16 Colloid Cyst
16.1 Introduction
Colloid cysts are histologically benign lesions most often located in the roof of the third ventricle near the foramen of Monro. Although they harbor the dangerous potential to create obstructive hydrocephalus, they may also present as asymptomatic, incidental findings. In this chapter, we discuss imaging and demographic risk factors that may help predict the development of symptoms, including obstructive hydrocephalus. In addition, we demonstrate the varying appearance of colloid cysts and show interesting companion cases in which alternative pathologies mimicked a colloid cyst.
16.2 Case presentation
16.2.1 Clinical History
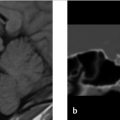
A 21-year-old man presented to the emergency room after a high-speed motorcycle accident with loss of consciousness at the scene. He complained of back pain but denied headache, nausea, or vomiting. A noncontrast head CT was obtained (see ▶ Fig. 16.1).

16.3 Imaging Analysis
16.3.1 Imaging Findings
The noncontrast head CT (▶ Fig. 16.1) reveals a 3-mm hyperdense lesion in the region of the foramen of Monro. The ventricles are normal in size.
16.3.2 Additional Imaging Performed
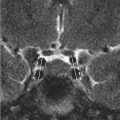
An MRI of the brain was performed to evaluate the finding on the head CT. The brain MR imaging findings are shown in ▶ Fig. 16.2.

16.4 Clinical Evaluation
16.4.1 Neurosurgery Evaluation
The patient denied having a headache (HA) in the ED and had no history of HAs. Neurological examination was normal.
16.4.2 Clinical Management
As this is an incidentally detected, asymptomatic, 3-mm CC with normal-sized ventricles, conservative management with imaging follow-up was elected. The patient was instructed that, although unlikely, the cyst could enlarge. If they experienced a sudden onset of HA or new neurological complaint, they should seek emergency medical attention. If they remained asymptomatic, they were instructed to return to the neurosurgical clinic for a follow-up appointment with a neurosurgeon at which time a follow-up noncontrast head CT would be obtained in 1 year.
16.5 Differential Diagnosis for Masses in the Region of the Foramen of Monro
Cysts
Colloid cyst (CC):
A round or oval shaped, well-defined mass, in the anterosuperior aspect of the third ventricle is virtually pathognomonic of a CC.
Majority are hyperdense on CT, which is more sensitive than MRI for small, hyperdense cysts. 1
Neurocysticercosis (NCC):
Intraventricular, vesicular stage should be considered especially in endemic areas:
Isointense to cerebrospinal fluid (CSF).
A hyperintense scolex may be seen, whereas the infrequently reported intracystic nodule of a CC is hypointense on T2 W image.
NCC vesicular cysts are mobile and most frequently found in the fourth ventricle.
Racemose form:
Numerous cysts, most commonly in the basilar cisterns, that incite inflammatory reaction and cause obstructive hydrocephalus.
Arachnoid, ependymal, and choroid plexus cysts 2 , 3 , 4 have rarely been reported to mimic CC but should follow CSF in signal intensity and density, unlike a CC.
Artifact
Flow void in the third ventricle on MRI due to CSF pulsation through the foramen of Monro 2 (see “Pearls and Pitfalls” and Companion Case 3”).
Vascular
Dolichoectatic basilar artery or basilar artery aneurysm displacing the floor of the third ventricle superiorly. 2 , 5
May mimic a CC on a single axial imaging, but its continuity with an ectatic, high-riding basilar artery, or basilar artery aneurysm can be confirmed in the coronal or sagittal plane.
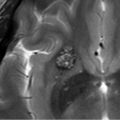
Cavernous malformation 6 and arteriovenous malformation 7 have been reported to mimic CC but are parenchymal rather than in the third ventricle. Cavernous malformations may have contrast enhancement. The blood products often have a hemosiderin ring appearance on GRE (gradient recalled echo) or susceptibility weighted imaging (SWI) type images with diffuse T1 shortening in the surrounding parenchyma (see Companion Case 7).
Tumor
Subependymoma:
Typically located in the floor of the fourth ventricle or the frontal horn of the lateral ventricle rather than the third ventricle.
Metastatic disease (see Companion Case 4); intraventricular craniopharyngioma (see Companion Case 8); choroid plexus tumor (primary, secondary); intraventricular meningioma; central neurocytoma; glioma and pituitary adenoma have rarely been reported to mimic CCs. 2 , 5 , 8 , 9
Miscellaneous
A punctate (≤ 1 mm) high-attenuation focus that is very well seen despite its small size is likely a tiny calcification within a vessel or choroid plexus (see Companion Case 7).
Intraventricular hemorrhage:
Associated with other areas of intraventricular hemorrhage (IVH).
Transient finding associated with other IVH and/or subarachnoid hemorrhage.
Special Considerations in the Pediatric Population
SEGA (subependymal giant cell astrocytoma; see companion case 6):
Most common lesion near the foramen of Monro in children as CCs are rare in the pediatric population.
Solid, prominently enhancing mass with calcification.
Found in some children with tuberous sclerosis complex (TSC). 5 Images should be inspected for additional associated findings such as cortical tubers and small subependymal hamartomatous nodules although patients presenting with SEGA often will not have other manifestations of the condition even though they carry the genetic mutation in TSC1 and/or TSC2.
LCH (Langerhans cell histiocytosis) and pilocytic astrocytomas have rarely been reported to mimic CCs. 5 , 13
16.6 Pearls and Pitfalls
CSF flow artifacts represent a major cause of “false-positive” MRI diagnosis of CCs. They are due to rapid or turbulent CSF flow causing signal loss within the ventricles (see Companion Case 3):
Flow artifacts occur most commonly on the fluid-attenuated inversion recovery (FLAIR) sequence in the frontal horns of the lateral ventricles and the third ventricle adjacent to the foramen of Monro. 2 , 5
Inconsistent appearance on multiple sequences, pulsatility artifact, and lack of confirmation on the sagittal T1 W image should raise the possibility of a flow artifact.
Confirmation with head CT may be helpful as flow artifacts are not present on CT imaging.
Initial incidental detection of a CC is often by head CT, which, in almost all cases, is how very small, hyperdense cysts are best seen. 1
CCs may be very difficult to see on FLAIR if they are low in signal on T2 W images because they may be isointense to the suppressed CSF.
CCs do not cause restricted diffusion, create edema in the adjacent brain parenchyma, or have prominent thick, nodular, or homogenous enhancement. Any of these findings should prompt consideration of a broader differential diagnosis.
16.7 Essential Facts about Colloid Cysts
16.7.1 Key Components of the Radiologist’s Report
Size of the cyst is usually measured on the axial imaging sequence on which it is best seen. In oval cysts, with an asymmetrically larger superior to inferior dimension, this may underestimate the cyst’s size.
T2 signal intensity: low signal cysts may be more difficult to aspirate by the surgeon. 14 , 15
FLAIR signal intensity: high signal on FLAIR has been found in some studies to indicate cysts that are more likely to be or become symptomatic. 16
Location of the cyst relative to the foramen of Monro 16 (see ▶ Fig. 16.3, third ventricular risk zones).
Size of ventricles: dilation of temporal horns and rounding of frontal horns are sensitive indicators of early hydrocephalus as is increased signal in the periventricular white matter on FLAIR. Comparison with prior studies, when available, is essential to look for subtle change in the size of the cyst and/or ventricles.
Presence of a cavum septum pellucidum or cavum vergae should be noted as these anatomic variants may affect the surgical approach.
Presence of a frontal lobe venous angioma should be noted as this may affect the surgical approach.

16.7.2 Imaging Features of Colloid Cysts
CCs are well-defined and round or oval in shape, with their signal intensity and density dependent upon their cholesterol content and hydration status. 2
Two-thirds are hyperdense on CT. The remainder are iso- to hypodense. Calcification is rare. 17
The “black hole” effect on MR is present in 25% (inspissated debris within the cyst forms a center that is black on T2 W images and is surrounded by proteinaceous fluid that is bright). 2
Uncommonly, the cyst may be T2 and/or FLAIR “bright” and have a small central or mural nodule that is usually dark. This unusual appearance is reminiscent of a Rathke cleft cyst’s mural nodule. 18 , 19
Ninety-nine percent are located in the foramen of Monro. Rarely they have been reported in the lateral and fourth ventricles, frontal lobe, cerebellum, cavum septum pellucidum, and vellum interpositum. 2 , 20 , 21 , 22
16.7.3 Third Ventricular“Risk” Zones
The precise location of the CC within the third ventricle has been reported by Beaumont et al to be a risk factor for cysts that are or may become symptomatic 16 (see ▶ Fig. 16.3):
Zone 1: Extending from the lamina terminalis posteriorly to a tangent line between the mammillary bodies and the anterior aspect of the mass intermedia. Cysts in zone 1 are considered at risk of occluding the foramen of Monro.
Zone 2: Extending from the posterior aspect of zone 1 to the anterior border of the cerebral aqueduct. Cysts in zone 2 are considered at low risk of obstructing CSF flow.
Zone 3: Extends from the posterior aspect of zone 2 to the posterior border of the third ventricle. Cysts in zone 3 are considered at risk of occluding the cerebral aqueduct.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree