12 Diffuse White Matter Hyperintensities
12.1 Introduction
Diffuse white matter hyperintensities on brain MRIs are a common finding with an extensive differential diagnosis. In this chapter, we describe a case in which a diagnosis of CNS demyelination was highly suggested based on the appearance of white matter lesions identified on MRI. The necessary imaging, clinical evaluation, and laboratory testing that led to a diagnosis of radiologically isolated syndrome (RIS) are outlined. In addition, companion cases of diffuse white matter signal abnormalities secondary to small vessel ischemic disease are presented to highlight key differences in imaging appearance and clinical presentation between these conditions. The differential diagnosis of diffuse white matter hyperintensities and imaging “red flags” that should suggest a diagnosis other than CNS demyelination are also discussed.
12.2 Case Presentation
12.2.1 History
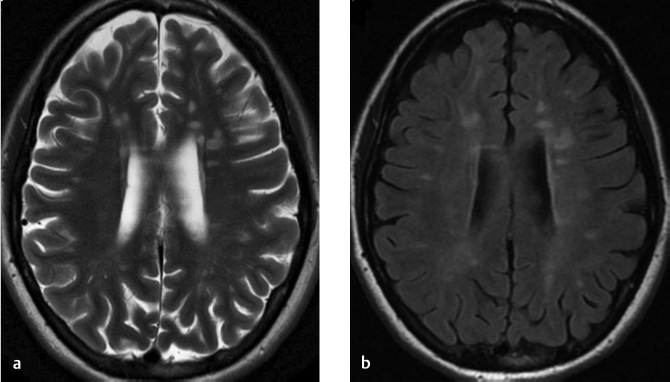
A 26-year-old woman who presents to the hospital for evaluation of syncope and collapse. A brain MR was performed. ▶ Fig. 12.1 shows the axial T2-weighted images (T2WIs; a) and axial fluid-attenuated inversion recovery (FLAIR) image (b).
12.3 Imaging Analysis
12.3.1 Imaging Findings and impression
▶ Fig. 12.2a,b shows large, discrete ovoid lesions that are hyperintense on T2WIs and FLAIR (arrows) MRI sequences. Many of these lesions measure greater than 6 mm in diameter and are located adjacent to the ventricles, and involve the deep white matter. The orientation of many lesions is perpendicular to the lateral ventricles (arrows in ▶ Fig. 12.2b,d). ▶ Fig. 12.2c shows infratentorial lesions, which are also hyperintense on T2WIs (arrow indicating largest infratentorial lesion). ▶ Fig. 12.2d shows the lesions are hypointense on T1WIs with the “Dawson’s fingers” appearance (white arrows).

The multifocal periventricular and posterior fossa white matter lesions have an appearance typical of demyelinating disease. (See Section 12.5, “Differential Diagnosis of White Matter Lesions.”)
12.3.2 Additional Imaging Recommended
Postcontrast MRI of the brain should be obtained if gadolinium was not administered for the initial brain MRI. Ideally, a high-quality MRI at 1.5 or 3T should be obtained.
MRI of the cervical spine is recommended with and without gadolinium given the suspicious nature of the brain MR findings. Although the vast majority of cervical spinal cord lesions would not be clinically “silent,” if present, they would impact management decisions and provide additional prognostic information in patients with multiple sclerosis.
12.4 Clinical Evaluation
12.4.1 Neurologist History and Physical Examination
The patient is a 26-year-old, right-handed, Caucasian woman with a history of type 1 diabetes mellitus, depression, and anxiety with anxiety who presented to the hospital after a possible “syncopal” episode that occurred while she was having an argument with a family member. She denied any prior symptoms other than the single fainting episode.
A complete neurological examination was performed. The patient was awake, alert, and oriented. Her speech was fluent and she answered all questions appropriately. Visual acuity was 20/20 bilaterally as tested by the Snellen chart with intact peripheral visual fields. Her face was symmetric bilaterally with intact facial expressions. Facial sensation was intact to light touch, pinprick, and temperature. Her tongue was midline and palate elevated equally bilaterally. A motor examination was normal in both proximal and distal upper and lower extremities. Sensation was intact in all extremities to light touch, pinprick, temperature, position, and vibration. Deep tendon reflexes were normal in all extremities and no pathologic reflexes were elicited. Gait and station were normal with full arm swing. Finger-to-nose and heel-to-shin tests were also normal bilaterally.
12.4.2 Recommended Additional Testing
MRI of the brain should be of high quality, preferably 1.5 or 3 T (see (Magnetic Resonance Imaging in multiple sclerosis [MAGNIMS] protocol).
MRI of the cervical spine with and without gadolinium.
Peripheral blood/serum studies: complete blood cell count (CBC), erythrocyte sedimentation rate (ESR), antinuclear antibody (ANA), rheumatoid factor, vitamin B12, homocysteine, methylmalonic acid, antiphospholipid antibody, thyroid function tests, angiotensin-converting enzyme (ACE), anticardiolipin antibody screen and Lyme disease antibody titers. 2
Routine cerebrospinal fluid (CSF) analysis should be performed to exclude other diagnoses—particularly infection. 1
Visual evoked potential (VEP) testing can also be obtained to look for signs of subclinical demyelination. 1
12.4.3 2015 MAGNIMS Standardized Brain and Spine MRI Protocol
Brain:
Mandatory:
Axial: proton-density and/or T2 FLAIR/T2-weighted.
Sagittal: 2D or 3D T2 FLAIR.
2D or 3D contrast-enhanced T1-weighted imaging.
Optional:
Unenhanced 2D or high-resolution isotropic 3D T1-weighted imaging.
2D and/or 3D dual inversion recovery.
Axial diffusion-weighted imaging.
Spinal cord:
Mandatory
Dual echo (proton density and T2 weighted) conventional and/or fast spin echo (FSE).
Short tau inversion recovery (STIR; as an alternative to proton-density-weighted images).
Contrast-enhanced T1-weighted spin echo (if lesions that are hyperintense on T2-weighted imaging are present).
Optional:
Phase-sensitive inversion recovery (as an alternative to STIR at the cervical segment).
12.4.4 Results of Additional Testing
Cerebrospinal fluid (CSF) studies showed an immunoglobulin index of 1.0 (normal < 0.7) and three oligoclonal bands (OCBs) that were not observed in the serum. All other serum labs were unremarkable. Additional testing performed in this patient included VEP and optical coherence tomography (OCT), both of which were normal.
The cervical spine MR failed to reveal any additional lesions.
There were no enhancing lesions in the brain or in the cervical spine.
12.4.5 Clinical Impression
Radiologically isolated syndrome (RIS).
12.4.6 Management Decision in This Case
VEPs can be performed on a case-by-case basis as they can add an additional risk factor for progression to symptomatic MS when positive. In this case, they would have offered information about prior optic nerve inflammation had they been positive.
There is currently no consensus as to routine use of disease-modifying therapies (DMTs) in patients presenting with RIS, even for those with abnormal cervical and/or thoracic spinal cord findings. A randomized clinical trial to determine the utility of early intervention in RIS patients is currently in progress.
In this case, a decision was made to pursue active monitoring with periodical clinical and radiological follow-up every 6 to 12 months.
12.5 Differential Diagnosis of White Matter Lesions
Inflammatory:
Multiple sclerosis (MS), radiologically isolated syndrome (RIS), vasculitis (systemic lupus erythematosus [SLE], Sjögren’s syndrome, Behçet’s syndrome, primary CNS vasculitis), neurosarcoidosis.
Hypoxic/ischemic:
Atherosclerosis, stroke, hypertension, migraine, amyloid angiopathy, vasculopathy (CADASIL, Susac’s syndrome).
Infectious:
HIV, syphilis, Lyme disease, TB, progressive multifocal leukoencephalopathy (PML).
Toxic/metabolic.
Traumatic:
Posttraumatic, radiotherapy.
Metabolic:
Leukodystrophies.
Neoplastic:
Metastatic or primary disease.
Normal:
Age-related or Virchow–Robin spaces.
12.6 Diagnostic Imaging Pearls
Imaging findings suggestive of a demyelinating process 1 :
Lesion size: usually greater than 5 mm.
Asymmetric.
Location: cortical/juxtacortical, periventricular (Dawson’s fingers), infratentorial, spinal cord, corpus callosum.
Gadolinium-enhancing lesions (incomplete rim enhancement in larger lesions).
Most typically, all lesions do NOT enhance simultaneously at onset.
“Central vein sign.” 1
New lesions on repeat imaging are common with possible regression of older lesions.
Nonconfluent except in very advanced cases.
12.7 Clinical and Diagnostic Imaging Pitfalls
“Red flag” clinical and imaging findings that are atypical for MS (RIS) and should suggest an alternative diagnosis (see ▶ Table 12.1).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree