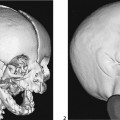
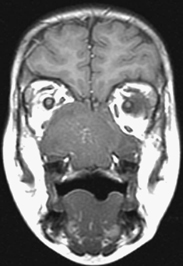
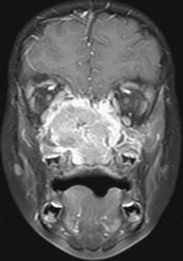
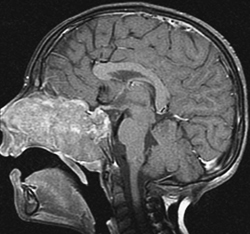
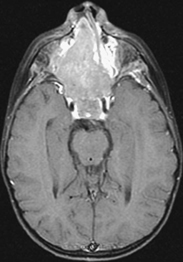
CASE 19 A 4-year-old boy presents with nasal obstruction. Figure 19A Figure 19B Figure 19C Figure 19D There is a huge soft tissue mass with malignant features centered in the nasopharynx. Unenhanced T1-weighted coronal image (Fig. 19A) shows a slightly hyperintense to muscle mass filling the nasal cavities and infiltrating the medial aspects of both orbits, greater on the right than on the left. Following contrast there is intense heterogeneous enhancement, as shown on the corresponding coronal fat-suppressed T1-weighted image (Fig. 19B). Sagittal and axial fat-suppressed, contrast-enhanced, T1-weighted images (Figs. 19C and 19D) better show its extent. Anteriorly it involves both nasal cavities. There is destruction of part of the nasal septum, and the residual septum is displaced to the left. The tumor extends into the medial maxillary sinuses, whereas posteriorly it involves the clivus. Superiorly the cavernous sinus is infiltrated, displacing the carotid arteries laterally. It also involves the frontal bone and adjacent dura. Rhabdomyosarcoma Most masses in the pediatric head and neck are benign, consisting primarily of congenital, developmental, or inflammatory lesions. Malignant tumors are less common in children, but 35% of all pediatric sarcomas manifest in the head and neck region. The rhabdomyosarcoma family is the most common soft tissue malignancy encountered in childhood. Rhabdomyosarcoma is essentially a disease of childhood and young adults. There is a bimodal age distribution, with one peak during childhood and another peak during adolescence. Most arise before age 12 years. There is a slight male predominance. Rhabdomyosarcomas are thought to arise from primitive mesenchymal tissue expressing myogenic (skeletal muscle) differentiation, probably satellite cells associated with skeletal muscle embryogenesis. They can develop in any part of the body, including those not containing muscle, with the exception of bone (to which it commonly metastasizes). Rhabdomyosarcomas can spread by direct extension and may erode directly through bone or extend through skull-base foramina via a perineural spread to produce epidural masses with occasional meningeal involvement. They also may extend along lymphatic vessels to lymph nodes or hematogeneously to lung, liver, bone, and bone marrow. Classification of sarcomas according to anatomic location in the head and neck is helpful because of the influence of location on presentation and disease management. Common locations include orbital (Figs. 19E1 and 19E2), parameningeal, or nonparameningeal sites. Parameningeal sites are the most common locations and have a poorer prognosis. These sites include the middle ear, nasal cavity, paranasal sinuses, nasopharynx, and infratemporal fossa. Nonparameningeal regions include the parotid gland, oral cavity, oropharynx, hypopharynx, larynx, thyroid/parathyroid, and neck. Staging depends on local extension, regional and distant metastases, and amount of residual tumor remaining after surgical resection.
Clinical Presentation
Radiologic Findings
Diagnosis
Differential Diagnosis
Discussion
Background
Etiology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree