15 Trauma and Fractures: Pelvis and Lower Extremity
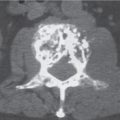
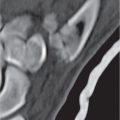
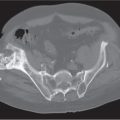
Pelvic fractures must be assessed for both stability and acetabular involvement. Stable pelvic fractures (Fig. 15.34) do not disrupt the osseous ring formed by the pelvis and sacrum (type 1 injuries) or disrupt it in only one place (type 2 injuries), whereas unstable fractures (Fig. 15.35) completely disrupt the ring in two or more places (type 3 injuries). Type 1 injuries include avulsion fractures that occur at tendinous attachment sites, such as the anterosuperior and anteroinferior iliac spines, ischial tuberosity, and iliac crest. These fractures occur commonly in children before closure of the corresponding physis (cartilage plate) and athletes secondary to forcible muscular contraction. Avulsions from the symphysis pubis at the origin of the adductor longus and brevis and the gracilis (“sports hernia”) may be associated with subtle osseous fragments. Another common type 1 injury represents a unilateral pubic ramus fracture (usually in the superior ramus) occurring in elderly patients after a fall or prosthetic hip replacement surgery and in athletes as stress fracture. Isolated transverse or vertical sacral fractures (Fig. 15.36) are rare and have to be differentiated from insufficiency fractures in osteopenia that have usually both a vertical and horizontal course. Type 2 injuries (single break in the pelvic ring) include ipsilateral fractures of the superior and inferior pubic (ischiopubic) rami, fracture of the pubic body adjacent to the symphysis, subluxation of one sacroiliac joint (Fig. 15.37) or the pubic symphysis, and a fracture paralleling the sacroiliac joint (Fig. 15.38). The likelihood of a second break in the pelvic ring (type 3 injury) increases with a greater degree of joint diastasis or fracture displacement at the primary injury site. It should be kept in mind that spontaneous recoil of a separated sacroiliac joint may occur that may result in underestimation of the pelvic injury. Type 3 injuries (double breaks in the pelvic ring) include straddle fractures (vertical fractures of both superior pubic and ischiopubic rami or unilateral vertical rami fractures associated with symphyseal diastasis) (Fig. 15.39) and injuries with complete disruption of both the anterior and posterior pelvic ring (e.g., Malgaigne fracture, bucket handle fracture, and pelvic “dislocation”) (Fig. 15.40). More extensive disruptions of the pelvis result from massive crush injuries in which the osseous ring is completely shattered. In the unstable jumper’s fracture (Fig. 15.41), dissociation of the central portions of the sacrum from its lateral portions occurs by bilateral vertical sacral fractures, most commonly through the neural foramina representing the weakest points in the sacrum. Pelvic fractures are frequently associated with severe soft tissue injuries, including vascular lacerations, compression or disruption of peripheral nerves, and perforation of the urinary bladder, urethra, rectosigmoid, and anus.
Classification systems of pelvic fractures combining the direction of the force that created the injury with the fracture pattern seen radiographically allow a highly specific injury description and are preferred by orthopedic surgeons (Table 15.1). Four underlying mechanisms of injury that produce a distinctive radiographic pattern are discerned by the Young–Burgess classification:
1. Lateral compression (LC): A lateral force vector characteristically causes transverse fractures of the pubic rami, vertical compression fractures of the sacrum, and fractures of the iliac wings, as well as pelvic instability caused by rotation of one or both hemipelvises (rotational instability). In a “wind-swept” pelvis, anterior rotation of the hemipelvis at the side of the impact is associated with posterior rotation of the contralateral hemipelvis.
2. Anteroposterior compression (AC): An anteroposterior or posteroanterior force vector produces vertically oriented pubic rami fractures and disruption of the pubic symphysis and the sacroiliac joints, resulting in pelvic “dislocation” (“sprung” pelvis or “open book” injury).
3. Vertical shear (VC): An inferosuperior force vector produces vertically oriented fractures of the pubic rami and disruption of the sacroiliac joints and sacral or ilial fractures, paralleling this joint. The involved hemipelvis typically is displaced superiorly. Because all ligaments stabilizing the osseous pelvic ring (e.g., iliolumbar, anterior and posterior sacroiliac, and sacrospinous and sacrotuberous ligaments) are affected in this type of injury, the pelvic instability is most severe and both rotationally and vertically unstable. Fracture of the transverse process of L5 where the iliolumbar ligament attaches is a harbinger of an unstable pelvic injury.
4. Combined (complex) mechanism: Two or more different force vectors have been delivered to the pelvis. Lateral compression and vertical shear are the most common combination.

AIIS | anteroinferior iliac spine |
AR | acetabular roof |
ASIS | anterosuperior iliac spine |
AW | anterior acetabular wall |
I | ilium |
IS | ischium |
ISP | ischial spine |
IST | ischial tuberosity |
PIS | posteroinferior iliac spine |
PW | posterior acetabular wall |
QL | quadrilateral lamina |
Dark shaded area | anterior column |
Light shaded area | posterior column |

Pelvic fractures may extend into the acetabulum, where the dome (acetabular roof), the anterior (iliopubic) wall and column, the quadrilateral lamina (surface), or the posterior (ilioischial) wall and column may be involved (Fig. 15.42). Anterior and posterior wall fractures (Figs. 15.43, 15.44) are limited to the acetabulum and affect only a portion of the corresponding column, including its articular surface, whereas anterior and posterior column fractures separate the entire column from the innominate bone and are almost always associated with an ischiopubic ramus fracture. Rarely an anterior column fracture extends only into the superior pubic ramus and spares the ischiopubic ramus. In this case, the fracture has to originate in the ilium above the anteroinferior iliac spine of the pelvis; otherwise, it is by definition an anterior wall fracture. The most widely used acetabular fracture classification was devised by Letournel and Judet in which five simple (elementary) and five complex (associated) patterns are distinguished (Table 15.2 , Fig. 15.45).
Hip dislocations can be classified as anterior, central (me-dial), and posterior. In anterior dislocation, the femoral head lies medial and inferior to the acetabulum, projecting into the suprapubic or obturator region, and the femur is abducted, externally rotated, and sometimes flexed. Central dislocation (traumatic protrusio acetabuli) is always associated with an acetabular fracture, with the femoral head protruding into the pelvic cavity (Fig. 15.46). Posterior dislocation (Fig. 15.47) is by far the most common type, accounting for almost 90% of all hip dislocations. In posterior dislocation, the femoral head lies lateral and superior to the acetabulum, and the femur usually is internally rotated and adducted. Dislocations are commonly associated with fractures of the pelvis, especially the acetabulum, and fractures of the femoral head and, less commonly, neck. The Thompson and Epstein classification of posterior hip dislocations incorporates associated fractures (Table 15.3). Femoral head fractures (Fig. 15.48) associated with posterior hip dislocations may be subdivided into four types (Table 15.4). In posterior hip dislocations with the fem-oral head being displaced superolaterally, the ligamentum teres (ligamentum capitis femoris) originating in the fovea of the femoral head and inserting into the transverse acetabular ligament at the floor of the acetabulum invariably ruptures or causes an avulsion fracture at the fovea. This avulsion fracture may extend cephalad in the weight-bearing articular surface of the femoral head (Pipkin type 2 fracture) that eventually may result in a deformed femoral head radiographically indistinguishable from sequelae of avascular necrosis.

Elementary fractures | |
Posterior wall | 30% |
Posterior column | 4% |
Anterior wall | 1% |
Anterior column | 4% |
Transverse | 10% |
Associated fractures | |
Posterior column and wall | 4% |
Anterior column or wall and posterior hemitransverse | 7% |
Transverse and posterior wall | 20% |
T-shaped | 7% |
Both columns | 13% |
Fractures of the proximal femur (commonly referred to as hip fractures) may be classified as capital, subcapital, midcervical (transcervical), basicervical, intertrochanteric, and subtrochanteric (Fig. 15.49). Capital fractures are uncommon and usually associated with posterior hip dislocations. Femoral neck fractures (Fig. 15.50) commonly occur in osteoporotic patients (e.g., elderly white women) after minor trauma. Common complications include nonunion, especially in the presence of severe osteoporosis, and avascular necrosis of the femoral head, because its main blood supply derives from branches of the circumflex femoral arteries entering the bone distal to the fracture line at the base of the femoral neck. Fractures of the femoral neck can be classified according to their anatomical location (see Fig. 15.49), the angle the fracture line in the neck forms with the horizontal plane (Pauwels classification, Fig. 15.51), and the displacement of the fracture fragments (Garden classification, Fig. 15.52). Garden 1 is an impacted (“incomplete”) fracture with valgus deformity, Garden 2 a nondisplaced fracture with varus deformity, Garden 3 a displaced fracture with varus deformity, and Garden 4 a fracture with cephalad displacement (foreshortening) of the femur shaft. Garden 1 and 2 fractures are commonly treated with internal fixation using multiple cancellous lag screws, Garden 3 and 4 with hemiarthroplasty.



In intertrochanteric fractures, differentiation between a stable and unstable fracture pattern is largely based on the integrity of the posteromedial cortex (Fig. 15.53), where the calcar is located. In stable fractures, the posteromedial cortex remains intact or has minimal comminution with cortical opposition of the fracture fragments. Intertrochanteric fractures can be classified based on the number of fracture fragments (Fig. 15.54). Two- and three-part fractures in this system tend to be stable, whereas four- and multipart fractures are unstable. Both a two-part intertrochanteric fracture with varus deformity and a two-part fracture of the proximal femur shaft extending into the lesser trochanter (reverse obliquity pattern) are always unstable, the latter because of the tendency for medial displacement of the femoral shaft. Sliding (dynamic) hip screw devices such as gamma nails are used for the operative treatment of intertrochanteric and extracapsular basicervical neck fractures.

Subtrochanteric fractures are classified according to the level of the fracture line (Fig. 15.55) or both location and degree of comminution affecting the stability of the fractures (Fig. 15.56). It is generally accepted that both a more distally located fracture and a greater comminution result in a higher incidence of complications, which include malunion, nonunion, hardware failure, and infection.
Femur shaft fractures are best classified by location (proximal, middle, and distal third or junction between these regions) and fracture morphology, including degree and type of comminution. A simplified AO/OTA classification differentiates between two-part fractures (type A), wedge fractures with butterfly fragments of varying size and possible comminution (type B), and complex fracture, including segmental and multipart comminuted fractures without contact between the proximal and distal diaphyseal segments (type C).
Fractures of the distal femur (Fig. 15.57) are classified as extra-articular supracondylar and intra-articular unicondylar and bicondylar fractures (Fig. 15.58). The severity of the fracture, which is inversely related to the prognosis, progressively increases in this classification system from one type or subgroup to the next. Complications include vascular injuries, infection, painful internal fixation devices (e.g., screws protruding outside the cortex), hardware failure, nonunion, malunion, and post-traumatic osteoarthritis. Loose intra-articular bodies may be the sequelae of osteochondral and meniscal fractures.


Patellar fractures are classified for a treatment-directed approach as either nondisplaced or displaced (Fig. 15.59). A displaced fracture is defined by fracture fragment separation of 4 mm or more or an articular incongruity of 2 mm or more. Descriptive terms such as transverse, vertical, stellate (comminuted), marginal (medial or lateral side), proximal or distal pole, and osteochondral can be used to further describe patellar fractures. Bipartite and, rarely, multipartite patella with the fragments representing accessory ossification center (s) with a smoothly rounded margin are characteristically located in the superolateral aspect of the patella and must be differentiated.









Tibial plateau fractures (Fig. 15.60) are the most common proximal tibia fractures involving either the medial or lateral plateau or both. Schatzker’s classification of tibial plateau fractures is most widely used and differentiates between medial and lateral involvement (Fig. 15.61). Type 1 (split fracture) is a pure cleavage fracture of the lateral tibial plateau. Type 2 (split-depression) is a cleavage fracture of the lateral tibial plateau in which the remaining articular surface is depressed into the metaphysis. Type 3 (depression) is a central depression fracture of the lateral tibial plateau. Type 4 involves the medial tibial plateau either as a split (4A), depression (4B), or split-depression (4C) fracture. Tibial spine fractures are frequently associated. Type 5 is a bicondylar fracture in which the fracture line often forms an inverted Y with intact junction between metaphysis and diaphysis. Type 6 is a tibial plateau fracture in which there is complete dissociation between the metaphysis and the diaphysis. These fractures may have varying degrees of comminution of one or both tibial condyles and the articular surface. Late complications include painful hardware (up to 50%), malunion, and posttraumatic osteoarthritis.
A Segond fracture is an avulsion from the lateral aspect of the proximal tibia just distal to the joint line at the insertion of the reinforced capsule. This fracture is frequently associated with tears of the anterior cruciate ligament and lateral meniscus secondary to varus stress with internal rotation of the flexed knee. The Segond fracture has to be differentiated from an avulsion of the Gerdy tubercle (insertion of the iliotibial tract) that is located anterior and slightly more distal to the former. A reverse Segond-type fracture consists of an avulsion fracture of the medial aspect of the proximal tibia at the insertion of the medial collateral ligament associated with tears of the posterior cruciate ligament and medial meniscus secondary to valgus stress and external rotation of the flexed knee.
Knee dislocation is a relatively rare injury that, besides extensive ligamentous damage and avulsions, is also frequently associated with a neurovascular insult (popliteal artery, peroneal nerve). In order of decreasing frequency anterior, posterior, medial, and lateral dislocations are differentiated. Spontaneous reduction is not uncommon, resulting in underdiagnosis of this injury. Disruption of all four major ligaments of the knee (both cruciate and collateral ligaments) is highly suggestive that a dislocation has occurred. MRI is the imaging modality of choice for the evaluation of knee dislocations.
Patellar dislocation is usually lateral, but it may be transient (spontaneous reduction of a traumatic dislocation). In this case, an osteochondral fracture of the medial patellar facet and lateral femoral condyle may be the clue for the correct diagnosis. Predisposing factors include a patella alta, deficient height of the lateral femoral condyle, shallowness of the patellofemoral groove, and genu valgum or recurvatum.


Proximal tibiofibular joint dislocation occurs anteriorly or, less frequently, posteriorly. Peroneal nerve injury may be associated with the posterior dislocation.
Tibia and fibula shaft fractures occur isolated or together. An isolated fibular shaft fracture is uncommon and results from a direct blow. More typically, an apparently isolated fibular fracture is actually a component of an ankle injury (e.g., Maisonneuve fracture). Because of the subcutaneous location of the anterome-dial surface of the tibia, an open (compound) fracture is not uncommon, resulting in a relatively high incidence of infection with nonunion. The AO/OTA classification of diaphyseal tibial fractures differentiates between two-part fractures (type A), wedge fracture with butterfly fragment (type B), and complex fractures (segmental or multipart fractures, type C). In type A fractures, spiral (A1), oblique (A2), and transverse (A3) fractures are differentiated. In type B fractures, an intact spiral wedge or butterfly fragment (B1), an intact nonspiral wedge in which the butterfly fragment is separated from the tibial shaft by oblique (not spiral) fracture lines (B2), and a fractured wedge (B3) are discerned. Furthermore, for both type A and B fractures, it must be assessed if the fibula is intact or if the tibia and fibula fractures are at the same or a different level. Type C fractures are further subdivided by the number of fracture fragments. Compartment syndrome occurs in about 4% of all tibial shaft fractures, but it is most common in male patients under 35 y of age. The syndrome may affect all four compartments of the lower leg, but it is always present in the anterior compartment. The diagnosis is made by monitoring the compartment pressure and can be supported by MRI.
In the ankle, axial-loading injuries resulting in tibial plafond (pilon) fractures and rotational ankle injuries resulting in malleolar fractures are differentiated. It has to be kept in mind, however, that axial load and rotational forces may coexist in an ankle injury, resulting in a more complex fracture pattern.
Tibial plafond (pilon) fractures (Fig. 15.62) typically result from motor vehicle accidents or falls from heights. Classifying these fractures by description, the displacement of the talus and articular fragments should be noted. The talus is frequently proximally displaced, but it may translate in any direction. The degree of comminution of both the articular surface and the metaphyseal area of the distal tibia must be assessed. The presence or absence of an associated fibula fracture and, if present, its location and degree of comminution also need to be evaluated. All these factors are essential in treatment planning and outcome prediction. Distal tibia fractures are divided by the AO/OTA classification system into the following categories: type A, nonarticular fractures; type B, partial articular fractures (these fractures are similar to rotational ankle fractures with extension into the tibial plafond and will be discussed later in this chapter); and type C, total articular fracture. Intra-articular tibial plafond (pilon) fractures are classified into three types. Type 1 is a nondisplaced cleavage fracture, type 2 a minimally comminuted and displaced fracture with articular incongruity but without depression of any articular fracture fragment, and type 3 a highly comminuted and displaced fracture (Fig. 15.63).
Rotational ankle fractures can be classified by location as unimalleolar, bimalleolar, trimalleolar, or complex (comminuted intra-articular fracture of the distal tibia associated with a distal fibular fracture, indistinguishable from a pilon fracture). Rotational injuries of the ankle are commonly caused by supination (inversion, adduction) or pronation (eversion, abduction) of the foot and may be associated with external (lateral) rotation of the foot. These injuries may be ligamentous, osseous, or a combination of both. Rotational ankle fractures can be classified by either anatomical location or injury mechanism. The Weber classification is based on the level of the fibular fracture: type A fracture is at or below the level of the ankle joint line, type B fracture originates at the level of the joint line or slightly above it and progresses superiorly, and type C fracture is located 2 cm or higher above the ankle joint line (Fig. 15.64). Type C fractures correspond to the pronation-external rotation (PER) fracture of the Lauge–Hansen classification (Fig. 15.65), which is based on the injury mechanism. These fibular shaft fractures associated with ankle injuries are often better known by their eponym. A Maisonneuve fracture is a pronation external rotation type injury consisting of a proximal fibula fracture, disruption of the tibiofibular syndesmosis distal to this fracture, and a medial malleolar fracture or a torn medial collateral (deltoid) ligament. A Dupuytren fracture consists of a distal fibula fracture 2 to 7 cm above the ankle joint line associated with disruption of the distal tibiofibular syndesmosis and the medial collateral (deltoid) ligament. The same injury with intact tibiofibular syndesmosis is termed a Pott fracture.






Avulsion fractures predominate in the talus and occur in the superior aspect of the head and neck and in the lateral, medial, and posterior aspects of the body. These fractures are frequently associated with ankle injuries. Major talar fractures may involve the head, neck, body, and the lateral or posterior process (Fig. 15.66). Of these, talar neck fractures are the most common and typically depict a vertical fracture course. The modified Hawkins classification differentiates four types of talar neck fractures. Type 1 is an undisplaced fracture without dislocation. Type 2 refers to a talar neck fracture with associated dislocation of the subtalar joint. This is the most common type. Type 3 is a talar neck fracture with dislocation of both the ankle and subtalar joint. Type 4 is also associated with subluxation or dislocation in the talonavicular joint (Fig. 15.67). Osteonecrosis of the proximal fracture fragment is a common complication of talar neck fracture. It is relatively rare in Hawkins type 1 fractures but may reach close to 100% in type 4 fractures. The appearance of a linear subchondral lucent area (Hawkins sign) in the talar dome after 1 to 3 months relates to hyperemia and continuity of blood supply and should not be misinterpreted as a crescent sign of osteonecrosis. At this stage, osteonecrosis manifests itself as relatively increased density in the proximal talar fragment when compared with the distal one.
Besides rare talar body fractures (Fig. 15.68) presenting in a variety of fracture patterns, osteochondral fractures of the talar dome and fractures involving either the lateral or posterior process of the talar body are more common and must be recognized as separate entities. The lateral talar process is a large, broad-based, wedge-shaped prominence of the talar body and includes two articular surfaces. Dorsolaterally, it articulates with the fibula and inferomedially with the anterior portion of the posterior facet of the calcaneus. CT is frequently required for the diagnosis of a lateral process fracture (Fig. 15.69). Differentiation of an os trigonum from a posterior process fracture may be difficult at times, particularly when the former is diseased. Osteochondral fractures (Fig. 15.70) of the medial or lateral talar dome result from shearing or rotatory forces applied to the articular surface in conjunction with an ankle injury. Differentiation of an osteochondral fracture from osteochondritis dissecans is not always possible based on imaging examinations alone. A chondral fracture limited to the joint cartilage without involvement of the subchondral bone is not appreciated by CT and requires CT arthrography or MRI for diagnosis.


Dislocation of the talus can occur with or without major talar fractures. A subtalar (peritalar) dislocation has to be differentiated from a total talar dislocation. A subtalar dislocation involves simultaneous dislocations of the talocalcaneal and talonavicular joint. Subtalar dislocations occur in any direction. Up to 85% of dislocations are medial, in which the calcaneus and the rest of the foot are displaced medially. The navicular is located medial and sometimes dorsal to the head and neck of the talus. Lateral subtalar dislocations are second in frequency, followed by anterior and posterior subtalar dislocations. In the total talar dislocation, the ankle is, besides the talocalcaneal and talonavicular joint, also completely dislocated (not only subluxed), resulting in a “floating talus.” Talar osteonecrosis is a frequent complication in this condition.

Calcaneal fractures (Fig. 15.71) are the most common tarsal fractures. They can be intra-articular (75%) or extra-articular (25%). Extra-articular calcaneal fractures are typically caused by either twisting forces, resulting in fractures of the tuberosity, sustentaculum tali, or anterior process, or a pull by the Achilles tendon, resulting in a beaklike avulsion fracture of the postero-superior aspect of the calcaneus. Intra-articular fractures occur in vertical falls in which the talus is driven into the calcaneus. This injury mechanism is bilateral in 10%. Calcaneal fractures can be classified based on both anatomical location and injury mechanism (Fig. 15.72). A specific calcaneal fracture classification system for CT was devised by Sanders (Fig. 15.73). Based on the oblique coronal plane perpendicular to the posterior facet, this structure is divided into three equal segments, defined as lateral (A), central (B), and medial (C). All nondisplaced articular fractures (< 2 mm), regardless of the number of fracture lines, are designated as type 1 fractures. Type 2 are two-part fractures of the posterior facet. Three types are differentiated, depending on the location of the fracture line in the lateral segment (2A), central segment (2B), or medial segment (2C). Type 3 are three-part fractures that usually feature a centrally depressed fragment. Based on the location of the two fracture lines in the posterior facet, the following fracture can be identified: 3AB, 3AC, and 3BC. Type 4 are four-part or multipart highly comminuted fractures of the posterior facet.
In the navicular bone, dorsal avulsion fractures related to the talonavicular or naviculocuneiform ligament insertion are most common. An os supranaviculare or os infranaviculare, respectively, must be differentiated from these avulsion fractures. Fracture of the navicular tuberosity at the insertion of the tibialis posterior is another traction type injury that should not be confused with an os tibiale externum (os naviculare secundarium). Body fractures of the navicular are horizontal (splitting the navicular into dorsal and plantar segments), vertical (resulting in medial and lateral segments), or comminuted. An isolated dislocation or subluxation of the navicular is usually associated with a neuropathic foot.




Cuboidal fractures and dislocations rarely occur as an isolated entity, but they are not uncommon in association with other tarsal bone injuries and complex Lisfranc joint disruptions. Avulsion fractures and, less frequently, two-part or comminuted body fractures are recognized. A fracture of the os peroneum, a sesamoid within the peroneus longus tendon, can clinically simulate an isolated cuboid injury. A bipartite os peroneum has to be differentiated from a fracture of this sesamoid.
Fractures of the cuneiforms are usually associated with tarsometatarsal joint injuries. The spectrum of these injuries ranges from simple sprains to complex tarsometatarsal dislocations, also referred to as Lisfranc fracture-dislocations (Fig. 15.74). Severe injuries with instability occur from high-energy trauma, such as a fall from a height or motor vehicle collision. Three types of Lisfranc joint instability can be differentiated in severe injuries: (1) first ray separation, evident as medial subluxation of the first metatarsal as an isolated finding or associated with widening of the space between the medial and intermediate cuneiforms; (2) homolateral dislocation of the first to fifth metatarsal; and (3) divergent dislocation, with lateral displacement of the second through the fifth metatarsal and medial or absent displacement of the first metatarsal (Fig. 15.75). Dorsal (rarely plantar) subluxation/dislocation in the tarsometatarsal joints is frequently associated. Fractures may be present in all tarsometatarsal joints, but they are most common in the base of the second metatarsal, followed by the third metatarsal and the medial and intermediate cuneiforms. Metatarsal fractures involving the shaft or neck may be transverse, oblique, spiral, or comminuted. Fractures of the metatarsal head are uncommon and, when present, usually associated with more typical fractures of adjacent metatarsals. In the fifth metatarsal, an intra-articular avulsion of the tuberosity at the peroneus brevis insertion has to be differentiated from a Jones fracture, which refers to an extra-articular transverse fracture of the proximal shaft. Jones fractures have a high incidence of nonunion.
Metatarsophalangeal injuries most commonly occur in the first metatarsophalangeal joint. Dislocations can occur in any direction, but in the first metatarsophalangeal joint they typically occur in dorsal or plantar direction. Hyperdorsiflexion injuries of the first metatarsophalangeal joint include both a turf toe and a sesamoid fracture (Fig. 15.76). These conditions are best assessed with MRI. A sesamoid fracture may be difficult to differentiate from a partite sesamoid. On CT, a fractured sesamoid has rough, irregular borders, and there is only minimal separation of the fragments unless the plantar plate is torn. The partite sesamoid has smooth sclerotic edges, and the sum of the partite sesamoids makes a sesamoid larger than a normal one (Fig. 15.77).



Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree