10 Prominent Perivascular Space
10.1 Case Presentation
10.1.1 History and Physical Examination
A 40-year-old man with no major past medical history complains of headache following a minor head trauma.
The patient is alert and oriented and his cranial nerves II–XII are grossly intact.
10.1.2 Imaging Findings and Impression
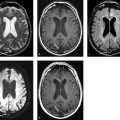
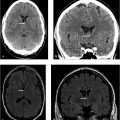
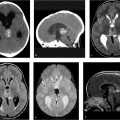
Brain MR images including axial T2-weighted (white arrow in ▶ Fig. 10.1a), axial noncontrast T1-weighted (white arrow in ▶ Fig. 10.1b), and fluid-attenuated inversion recovery (FLAIR; black arrow in ▶ Fig. 10.1c) demonstrate a small fluid-filled cystlike lesion measuring 3 × 6 mm involving the left thalamus. It follows cerebrospinal fluid (CSF) signal intensity on all the sequences. Axial diffusion-weighted image (▶ Fig. 10.1d) and apparent diffusion coefficient (ADC) map (▶ Fig. 10.1e) show no restriction. The fluid-filled lesion is nonenhancing on the axial postcontrast T1-weighted image (▶ Fig. 10.1f), consistent with a prominent perivascular space (PVS).

10.2 Differential Diagnosis
Prominent PVS:
It represents enlarged PVSs that follow cerebrospinal fluid (CSF) signal intensity on all MRI sequences.
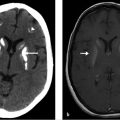
Neurocysticercosis:
May mimic a PVS in the initial vesicular stage. Endemic area and additional lesions in regions of the brain that are atypical for PVSs is helpful. Additional calcified lesions, representing the nodular calcified stage of neurocysticercosis, are helpful in making this diagnosis.
A “dot sign” may be seen inside the cyst, representing the parasite scolex.
Cryptococcosis:
It spreads along the PVSs and becomes distended with mucoid, gelatinous material.
When multiple, they should be differentiated from prominent PVSs.
If the patient is immunocompromised, cryptococcus should be considered highly in the differential diagnosis!
Cryptococcomas can manifest with low signal intensity on T1-weighted images, high signal intensity on T2-weighted images and fluid-attenuated inversion recovery (FLAIR) images, and variable enhancement on postcontrast images.
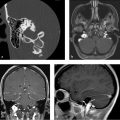
Arachnoid cyst:
CSF-containing cysts that are most commonly found in the middle cranial fossa, the parasellar region, and the subarachnoid space over the convexities.
It follows CSF signal intensity on all sequences.
Lacunar infarctions:
They show abnormal increased FLAIR signal intensity along the rim and more commonly happen in the upper two-thirds of the basal ganglia.
Acute lacunar infarcts show restricted diffusion.
Cystic neoplasm:
They have solid components, may enhance, and commonly show surrounding edema.
Diffusion-weighted images and the FLAIR sequence should be evaluated for better differentiating cystic neoplasms from prominent PVSs.
Dysembryoplastic neuroepithelial tumor (DNET) and multinodular and vacuolating neuronal tumor (MVNT):
These are similar-appearing cystic bubbly lesions most frequently located in the temporal lobe.
DNETs are cortical lesions, while MVNTs are subcortical in location.
MVNT is a recently introduced entity in WHO 2016 classification.
The cystic component does not suppress completely on the FLAIR sequence and often has a hyperintense rim.
Lack of enhancement is most common.
Non-neoplastic neuroepithelial cyst:
It is spherical to ovoid and measures up to several centimeters.
It may involve the lateral ventricles or the fourth ventricle with which they do not communicate.
CSF-like signal on MR images with no enhancement on postcontrast images. 1
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree