Tibial and Fibular Shafts
Trauma
Fractures of the tibial and fibular shafts are among the most common long bone fractures in adults (average age 37), teenage males (15% of all fractures), and comprise 4% to 5% of all childhood fractures. Fibular fractures are usually associated with tibial fractures (see Fig. 7-1). Therefore, the focus will be on tibial injuries. The distal two thirds of the tibia is most often involved. Also, the lower leg is the most common site of combined osseous and soft tissue injury. The relatively exposed subcutaneous location of the tibia makes it vulnerable to direct high-velocity injury such as motor vehicle accidents or gunshot wounds. Direct trauma usually results in transverse, segmental, or comminuted fracture of the tibia with associated fibular fractures. Indirect trauma generally results in oblique or spiral fractures (see Fig. 7-2). Overuse injuries may also result in stress fractures of the tibia and fibula. Fractures should be described by precise anatomic location, pattern of the fracture line, position of the fragments, degree of comminution, and whether they are open or closed.
Suggested Reading
Court-Brown CM, McBirnie J. The epidemiology of tibial fractures. J Bone Joint Surg. 1995;77B:417–421.
Classification
Treatment of tibial shaft fractures includes closed and open approaches. Treatment choice is based on the type of fracture, whether open or closed, patient status, and surgical preference. There are multiple classification systems designed to assist with treatment and prognosis. Gustilo and Anderson’s classification is specifically designed for open wounds, a common feature of tibial shaft fractures.
Orthopaedic Trauma Association classification
Type A: Simple fractures
Type B: Wedge fractures (see Fig. 7-4)
B1—spiral wedge fractures
B2—intact bending wedge fractures
B3—comminuted wedge fractures
Type C: Complex fractures (see Fig. 7-5)
C1—spiral complex fractures
C2—segmental complex fractures
Gustilo and Anderson classification
Type I: Wound clean and <1 cm
Type II: Wound larger than 1 cm without extensive soft tissue damage
Type IIIA: Extensive soft tissue wound (≥10 cm), periosteum intact
Type IIIB: Periosteal stripping requiring flap coverage
Type IIIC: Above plus vascular injury requiring vessel repair (see Fig. 7-6)
 Fig. 7-1 A: Isolated fibular fracture (arrow) due to a direct blow. Cast immobilization. Anteroposterior (AP) (B) and lateral (C) radiographs at 6 weeks demonstrate organizing callus formation. |
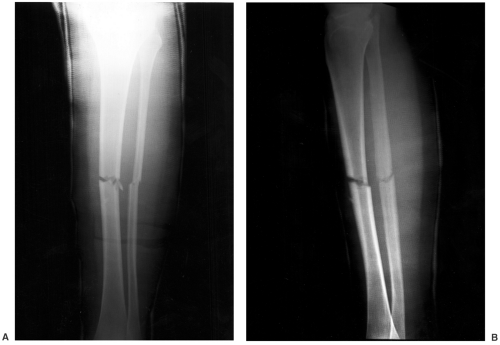 Fig. 7-3 Anteroposterior (AP) (A) and lateral (B) radiographs of minimally displaced transverse fractures of the mid tibia and fibula with cast immobilization. |
 Fig. 7-4 Anteroposterior (AP) radiograph demonstrating a wedge (butterfly fragment) fracture (arrow) of the proximal tibia with adjacent comminuted fibular fracture. |
Suggested Reading
Gustilo RB, Anderson JT. Prevention of infection in treatment of 1025 open fractures of the long bones. J Bone Joint Surg. 1976;58A:453–458.
Lenehan B, Fleming P, Walsh S, et al. Tibial-shaft fractures in amateur footballers. Br J Sports Med. 2003;37:176–178.
Muller ME, Nazarin D, Koch P, et al. Comprehensive classification of fracture of the long bones. Springer-Verlag: Berlin;1990.
Okike K, Bhattacharyya T. Trends in management of open fractures. J Bone Joint Surg. 2006;88A:2739–2748.
Imaging Techniques
Imaging of tibial and fibular shaft injuries can be accomplished with anteroposterior (AP) and lateral radiographs for complete fractures (Figs. 7-1, 7-2, 7-3, 7-4, 7-5). Knee and ankle should be included. Subtle stress injuries or undisplaced fractures may be more easily assessed with magnetic resonance imaging (MRI). Radionuclide scans can also be useful for detection of subtle fractures. However, magnetic resonance (MR) features are typically more specific. Angiography may be required in patients with advanced soft tissue injury who may require vascular repair (Gustilo and Anderson IIIC) (Fig. 7-6).
Suggested Reading
Bender CE, Campbell DC, Berquist TH. The tibia, fibula and calf. In: Berquist TH, ed. Imaging of orthopaedic trauma, 2nd ed. New York: Raven Press; 1992:433–454.
Mashru RP, Herman MJ, Pizzutillo PD. Tibia shaft fractures in children and adolescents. J Am Acad Orthop Surg. 2005;13:345–352.
Tervonen O, Junila J, Ojala R. MR imaging of tibial-shaft fractures. A potential method for early visualization of delayed union. Acta Radiol. 1999;40:410–414.
Treatment Options
Goals for management of tibial fractures include maintaining length, restoring normal weight-bearing alignment, and preservation of soft tissues. Alignment and rotation should be corrected to near anatomic position. The ankle and knee joints must be parallel. There should be no >5 degrees of varus or valgus angulation, 10 degrees of anterior or posterior angulation, 10 degrees of rotation, and 1 cm or less of leg length discrepancy (see Fig. 7-7). In children younger than 8 years, apposition is less critical. In older children, at least 50% apposition should be achieved (see Fig. 7-8). Treatment options include closed reduction with cast or brace immobilization, external fixation, intramedullary nailing, and open reduction with plate and screw fixation.
Closed Reduction with Cast or Brace Immobilization
Initially, all tibial fractures should be treated with a long posterior splint with the knee in flexion and the ankle in neutral position. Compartment syndrome is a concern and should be monitored. Stable undisplaced fractures can be treated with cast immobilization in 3 to 5 days after initial swelling has decreased (Fig. 7-8). There are several cast approaches including long leg casts with slight knee flexion and patellar-tendon bearing (PTB) casts (see Fig. 7-9). In either situation, early weight bearing is important. In adolescents long leg cast immobilization for 6 weeks is followed by progressive weight bearing in a PTB cast for an additional 4 to 6 weeks. A brace can also be used after several weeks of cast immobilization to increase joint motion and facilitate weight bearing. Serial radiographs are important to assure fracture stability. Callus begins to form at approximately 6 to 8 weeks following the injury.
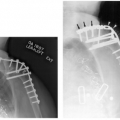
External Fixation
External fixation approaches are commonly used with tibial shaft fractures due to the relatively high frequency of open fractures with varying degrees of soft tissue injury. Fixation is easily applied and allows adjustability of fragments and access to soft tissue wounds (see Fig. 7-10). Pin or wire placement is accomplished to avoid critical anatomic structures such as neurovascular areas (see Fig. 7-11).
Indications for external fixation
Open fractures with soft tissue injuries (see Fig. 7-12)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree