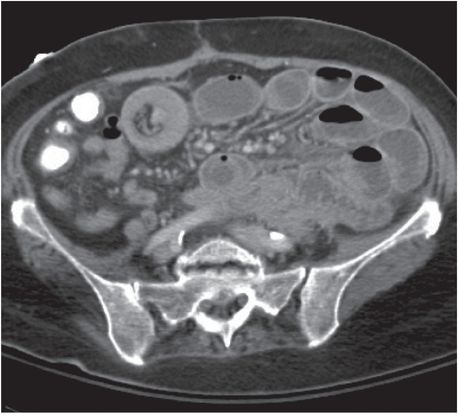
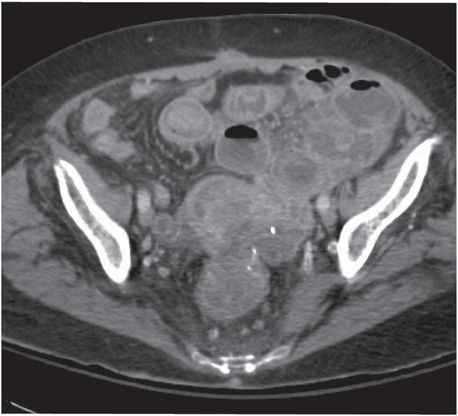
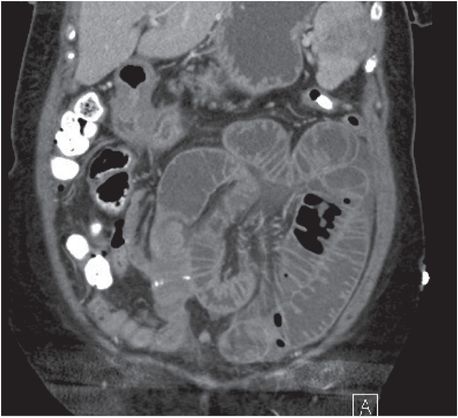
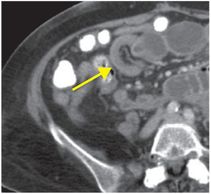
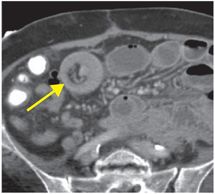
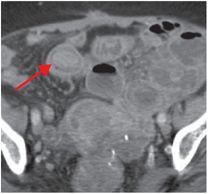
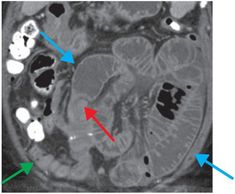
Diagnosis: Small bowel obstruction (secondary to intussusception from metastatic ovarian cancer)
Axial (first three images at left) and coronal (last image at right) contrast-enhanced CT images show invagination of a bowel loop with its mesenteric fold (intussusceptum, yellow arrows in first two images) into the lumen of a contiguous portion of bowel (intussuscipiens). A soft tissue mass (red arrows in final two images) acts as the lead point. Proximally, obstructed small bowel is dilated and fluid-filled (blue arrows), while distally, the small bowel is decompressed (green arrow).
Discussion
Role of imaging in suspected small bowel obstruction
Small bowel obstruction (SBO) accounts for 12–16% of surgical admissions for acute abdominal pain.
Nausea and vomiting are typical clinical symptoms. Clinical exam and labs are often insufficient for differentiating simple obstruction from strangulated bowel.
CT is the primary modality for imaging suspected acute SBO and answers the following questions:
Is there a mechanical obstruction? Mechanical obstruction is characterized by proximally dilated small bowel loops (>2.5 cm between the outer walls) with distal loops that are normal in caliber or decompressed.
How severe is the obstruction, if present?
Mild (low grade): 25–50% discrepancy between proximal and distal small bowel caliber.
Moderate (intermediate grade): >50% discrepancy, with residual gas or contrast in distal small bowel.
Severe (high grade): >50% discrepancy, with completely collapsed distal small bowel and colon that do not contain residual gas, stool, or contrast.
Where is the obstruction located? Multiplanar reformats are helpful for determining the site and level of the obstruction. The site of obstruction, or “transition point,” is where the caliber change occurs. Two transition points are present in “closed loop” obstruction, which is a surgical emergency.
What is the cause of the obstruction? The transition point should be carefully inspected to help determine the etiology of the obstruction. The most common cause of SBO is adhesions, which are generally invisible or detectable only by inference on CT. Bowel loops obstructed by adhesions may be abnormally angulated or appear tethered to the abdominal wall or other structures.
Other common causes include hernias, Crohn’s disease, and neoplasms.
Less common causes include intussusception, gallstones, hematomas, tuberculosis, radiation enteritis or fibrosis, endometriosis, and foreign bodies.
Is strangulation present? Signs of bowel ischemia include decreased bowel wall enhancement, wall thickening, mesenteric fluid/congestion, and ascites.
Does the patient require emergency surgery? Is there a closed loop obstruction or evidence of strangulation/ischemia?
Clinical synopsis
The patient was deemed a poor surgical candidate due to comorbidities and was treated with a gastrostomy tube for palliative decompression.
Self-assessment
| • What is the “small bowel feces” sign? |
|
| • Name four signs of a closed loop obstruction. |
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








