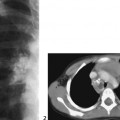
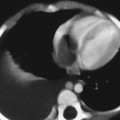
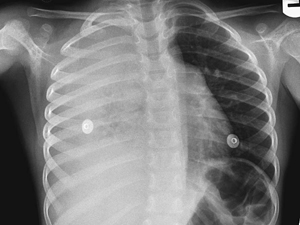
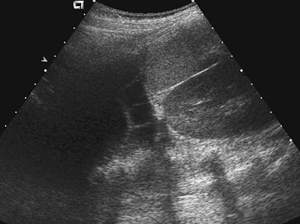
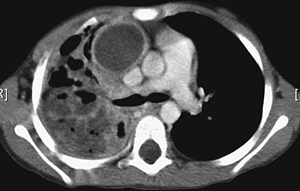
CASE 105 A 4-year-old female presents with high fever, cough, increased respiratory rate, bronchial breathing, and decreased breath sounds on the right side. Her pediatrician had treated her with antibiotics. She continued to deteriorate, and after a chest radiograph was performed she was referred to a pediatric tertiary care center. After admission she was further imaged with CT and ultrasonography. What interventional procedure should be performed? Figure 105A Figure 105B Figure 105C The chest radiograph demonstrates complete opacification of the right hemithorax (Fig. 105A). Ultrasound shows a complex collection (Fig. 105B), whereas CT provides evidence of empyema with underlying lung inflammation, abscess, and likely necrosis. In addition, there is a medial enhancing fluid collection that represents either a medial loculated empyema or a mediastinal abscess (Fig. 105C). Necrotizing or aggressive pneumonia with empyema, and possible mediastinal abscess requiring chest tube placement Chest tubes (or thoracostomy tubes) are placed in the pleura space for the drainage of air and/or fluids in the thoracic region. Chest drainage techniques have been used since the early 1900s for the treatment of postpneumonic empyema. In recent years, the traditional technique has been replaced by an image-guided technique and adjunctive intracavitary fibrinolytic therapy. The image-guided technique has the potential of reducing many of the complications associated with a “blind” placement technique, including accidental damage to the internal thoracic arteries. Chest drainage is used in situations where a loss of pleural negative pressure is noted. This may have the following causes: Clinical findings are usually related to the underlying pathology. Some common symptoms may include:
Clinical Presentation
Radiologic Findings
Diagnosis
Discussion
Background
Etiology/Indications for Drainage
Clinical Findings
Complications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree