

Diagnosis: Tubo-ovarian abscess (TOA)
Sagittal grayscale transvaginal ultrasound image of the right adnexa (A) demonstrates a complex right adnexal lesion (yellow arrows) that measures up to 5 cm. The lesion was inseparable from the ovarian parenchyma at real-time imaging. Sagittal grayscale transvaginal ultrasound image with color Doppler overlay (B) demonstrates peripheral blood flow.
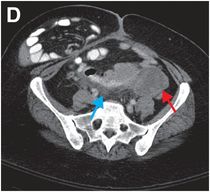
Contrast-enhanced axial CT of the pelvis in the same patient demonstrates corresponding bilateral adnexal complex fluid collections (red arrows) and midline inflammatory fat stranding (blue arrow). Incidentally, there is a fibroid uterus and an uncomplicated bowel-containing right ventral hernia.



Discussion
Tubo-ovarian abscess (TOA) is pyogenic infection of the ovary and/or the fallopian tube.
TOA is considered the most severe form of pelvic inflammatory disease (PID). Clinical signs and symptoms include abdominal or pelvic pain, fever, leukocytosis, and palpable mass.
Causes of TOA include prior pelvic surgery, older intra-uterine devices such as the Dalkon shield, and infertility treatments.
If left untreated, TOA is associated with abscess rupture, peritonitis, adhesion formation, chronic pelvic pain, and impaired fertility.
Ultrasound is the imaging test of choice for suspected TOA.
The sensitivity of ultrasound is approximately 82% and specificity is up to 90%.
The typical appearance of TOA is a predominantly hypoechoic, complex cystic, thick-walled adnexal mass.
CT or MRI can be helpful problem-solving modalities. CT is used if ultrasound demonstrates nonspecific or atypical findings, or if initial therapy is ineffective. In comparison to ultrasound, MRI is capable of demonstrating smaller amounts of fluid and may better demonstrate fluid-filled fallopian tubes and abscesses in some cases.
Treatment decisions vary based on clinical picture.
Medical management includes administration of broad-spectrum IV antibiotics with anaerobic coverage.
If there is no clinical improvement within 2–3 days, ultrasound- or CT-guided drainage may be performed.
Laparotomy may be indicated if ruptured TOA is suspected, if perforated viscus cannot be excluded from the differential diagnosis, or if hysterectomy or salpingo-oopherectomy is necessary.
Clinical synopsis
The patient underwent CT-guided drainage of bilateral TOAs, and approximately 100 mL of purulent fluid was aspirated from the right-sided collection.
Self-assessment
|
|
Spectrum of tubo-ovarian abscess
CT imaging of TOA
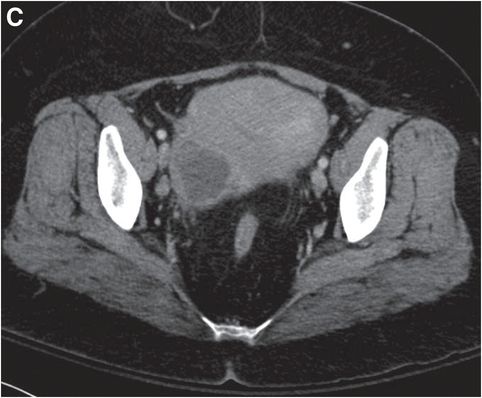
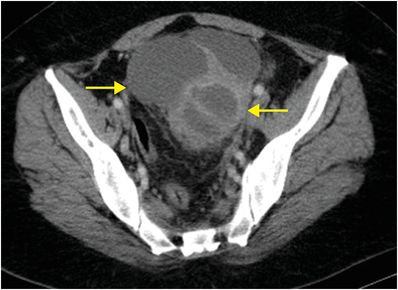
CT is utilized to determine extent of disease and assess complications. It is also indicated when the patient is not responding to antibiotic therapy or for planning in cases where drainage catheter placement is being considered. Internal foci of gas are specific for abscess; however, they are not often seen in TOA. Secondary CT findings include adjacent fat stranding, indistinct margins of nearby bowel loops, and thickening of the broad ligament. Axial and coronal contrast-enhanced CT images of the pelvis demonstrate a thick-walled, septated, low-density adnexal mass (arrows).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








