13 Brain Capillary Telangiectasias
13.1 Introduction
Brain capillary telangiectasias (BCTs) are rare findings often found incidentally on imaging workup of unrelated symptoms. Because of their benign nature, it is important not to mistake BCTs from more serious conditions (such as neoplasm, demyelination, or infarct) that have worse prognoses. Familiarity with the imaging findings of BCTs is crucial, not only to avoid unwarranted and potentially hazardous biopsies, but also to allay patient’s fears and concerns arising from a “wrong diagnosis.” The epidemiology, pathology, characteristic imaging features, and pertinent clinical issues, including the management of BCTs, are discussed.
13.2 Case Presentation
An otherwise healthy 56-year-old man was referred to our outpatient imaging facility for behavioral changes. The patient had no other symptoms or neurologic complaints. On examination, he was neurologically intact.
13.3 Imaging Analysis
13.3.1 Imaging Findings
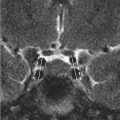
Axial T1 precontrast MRI (▶ Fig. 13.1a) showed no abnormality. Axial T1 postcontrast study revealed an enhancing lesion in the left paramedian pons. The lesion shows brush-like or stippled pattern of enhancement. The brain MRI examination is otherwise unremarkable.

Impression: The imaging findings are consistent with capillary telangiectasia. This is an incidental finding and the patient’s history and clinical presentation are noncontributory.
13.4 Clinical Evaluation and Management
No follow-up imaging is recommended for an asymptomatic capillary telangiectasia with no evidence of cavernous malformation.
13.5 Differential Diagnosis
Capillary telangiectasia (see Companion Case 5, ▶ Fig. 13.6):
Lack of any abnormality on the precontrast T1-weighted and fast spin-echo (FSE) T2-weighted images is characteristic.
It is most commonly found in the pons, although it may occur in other locations within the brain parenchyma
Gradient recalled echo (GRE) and susceptibility-weighted imaging (SWI) shows low signal.
Enhancement is brushlike or stippled.
Neoplasm (see Companion Case 1, ▶ Fig. 13.2):
Enhancement is almost always more nodular and solid.
Abnormality on the T2-weighted images is frequent but not always present.
Multiple lesions favor metastatic disease.
Subacute infarction (see Companion Case 2, ▶ Fig. 13.3):
It follows a vascular territory and respects the midline.
It restricts on diffusion-weighed imaging (DWI).
It may also show decreased signal on GRE and SWI, but only if hemorrhagic.
It may have patchy enhancement in the subacute phase.
Active demyelination (see Companion Case 3, ▶ Fig. 13.4):
Abnormal signal is present on fluid-attenuated inversion recovery (FLAIR) and T2-weighted images.
Supratentorial callososeptal lesion (Dawson fingers) is usually present if due to multiple sclerosis.
Inflammatory processes, that is, chronic lymphocytic inflammation with pontine perivascular enhancement responsive to steroids (CLIPPERS; see Companion Case 4, ▶ Fig. 13.5):
CLIPPERS is a pontine-centric condition with variable involvement of adjacent structures. 1 Lesions are typically less numerous and smaller as distance from the pons increases. 1
Nodular and curvilinear enhancement “peppering” the pons is the MRI signature of CLIPPERS, 1 which appears different from the “brushlike” enhancement of a capillary telangiectasia.
Patchy, nonspecific T2 signal elevation in the areas of enhancement is seen, 1 whereas no abnormality is evident on the T2-weighted images with capillary telangiectasia.
All patients are symptomatic with cranial sensory abnormalities, diplopia, ataxia, and dysarthria. 1
Behcet’s disease:
This is a chronic, idiopathic, relapsing-remitting, multisystem inflammatory vascular disease characterized mainly by skin lesions and CNS involvement in 20 to 25% of patients 2 (neuro-Behcet’s disease).
Mucocutaneous recurrent oral and genital ulcers, aphthous stomatitis, ophthalmologic lesions such as uveitis and iridocyclitis, and multiple arthralgias are the major clinical features of Behcet’s disease. 2
Brainstem involvement is typical, although any part of the central nervous system may be affected. 2
Typical MRI findings are small circular, linear, crescent-shaped, or irregular T2/FLAIR hyperintensity in the brainstem, usually with minimal mass effect 2 unlike capillary telangiectasia.
Mild to moderate patchy enhancement is common; strong uniform enhancement is rare. 2
13.6 Diagnostic Imaging Pearls
The combination of signal-intensity loss on SWI and focal enhancement in a lesion that is otherwise unremarkable on conventional MR images is virtually diagnostic for BCT 3 (▶ Fig. 13.6).
Classic capillary telangiectasia can be distinguished from cavernous malformation. 4 The latter shows a hypointense hemosiderin ring and marked signal loss (termed “blooming”) on GRE. 4
BCTs are typically small with a stippled or brushlike pattern of enhancement on postcontrast MRI 2 (▶ Fig. 13.1). They lack edema and the hemosiderin halo of cavernous malformations. 2 , 4
BCTs show low signal intensity (susceptibility) on GRE sequence. 5 The presence of susceptibility makes the diagnosis of demyelination, neoplasm, or subacute infarction unlikely 5 (▶ Fig. 13.7).
SWI is a better technique than GRE in the diagnosis of BCT 3 , 6 (▶ Fig. 13.8).
BCTs are angiographically occult. 2 , 7
A small draining vein sometimes associated with BCT 5 may serve as a useful clue to the diagnosis (▶ Fig. 13.8).
13.7 Essential Facts about BCTs
It is important to recognize the MRI features of BCTs in order to avoid unnecessary biopsies, which may be potentially dangerous. 8 The implications of an erroneous diagnosis are profound because of the different prognoses of these other lesions, including their potentially devastating psychological impact to patients and their families. 5
BCTs are typically asymptomatic and incidentally found. 2 , 9 They are considered “leave-me-alone” lesions.
SWI is superior to GRE (▶ Fig. 13.8) 3 , 6 in confirming the diagnosis and differentiating BCT from more serious lesions. This serves to discard serious differential diagnoses with high specificity, reassuring patients and referring physicians. 3
SWI is particularly helpful for BCT in atypical locations and may replace T2*-GRE. 3 SWI is extremely sensitive to susceptibility effects and offers high spatial resolution and excellent contrast. 3
Diffusion-weighted imaging (DWI) may also help differentiate BCTs from other lesions such as infarct. They have a consistently low signal on DWI, contrary to elevated DWI signal for recent infarcts. 10
A draining vein from the lesion is frequently found on postcontrast T1-weighted MRI as an enhancing structure. This may serve as a useful clue to the diagnosis of BCTs. 11
The presence of a small draining vein may also help differentiate BCTs from other lesions. 5 Infarct, neoplasm, or demyelination typically do not harbor such draining vein.
Because they are composed of sacs of stagnant blood that has presumably partially converted to deoxyhemoglobin, they exhibit susceptibility dephasing, which is evident only on GRE (T2*-weighted) images. 5 This dephasing is probably due to the BOLD effect. 5
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree