21 Pituitary Gland: Diffuse Enlargement
21.1 Introduction
Unlike pituitary micro- and macroadenomas, there are no well-established guidelines for the evaluation of an incidentally detected, diffusely enlarged pituitary gland. Consideration of the age and sex of the patient is a key factor in determining the differential diagnosis and deciding whether any further investigation is warranted. In this chapter, we will discuss the normal appearance of the pituitary gland and the most common underlying conditions that are associated with diffuse enlargement.
21.2 Case Presentation
21.2.1 History
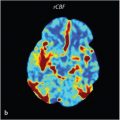
A 29-year-old woman presented with headaches. Dedicated pituitary images were performed for “prominence of the pituitary gland” detected on a routine brain MRI (▶ Fig. 21.1).

21.3 Imaging Analysis
21.3.1 Imaging Findings and Impression
The pituitary gland appears mildly enlarged and homogeneously enhancing, measuring 11 mm in height × 10 mm in transverse dimension. No focal area of heterogeneity is seen on the T1- or T2 W images. It is convex superiorly where it contacts but does not compress the optic chiasm. The gland is symmetric and the stalk midline. The cavernous sinuses are normal (▶ Fig. 21.2).

Incidentally detected, mild pituitary enlargement that is homogenous and symmetric most often represents physiologic hyperplasia or secondary pituitary hypertrophy. Convexity of the superior aspect of the gland is normal in peripubescent females but atypical for a 29-year-old woman. Considerations include pregnancy as well as other causes of physiologic hyperplasia and secondary hypertrophy.
21.3.2 Additional Imaging Recommended
None. Clinical correlation is needed.
21.4 Clinical Evaluation
21.4.1 Endocrinologist Evaluation
This is a 29-year-old woman who presents with an incidentally detected, enlarged pituitary gland. She denies galactorrhea or breast tenderness. Menses are regular. There is no fatigue, constipation, dry skin, nausea, or loss of appetite. She denies polydipsia or nocturia.
The physical examination is unremarkable.
21.4.2 Recommended Laboratory Testing and Results
Pregnancy test: negative.
PRL: 28.2 ng/mL (3–30 ng/mL).
Thyroid-stimulating hormone (TSH): 0.6 mIU/L (0.5–5.0 mIU/L).
Free T4: 1.4 ng/dL (0.8–1.8 ng/dL).
21.4.3 Clinical Impression
This is a well-appearing woman without signs or symptoms of hormonal dysfunction. It was important to exclude pregnancy, which would be the most common cause of this finding. In this asymptomatic patient, this mildly enlarged gland is most likely a normal variant of physiologic hyperplasia. A follow-up MR was performed 5 months later and showed a completely stable appearance of the pituitary gland.
21.4.4 Recommendations
No further testing was recommended.
21.5 Differential Diagnosis of Diffuse Enlargement of the Pituitary Gland
Common
True physiologic hyperplasia:
In the female, normal physiologic change during puberty may cause the superior aspect of the gland to become convex. Pregnancy should also be considered during which pituitary volume increases due to lactotroph and gonadotroph hyperplasia. Milder enlargement due to gonadotroph hyperplasia may occur during the perimenopausal period due to estrogen deficiency.
Pathological hyperplasia:
This is most commonly secondary to end organ failure, specifically hypothyroidism or hypogonadism.
Macroadenoma/microadenoma:
Rarely, the lesion may be of similar signal intensity to the normal gland with homogeneous enhancement, making the tumor difficult to detect as a separate entity.
Uncommon
Congenitally small sella:
If the sella is congenitally small, the gland may bulge superiorly but not actually be increased in volume.
Tortuous cavernous carotid arteries:
If the cavernous carotids are tortuous and converge medially, they may cause the gland to project superiorly but not be increased in overall volume.
Uncommon Causes in Which the Pituitary Enlargement Is a Nonincidental, Important Finding
Cerebrospinal fluid (CSF) hypotension.
Lymphocytic hypophysitis.
Langerhans cell histiocytosis (LCH).
Neurosarcoidosis.
Pituicytoma.
Lymphoma/leukemia.
Metastatic disease.
21.6 Clinical and Diagnostic Imaging Pearls
Know What Is Normal
Prepuberty: ≤ 6 mm.
Postmenopausal females and males: ≤ 8 mm.
Premenopausal females: ≤ 9 mm.
In females during puberty, the superior margin of the gland may become convex.
The gland enlarges throughout pregnancy and may rarely reach 12 to 15 mm in height but usually does not exceed 10 to 11 mm.
Correlate Clinically
A peripartum female who is asymptomatic with a diffusely enlarged gland most likely has normal physiologic hypertrophy.
Pregnancy should always be considered in a female with a diffusely enlarged gland.
A diffusely enlarged gland in a male child is most likely due to pituitary hyperplasia resulting from end organ failure (i.e., hypothyroidism) as pituitary adenomas are rare in this population.
A peripartum female, or patient on immune therapy for malignancy and/or with a history of autoimmune disorders (i.e., thyroiditis) who is not asymptomatic but has headaches and visual complaints and confusion secondary to low serum sodium, may have lymphocytic hypophysitis. MR in these patients often reveals diffuse enlargement of the pituitary gland, loss of the normal posterior pituitary bright spot, and thickening of the stalk. Associated clinical abnormalities include adrenal insufficiency, diabetes insipidus, prolactin (PRL) elevation, and hypopituitarism.
If a patient is symptomatic with postural headaches, consider CSF hypotension. Important additional findings on MR may include tonsillar ectopia, distended dural sinuses, enhancing subdural “collections,” decreased CSF cisterns about the brainstem, and anteroposterior elongation of the midbrain.
21.7 Companion Cases
21.7.1 Companion Case 1
Case Presentation
History
The patient is a 42-year-old woman with a possible pituitary lesion seen on routine brain MR for headaches.
Imaging Analysis
MRI Findings
On the dedicated pituitary protocol MR performed for further evaluation, an ill-defined “lesion” was called on the postcontrast sagittal T1 W images, which could not be confirmed on the coronal pre- or postcontrast T1 W nor the T2 W images. Note is made of the normal midline position of the pituitary stalk and overall normal shape and size of the gland without expansion of the sellar floor.
A follow-up MR was recommended.


Follow-up MRI
The recommended 1-year follow-up MR for the “possible incidental microadenoma” is shown in ▶ Fig. 21.5.

Follow-up MRI Findings and Impression
There has been interval enlargement of the pituitary gland, which remains homogeneous without a discrete lesion. The stalk is midline and the cavernous sinuses are normal. The previously identified “incidental pituitary microadenoma” is no longer seen and was probably not a true abnormality but rather mild heterogeneity in the enhancement of the gland, the appearance of which can be accentuated by technical factors such as narrowing the display window or by dynamic imaging after the administration of contrast.
This interval development of diffuse enlargement of the pituitary gland in a 43-year-old woman is of uncertain significance; clinical correlation will be needed. The patient reported prior to the MR that she was not pregnant, which was verified by subsequent testing.
Clinical Evaluation
Endocrinology Evaluation
This is a 43-year-old woman who initially presented for evaluation of a possible pituitary microadenoma. Her medical history includes hypothyroidism, which was diagnosed 10 years ago.
Initial Testing Performed for Possible “Microadenoma” 1 Year Ago When Patient Was Asymptomatic
PRL: 23.2 ng/mL (4.8–23.3 ng/mL).
Insulin-like growth factor 1 (IGF-1): 125 ng/mL (98–261 ng/mL).
TSH: 2.3 mIU/L (0.5–5.0 mIU/L).
Free T4: 1.2 ng/dL (0.8–1.8 ng/dL).
One-year Follow-up Evaluation
Since the prior evaluation, she reports new constipation and fatigue. Physical examination is notable for dry skin and slightly delayed relaxation of deep tendon reflexes in her upper and lower extremities.
Additional Testing Results:
Pregnancy test: negative.
TSH: 214 mIU/L (0.5–5.0 mIU/L).
Free T4: 0.5 ng/dL (0.8–1.8 ng/dL).
Cortisol: 14.5 µg/dL (5–25 µg/dL).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree