelitis complicating war injuries is predominantly caused by MDR organisms and include MRSA, Enterobacteriaceae and Acinetobacter. There is commonly a history of previous surgical procedures and these conditions usually need further more aggressive management.10 Fungal infections of the bone and joints are uncommon and occur predominantly in the immunosuppressed patient. Such infection may resemble tuberculous disease and present as chronic multifocal osteomyelitis or polyarthritis.11 Osteomyelitis can be classified by the type of infection or more commonly by the duration since onset of the illness. Acute osteomyelitis is defined as infection diagnosed within 2 weeks of onset of symptoms whilst subacute osteomyelitis is diagnosed if symptoms exceed 2 weeks’ duration. If the infection is diagnosed months after the onset of symptoms, then it is defined as chronic osteomyelitis.12,13 There are, however, other classifications in the literature, depending on the anatomical areas of bony involvement and on pathogenesis.14,15 Paediatric, unlike adult, bone infections more commonly occur in healthy bones, without pre-existing trauma, etc. The usual mode of infection is haematogenous, via the arterial blood supply. Acute haematogenous osteomyelitis (AHO) is the most common form of bone infection in children. About 50% of cases occur in children less than 5 years of age and it is twice as common in boys than in girls. Immunocompromised children and children with underlying haematological disorders such as sickle cell disease are more prone to these infections.16 Infections are commonest in long bones such as the femur, tibia or humerus, with most cases limited to single bone involvement. Less than 10% of cases involve two or more locations,17 the corollary of which is that multifocal involvement does not exclude acute osteomyelitis (the same is true for septic arthritis). Haematogenous spread is the most common route to bones and joints, though implantation at trauma or surgery and spread from contiguous infection may also occur. Infection usually starts in the metaphysis due to its rich blood supply. From here the infection may spread to the bone cortex and penetrate the loosely attached periosteum, eliciting a periosteal reaction. It may perforate the periosteum and spread to adjacent muscles and soft tissues, forming abscesses. Less commonly, the infection may spread to the epiphyseal plates and joints, causing septic arthritis. In neonates, the metaphyseal capillaries form a connection with the epiphyseal plate, thus increasing the chance of joint infection. In later infancy, these vessels atrophy and there is thickening of the cortex, thus reducing the risk of growth plate involvement and septic arthritis. Staphylococcus aureus accounts for approximately 60–90% of childhood AHO, followed by group A β-haemolytic streptococci (10%). Other causes include H. influenzae and S. pneumoniae. Salmonella infections were historically common in patients with sickle cell disease but this seemed to reflect the organism prevalence in the population. Pseudomonas infections can be seen after puncture wounds of the feet. In neonates, again, S. aureus infections predominate, but group B streptococcus and E. coli infections are also common.16,18 A few well-recognised clinical presentations of bone and joint infections are seen in children. Acute osteomyelitis, more common in boys, usually occurs between ages 1 and 10 years. The lower limbs are usually involved. Children usually present with pain and reluctance to use the affected limb. The cardinal signs of acute inflammation, including pain, redness and swelling, may not be present initially, may develop later and may be associated with systemic illness. Often pain is localised and prompt diagnosis and treatment offers a good prognosis. Chronic osteomyelitis has a more insidious onset over a few weeks and is more difficult to diagnose. There is usually minimal loss of function. Systemic signs are usually absent, but local tenderness may be present. Radiographs are usually helpful as bone changes are usually present by the time medical attention is sought. Chronic osteomyelitis is further discussed under adult infections. Septic arthritis is also twice as common in boys, with a peak incidence below 3 years of age. Symptoms include pain and swelling around the joint with reluctance to move the limb. Pseudo-paralysis and painful passive movements may be present. There are systemic symptoms and there is rapid progression of symptoms. Diagnosis is more difficult in neonates. The joint is warm and ultrasound can demonstrate a joint effusion. The lower limbs are usually involved, particularly the hip or knee. Neonatal osteomyelitis and septic arthritis are probably different manifestations of the same condition: 75% of the children are not severely ill and present as failure to thrive. Prognosis is not as good as there is usually a delay in diagnosis. Disseminated staphylococcal disease presents as a rapidly progressive severe life-threatening illness with virulent bacteraemia and multiorgan involvement, but fortunately is rare. Thorough clinical examination and laboratory investigations are extremely important in diagnosis, before imaging evaluation is performed. Conventional radiography is still one of the most important investigations for diagnosis. The other imaging investigations, ultrasound, CT, MRI and scintigraphic studies are also used. The risk/benefits and costs of these tests, their radiation exposure, requirements for sedation or anaesthesia need to be assessed carefully as investigations are planned. In acute osteomyelitis, plain radiographs are extremely useful to exclude other lesions such as fractures, Perthes’ disease and slipped femoral epiphysis. In septic arthritis the joint space is initially expanded with fluid and may give rise to some asymmetry in the position of the epiphysis, but ultrasound is more reliable to demonstrate fluid in the joint. In subacute osteomyelitis, periosteal reaction, new bone formation and occasionally lucent lesions (Brodie’s abscess) in the metaphysical region may be seen. Chronic osteomyelitis shows bone sclerosis, destruction, and periosteal new bone formation. Ultrasound has an important role in demonstrating increased joint fluid early in acute septic arthritis and is also used to guide aspiration of the joint effusion for diagnostic and therapeutic purposes (Fig. 53-1). In septic arthritis the cellular debris-laden effusion may be echoic, rendering it less conspicuous. Demonstrating movement of this debris by varying the US probe pressure during the examination may reduce false-negative interpretation. Subperiosteal abscess can be demonstrated as hypoechoic fluid along the bone surface in acute and subacute disease. Soft-tissue abscesses can also be seen as hypoechoic fluid with thick walls that may show increased colour Doppler flow. Direct aspiration under ultrasound guidance and culture and sensitivity of the aspirate is extremely helpful to confirm diagnosis and for further treatment with the appropriate antibiotics. Soft-tissue abnormalities can also be demonstrated with ultrasound, though MRI is more reliable. This investigation is less useful in a paediatric population due to its radiation dose and lack of specific advantages, and MRI is preferred. MRI is the investigation of choice for the diagnosis of acute, subacute and chronic osteomyelitis with high sensitivity and specificity. The characteristic signs of acute osteomyelitis in children include bone marrow oedema, which is seen as low T1 signal in the bone marrow, along with high signal on T2 and STIR images.19 Abscesses are seen both early and late in disease, as well-defined low-signal collections on T1, high signal similar to fluid on T2 images, with enhancing walls on post contrast sequences (Fig. 53-2). This may be seen in the bone, adjacent soft tissues or subperiosteal location due to the loose attachment of the periosteum to the underlying bone in children. Septic arthritis is diagnosed by the presence of a joint effusion, abnormal bone marrow signal localised to either side of the joint or synovial thickening which also shows post contrast enhancement. Physeal involvement is characterised by low T1 and hyperintense T2 signal along the growth plate associated with widening of the growth plate and enhancement on post contrast imaging (Fig. 53-3). Later in the course of the infection, chondrolysis occurs. Fat-saturated T1-weighted (T1W) images with intravenous contrast medium can increase confidence in the diagnosis of osteomyelitis and also help diagnose complications such as septic arthritis, physeal involvement, intra-osseous, subperiosteal and soft-tissue abscesses. Intravenous gadolinium is most useful to identify non-enhancing abscess collections within a background of soft-tissue and bone marrow oedema and to aid differentiation between granulation tissue and true abscess. It is generally not useful if unenhanced images show no evidence of soft-tissue or bone marrow oedema. The merits of administering intravenous contrast agents should be weighed against its injudicious use in children.20 The rim sign is seen in chronic osteomyelitis as a low-signal area of fibrosis surrounding an area of active infection. Active infection has high signal on T2, whereas the rim has low signal on all sequences. There may also be thickening and remodelling of cortex due to chronic infection. Periosteal reaction may not be present at this stage. Bone abscess is seen as fluid signal surrounded by a thick wall that has low signal on T1 and significant enhancement. Abscesses may extend through the cortex into the surrounding soft tissues with the formation of sinuses. There is high T2 signal return from surrounding soft tissues, with loss of normal fat signal on T1 and T2 images (Fig. 53-4). Post-surgical or interventional procedures cause bone signal changes that can persist for up to 12 months. Hence, whenever possible, MRI should be obtained before any interventions are performed, to avoid the need for additional procedures.21 Whole-body MRI may be useful to demonstrate multiple sites of involvement. In early stages, three-phase 99mTc-MDP skeletal scintigraphy may be useful for demonstrating increased radioactivity in the affected bone and also for demonstrating multifocal disease. Increased activity may be seen in dynamic perfusion, early blood pool and delayed images. However, such uptake is non-specific and may be seen in other conditions including trauma and tumours. Use of Ga-67 citrate and 111indium-labelled leucocytes will increase the specificity for infection up to 80%.13 This uncommon form of non-bacterial inflammatory osteomyelitis occurs in children, usually less than 18 years of age. The aetiology is not known, but may be related to autoimmune disorders due to its association with inflammatory bowel disease and psoriasis-like skin conditions. A genetic aetiology is also postulated due to an association with mutation of the LPIN2 gene. It is characterised by recurrent bouts of inflammatory arthritis and features of osteomyelitis which undergo spontaneous remission. It is more common in the lower limbs and may be symmetrical. Metaphyseal lesions occur in approximately 75% of cases. Symptoms are vague and it may present as monoarthritis or polyarthrits. When a single site of disease is present, the term chronic non-bacterial osteomyelitis is used.22 There may be mild elevation of inflammatory markers but lab diagnosis is generally not helpful. Cultures do not reveal any organisms. Plain radiographs may reveal osteolytic lesions with surrounding sclerosis. Whole-body MRI can be helpful by identifying multiple sites of the disease, some of which may be asymptomatic. Typically MRI reveals periostitis, bone marrow oedema and signs of transphysitis.23 Many lesions may heal spontaneously, though symptoms may persist for several years. Diagnosis is made by exclusion and from clinical history and typical radiological findings affecting multiple sites and recurrent negative cultures and bone biopsy. Majeed syndrome is an autosomal recessive disorder comprising a triad of CRMO, congenital dyserythropoietic anaemia and inflammatory dermatosis. This is considered as a form of CRMO and occurs in children and young adults, commonest between the second and third decades of life.23 It is characterised by the presence of synovitis, acne, pustulosis, hyperostosis and osteitis (SAPHO). Skin manifestations and osteoarticular involvement commonly occur. Skin manifestation includes palmoplantar pustulosis and acne. There is bilateral symmetric pain and swelling of the bones and joints. The metaphyses of the tubular bones are commonly affected, though flat bones and axial skeletal sites may also be affected. Biopsy demonstrates acute and chronic inflammatory cells. Relationship to Propionibacterium acnes has been postulated but is debatable.24 Treatment is by non-steroidal anti-inflammatory drugs (NSAIDs) in the first instance but severe cases may need immunosuppressive treatment. This is a chronic form of osteomyelitis, usually occurring in children, and commonly affects the mandible. This is considered as a form of CRMO affecting the mandible. Patients present with pain and hard swelling of the mandible. Initial findings include lytic lesions of the mandible associated with sclerosis. With disease progression there is non-suppurative ossifying periostitis with subperiosteal new bone formation and sclerosis.25 The diagnosis can be made presumptively by radiology, and biopsy reveals features of chronic osteomyelitis, with cultures usually negative.23 This is a rapidly progressive life-threatening infection occurring in young children and more common in males. This condition also occurs in adults. Risk factors include immunocompromise, diabetes, intravenous drugs or alcohol abuse and patients with peripheral vascular disease. The condition is polymicrobial in origin, and includes Gram-positive aerobes like group A β-haemolytic streptococcus, S. aureus, Gram-negative organisms like E. coli, Pseudomonas aeruginosa and anaerobes like Bacteroides. Clostridium infection leads to a gas-producing necrotic infection, gas gangrene, which is rapidly progressive and leads to systemic toxicity and shock. Characteristically, the gas is intramuscular in gas gangrene, giving rise to gas loculi that are elongated and aligned with the muscle fascicles, whilst more globular gas loculi are seen in fasciitis, when a gas-forming organism is present. The infection involves deep subcutaneous tissues and is associated with a high mortality. Infection causes thrombosis of small blood vessels, leading to necrosis and rapidly involving several facial planes. The condition has been associated with trauma, burns, eczema and varicella infections. The extensive soft-tissue damage leads to multi-organ failure and shock.26 Ultrasound can be useful in diagnosing the abnormal muscle echo texture, but MRI is more reliable and is needed to assess the extent of tissue damage and demonstrate the spread of infection along the facial planes. CT may also be useful, but MRI is preferred due to better soft-tissue contrast and lack of radiation. Emergency surgical debridement is needed to stop the progress of this fulminating condition; relevant imaging must therefore be performed immediately. Spontaneous musculoskeletal infections in adults are less common than in children and are usually due to trauma, previous surgery or underlying immunodeficiency disorders. Trauma and open wounds can result in seeding of bone with microorganisms and to development of osteomyelitis. Whilst haematogenous infection is common in childhood osteomyelitis, in adults, it is mostly responsible for vertebral osteomyelitis. Apart from trauma, infection can also develop in prosthetic implants after surgery. Underlying conditions like diabetes, vascular insufficiency, decubitus ulcers and sinuses can predispose to development of osteomyelitis in adults. Osteomyelitis is classified by the time since onset, as described earlier.27,28 Healthy adult bone is usually resistant to infection, but when affected can be difficult to treat. The presence of dead bone and implants make it difficult to treat by anti-microbial agents and removal of the debris and the prosthetic implants is necessary to eradicate the infection. The bacteria attach to the bone matrix and orthopaedic implant devices by developing receptors to fibronectin and other structural proteins. They develop a slimy coat and a very slow metabolic rate, hide in intracellular locations and are thus able to elude host defences and antibiotics. The presence of implants also causes cell dysfunction which decreases the ability of polymorphonuclear cells to phagocytise bacteria. Reactions between the bacteria and the host defences cause release of cytokines and consequent osteolysis.29 Patients with sickle cell disease are prone to developing enteric bacterial osteomyelitis. In sickle cell disease, there is impaired gut defence due to sickling in the vasculature of gut. This enables the entry of organisms into the bloodstream, and haematogenous spread of infection into the bones. Typically this is Salmonella infection but this probably reflects the prevalence of Salmonella in countries where sickle cell disease is common.30 Clinical features are variable, but acute infections generally present with pain, swelling and redness of the affected area associated with systemic illness. Joint swelling, reduced mobility and features of overlying cellulitis may be present. In chronic infections, discharging sinuses may be present. Treatment may render chronic osteomyelitis inactive, but reactivation may occur, with recurrence of symptoms (pain, swelling, erythema, fever) and new radiographic features (bone destruction, periosteal reaction). Characteristic radiographic features of chronic osteomyelitis include intraosseous cavities which may contain separated fragments of necrotic bone (a sequestrum) with the surrounding bone becoming thickened and sclerotic (involucrum). The cavity may communicate with the surrounding soft tissue through cloacae in the involucrum, with sinus tracks to soft-tissue abscesses or cutaneous ulcers. Extrusion of sequestra may occur through these sinuses. Laboratory investigations may demonstrate an increased white cell count, elevated C-reactive protein and ESR. In acute infections blood cultures may be positive. Culture of the pus from discharging sinuses is also useful, but generally has a low yield rate for microorganisms. Table 53-1 summarises the main imaging findings in acute, subacute and chronic osteomyelitis. In acute infections, plain radiographs are useful to exclude other lesions such as fractures or malignancy. Focal abnormalities occur in acute osteomyelitis, usually in the metaphyseal region. These are commonly lytic lesions with a narrow zone of transition but bone sclerosis can also occur. There may be associated soft-tissue abnormalities. In subacute osteomyelitis, periosteal reaction and cortical thickening also occur. As the disease progresses, bone sclerosis, thickening, resorption and destruction resulting in deformities may occur (Fig. 53-5). Septic arthritis can destroy the joint, resulting in joint fusion and deformities. Ultrasound is a simple, non-expensive bedside investigation that can be extremely useful in the acute setting with ease of performing interventions in the same setting. Cellulitis is easily demonstrated as oedema and thickening of the subcutaneous tissues.31 This creates a cobblestone pattern due to anechoic strands randomly traversing the subcutaneous tissues. Infective bursitis is demonstrated by the presence of excess fluid in the bursa, wall thickening with increased colour Doppler flow due to inflammatory changes in the affected bursa. Prepatellar and olecranon bursae are the most commonly affected. Fluid aspiration for diagnosis by microscopy and culture under ultrasound guidance also offers therapeutic benefit. Tenosynovitis shows thickening of the tendon sheath associated with fluid surrounding the tendon itself. There may be non-compressible thickening of the tendon sheath which also demonstrates increased colour Doppler flow due to hyperaemia.32 It is difficult to differentiate inflammatory tenosynovitis from infection, and aspiration and cytology will confirm the diagnosis (Fig. 53-6). In the appropriate clinical setting, septic arthritis is confirmed by the presence of fluid in the affected joint and can usually be readily demonstrated by ultrasound, though turbid fluid may be echogenic and more difficult to see. Ultrasound is particularly useful in the hip, where guided diagnostic aspiration can be performed. Early diagnosis can avoid serious consequences, especially in children, where an effusion can be the only sign localising infection to that joint. In the hands, wrists and feet joints, diagnostic aspiration under ultrasound reduces the risk of contamination of other compartments.26 Thickening of the synovium is seen in septic arthritis associated with lack of compressibility and increased colour Doppler flow due to the presence of inflammation, but can also be seen in other inflammatory and non-inflammatory arthritis. Abscesses are usually well defined and show hypo-echoic or anechoic fluid within, usually with a thick capsule which shows increased Doppler flow. Subperiosteal abscesses can also be demonstrated by ultrasound before a periosteal reaction is evident radiographically, but osteomyelitis generally needs further cross-sectional imaging. Pyomyositis shows abnormal echogenicity in early stages, but in later stages abscess formation is seen (Fig. 53-7). With prosthesis-related infection, ultrasound can be extremely useful to demonstrate fluid collections and diagnostic aspiration can be performed at the same time. High-resolution, multiplanar reconstruction and wide availability result in CT being commonly used in the diagnosis and assessment of osteomyelitis. The main disadvantages of CT are exposure to ionising radiation and limited soft-tissue contrast. The advantages of CT are that it can demonstrate periosteal reaction, subtle bone erosion, cortical destruction, abscess formation and soft-tissue swelling. CT may also demonstrate thickening of trabeculae and medullary abnormalities. In chronic osteomyelitis CT is better than MRI for the demonstration of cortical destruction and demonstrating the presence of gas (Fig. 53-8). CT is also superior to MRI in the demonstration of sequestra (Fig. 53-9), involucra and cloacae and can guide therapeutic options.33 Soft-tissue abnormalities can be seen with CT, but MRI is superior for demonstrating these (Fig. 53-10).34 In the spine, CT is much more sensitive in demonstrating trabecular destruction and end-plate erosions than conventional radiography. Paravertebral abscesses may be demonstrated clearly with CT. Vertebral disc space narrowing is not reliably detected on axial images and requires sagittal reconstructions. Spinal canal stenosis and associated fractures of bones can also be clearly demonstrated.35 In the absence of trauma, the presence of fat/fluid levels in the soft tissues around the bone, especially when associated with spongy bone destruction is an important and specific sign of underlying osteomyelitis.29 Periprosthetic infection may be demonstrated by CT. Artefacts due to beam hardening, from high density metallic prosthetic components can be minimised by using an extended CT number scale, a high kVp, acquiring data in thin sections then generating thicker section maximum intensity projection reformations and the use of iterative image reconstruction software designed to suppress metal artefacts. MRI has high accuracy and can be positive as early as 3–5 days after the onset of infection. The good soft-tissue contrast, high diagnostic accuracy and wide availability of MR imaging makes this the investigation of choice in suspected osteomyelitis. T1- and T2-weighted (T2W) spin-echo (SE) sequences should be obtained in at least two planes: axial and coronal or sagittal. A short tau inversion recovery (STIR) sequence or fat-suppressed T2 sequence is useful to identify the bone marrow oedema and soft-tissue oedema easily. Usual slice thickness is 3–4 mm (Fig. 53-11).36 Fat-suppressed images can identify ulceration, abscess formation and sinus tracts due to the accentuated fluid signal against a background of suppressed soft-tissue and marrow signals. Gadolinium-enhanced T1-weighted SE images with fat saturation help improve diagnostic confidence, although the overall sensitivity and specificity do not change significantly (Fig. 53-12).33 Bone marrow oedema is one of the earliest signs of osteomyelitis. In acute osteomyelitis there is increase in intramedullary water due to oedema, inflammation and ischaemia, resulting in areas returning low T1 signal and increased T2 signal; this is even better appreciated on fat-saturated or STIR images. The marrow oedema is usually ill defined in its early stages. Later on with more localised bone destruction the oedema and signal changes appear well defined.36 Bone marrow oedema is more extensive in osteomyelitis than in degenerative or infective arthritis. Cortical disruption may lead to the development of periosteal reaction. Cortical disruption is seen as a break in the normal low signal of the cortical bone. Periostitis shows as thin linear pattern of oedema with enhancement, surrounding the outer cortical margin. Chronic periostitis and periosteal reaction are seen as thickening of low signal of cortical bone in both T1- and T2-weighted images. In subacute osteomyelitis, an intramedullary abscess (Brodie’s abscess) may be seen. The central fluid component has low-to-intermediate T1 signal and hyperintense T2 signal, surrounded by a sclerotic rim which has low T1 and T2 signal (Fig. 53-13). The MR characteristics of a sequestrum are similar to the bone it is derived from. If it is from cortical bone, it has low signal, with a higher signal if derived from cancellous bone. The exudate in the presence of active infection tends to show a low T1 signal and high T2 signal, which may show enhancement, which is seen to surround the central sequestrum. The involucrum has the signal of normal living bone, but is commonly thickened and sclerotic and may show oedema. A cloaca is seen as a high signal defect in cortical bone at the edge of a cavity. Collections of pus may be seen extending from the cloaca to the subcutaneous tissue (Fig. 53-14).36 Soft-tissue oedema is demonstrated as low T1 signal on the background of high signal of the subcutaneous fat and has hyperintense signal compared to normal fat on T2 images. Fat-saturated proton density-weighted images and STIR images can demonstrate the soft-tissue changes more clearly.37 MR imaging can be useful in differentiating between acute osteomyelitis and acute bone infarction, especially after intravenous gadolinium contrast agents. Those with osteomyelitis showed a thick, irregular peripheral enhancement around a non-enhancing centre. Medullary infarctions show thin, linear rim enhancement or a long segment of serpiginous central medullary enhancement.38 Metal artefact suppression MRI techniques are useful for imaging close to prostheses. These include avoidance of gradient-echo sequences, use of STIR rather than fat suppression, acquiring the images on a high image matrix with a wide bandwidth and repeating sequences with swapped phase and frequency. Three-phase skeletal scintigraphy is generally useful in the diagnosis of osteomyelitis. However, in the presence of previous trauma, metal devices, neuropathic joints and pre-existing bone conditions, this becomes less reliable and indium and gallium studies play a role. The limiting factor in these investigations is the need for a second investigation such as MRI to confirm the diagnosis due to poor specificity and spatial resolution (Fig. 53-15).
Bone, Joint and Spinal Infection
Introduction
Epidemiology
Classification
Paediatric Musculoskeletal Infections
Pathophysiology
Clinical Features
Investigations and Management
Plain Radiographs
Ultrasound
Computed Tomography
Magnetic Resonance Imaging
Nuclear Medicine
Chronic Recurrent Multifocal Osteomyelitis (CRMO)
SAPHO Syndrome
Sclerosing Osteomyelitis of Garré
Necrotising Fasciitis
Adult Musculoskeletal Infections
Pathogenesis
Clinical Features
Investigations and Management
Plain Radiographs
Ultrasound
Computed Tomography
Magnetic Resonance Imaging
Nuclear Medicine

Bone, Joint and Spinal Infection
Chapter 53