
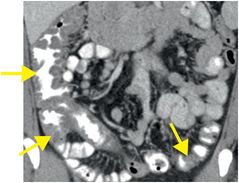
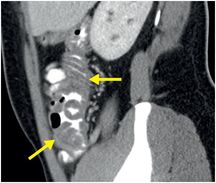
Diagnosis: Crohn’s disease (acute flare)
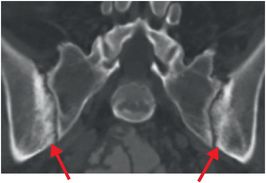
Coronal (left image) and sagittal (middle image) CT images with oral and intravenous contrast show a long segment of mural thickening (yellow arrows) involving the distal ileum, cecum, and ascending colon, associated with subtle pericolonic fat stranding, representing ileocolitis. Coronal CT in bone window (right image) of the same patient demonstrates symmetrical sclerosis at the iliac aspect of the sacroiliac joints (red arrows), consistent with sacroiliitis.
Discussion
Overview of Crohn’s disease
Crohn’s disease is a chronic, relapsing granulomatous inflammatory disorder affecting the gastrointestinal tract. Many cases of Crohn’s disease are first diagnosed during the workup for acute right lower quadrant pain in the Emergency Department.
Crohn’s disease can involve any segment of the gastrointestinal tract, from the oral mucosa to the anus. The terminal ileum is almost always involved. The involved portions of bowel are characteristically discontinuous in location (e.g., there may be simultaneous involvement of the terminal ileum and anus without any abnormality of intervening bowel segments, a distribution described as “skip lesions”). The affected bowel features ulcerations, full-thickness mural inflammation, and formation of noncaseating granulomas.
Crohn’s disease is most commonly diagnosed in adolescence through the third decade, although onset in late adulthood has also been reported. Patients usually present with chronic diarrhea, abdominal pain, weight loss, and fever.
Skip lesions and transmural involvement are characteristic of Crohn’s disease. In contrast, ulcerative colitis (UC) tends to feature continuous, superficial (mucosal) inflammation. The rectum is almost always involved in UC, with extension proximally.
Imaging of Crohn’s disease
CT is the primary imaging modality for the evaluation of acute right lower quadrant pain due to quick examination time with single-breath-hold scanning and near-universal availability.
Mesenteric hyperemia leads to many of the CT findings of Crohn’s disease. Transversely oriented engorged vessels perpendicular to the longitudinal axis of the involved bowel loop produce the characteristic “comb” sign. Intramural fat and mesenteric fibro-fatty infiltration (called “creeping fat” by pathologists) are indicative of chronic involvement.
The most common cross-sectional imaging findings during an acute flare include:
Wall thickening (>4 mm)
Mesenteric vascular engorgement, submucosal and mesenteric edema, and mucosal hyperenhancement
Transmural ulceration and fistula formation
Enlarged mesenteric lymph nodes
MR enterography is a highly accurate, dynamic imaging technique that spares the generally young population of patients with inflammatory bowel disease from ionizing radiation exposure.
Abdominal complications and management of Crohn’s disease
There is a high incidence of abdominal complications of Crohn’s disease, including bowel stricture, fistula (to other bowel segments, urinary bladder, skin, or perianal tissue), and abscess.
Differentiation between an acute flare and chronic stenosis is critical, since management differs substantially. An acute flare is usually treated with anti-inflammatory drugs, while a chronic stenosis may require surgery. The absence of acute inflammatory changes and the presence of fibrotic stenoses suggests chronic disease.
Extra-intestinal manifestation of Crohn’s disease
Extra-intestinal inflammatory processes are seen in up to 25% of patients with Crohn’s disease and may involve the musculoskeletal, ocular, and mucocutaneous systems. Musculoskeletal involvement includes an inflammatory arthropathy, which characteristically affects the sacroiliac joints (as shown in this case), although any joint may be involved. Ocular manifestations include uveitis. Mucocutaneous findings include erythema nodosum and pyoderma gangrenosum involving the lower extremities, and aphthous ulcers involving the mucous membranes.
Clinical synopsis
This patient underwent colonoscopy with biopsy revealing a granulomatous inflammatory process, consistent with Crohn’s disease. Appropriate medical treatment was started.
Self-assessment
|
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








