15 Cerebral Cavernous Malformations
15.1 Introduction
Cerebral cavernous malformations (CCMs) are vascular anomalies known as the “popcorn” lesions in the brain. Symptomatic hemorrhage resulting from these lesions is the main reason for imaging and treating them. The epidemiology, natural history, imaging workup, and approach to management of CCMS are addressed.
15.2 Case Presentation
A 30-year-old Hispanic woman sought consult to a primary care provider for headaches. On examination, the patient was neurologically intact without focal deficits. She was referred to our outpatient facility for imaging evaluation.
15.3 Imaging Analysis
15.3.1 Imaging Findings
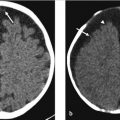
Noncontrast head CT shows a focal area of increased attenuation in the right occipital lobe without surrounding edema (arrow in ▶ Fig. 15.1).

An area of increased attenuation within the brain on CT scan may be due to calcification, an acute hemorrhage, or dense, hypercellular tumor. The lack of surrounding edema makes the possibility of acute hemorrhage unlikely. Therefore, an MRI was recommended for further evaluation.
15.3.2 Additional Imaging
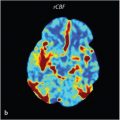
A brain MRI was performed for further evaluation (see ▶ Fig. 15.2).

15.3.3 Imaging Findings
The brain MRI axial T1-weighted image (▶ Fig. 15.2a) demonstrates a mixed signal intensity (SI) lesion with areas of hyperintensity and hypointensity/isointensity relative to the brain parenchyma. The T2-weighted image (▶ Fig. 15.2b) reveals a predominantly hyperintense lesion resembling a “popcorn” ball or mulberry. There is a halo of hypointensity reflecting hemosiderin staining. However, there is no surrounding edema. The GRE sequence (▶ Fig. 15.2c) depicts signal dropout of the lesion. These findings correspond to the localized area of increased attenuation on the reference CT.
15.3.4 Impression
Typical appearing cavernous hemangioma in the right occipital lobe. There is no surrounding edema, to suggest recent or acute hemorrhage.
15.4 Differential Diagnosis
Cavernous malformation (CM)—Classic “popcorn” appearing, round lesion with dark hemosiderin rim on T2-weighted images that “blooms” on GRE sequences. Often a vague surrounding area of T1 shortening (bright signal) in the brain parenchyma may suggest bleeding that originated from an acutely hemorrhagic CM.
Microhemorrhage associated with shear injury as seen in diffuse axonal injury (DAI)—Clinical history of trauma with severely compromised neurological examination out of proportion to imaging findings. Typical locations include the gray–white matter junction, dorsal brainstem, and corpus callosum. Associated edema is frequent (see Companion Cases 1 and 2: Diffuse Axonal Injury; ▶ Fig. 15.3 and ▶ Fig. 15.4).
Amyloid angiopathy associated microhemorrhages (see Companion Case 3: Amyloid Angiopathy; ▶ Fig. 15.5).
Hemorrhagic metastatic disease—surrounding edema and multifocal lesions without hemosiderin rim (see Companion Case 4: Hemorrhagic Metastatic Disease; ▶ Fig. 15.6).
Arteriovenous malformation (AVM)—Hemorrhage in association with prominent vascular flow voids should prompt consideration of this entity and CTA, MRI/MRA, or DSA performed. This typically lacks hemosiderin rim.
15.5 Diagnostic Imaging Pearls
“Popcorn” ball (or mulberry) describes the classic appearance of a CM (▶ Fig. 15.2b and ▶ Fig. 15.7, and ▶ Table 15.1)—a well-circumscribed mixed density/SI mass surrounded by hemosiderin rim. 1
On T2-weighted MRI, the combination of a reticulated core of mixed SI with a surrounding rim of decreased SI strongly suggests the diagnosis of a CM (▶ Fig. 15.2b and ▶ Fig. 15.7, and ▶ Table 15.1). Smaller lesions appear as areas of decreased SI (black dots; ▶ Table 15.1). 2
CMs are frequently associated with developmental venous anomalies (DVAs). 3 , 4 , 5 , 6 , 7
15.6 Clinical Evaluation and Management
15.6.1 Neurosurgical Evaluation
The patient was neurologically intact. The causal relationship of the lesion to the patient’s symptoms (i.e., headaches) was not established given its size, location, and lack of evidence for recent bleeding. Conservative management was elected in this case. Repeat imaging may be performed should the patient develop new neurological symptoms suggesting that CCM has bled. Follow-up imaging may be also considered to reassure the patient about the stability of the lesion.
15.6.2 Essential Diagnostic Imaging Information Regarding Cavernous Malformations
MRI is particularly sensitive in detecting CMs and is highly specific. 8 , 9 It is recommended that every symptomatic venous malformation be worked up with a high field strength MR unit. 2 , 10
T2-weighted gradient-echo sequences have been shown to be more sensitive than conventional sequences. 10 More advanced imaging techniques such as high-field and susceptibility-weighted MR imaging have been employed for evaluation of CCMs. 10
GRE MRI is a key method for diagnosis of CCMs due to its ability to display hemosiderin-filled brain tissue with a very distinct hypointensity. GRE MRI not only is more capable of identifying all lesions present, but also delineates them more precisely 11 (see ▶ Table 15.1).
GRE MRI may show multifocal lesions in elderly patients with hypertension and a history of stroke; however, they must not be mistaken for familial CCMs. They result from hypertensive angiopathy and are located in periventricular areas. 10
Susceptibility-weighted imaging (SWI) is very advantageous for detecting CM lesions because it accurately recognizes deoxyhemoglobin and hemosiderin. It is also considered the only method capable of detecting unbled CM lesions. 10 Studies indicate that SWI is more sensitive than GRE in the evaluation of CCMs. 10 , 12 , 13 , 14 This is particularly true in the familial form of the disease where many lesions shown on SWI were not detected on GRE. 10 , 13 , 15 It was proposed that the CCMs identified only on SWI and undetectable on GRE be added as a new type (type V) in the Zabramski classification. 16
Diffusion tensor imaging (DTI) and functional MR imaging have been applied to the preoperative and intraoperative management of these lesions. 10 The Zabramski classification system characterizes the varied appearances of CCMs on MRI (▶ Table 15.1), 17 and can help predict the hemorrhage rates of CCMs 18 :
CCMs with acute or subacute blood degradation products have the highest hemorrhage risk (Zabramski types I and II)—23.4%. 18
CCMs without acute or subacute blood degradation products have an intermediate risk of hemorrhage (Zabramski type III)—3.4%. 18
Dot-sized lesions have the lowest hemorrhage rate (Zabramski type IV)—1.3%. 18
A simple tripartite classification might be more useful in clinical practice. 18
15.7 Companion Cases
15.7.1 Companion Cases 1 and 2: Diffuse Axonal Injury


15.7.2 Companion Case 3: Amyloid Angiopathy

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree