Diagnosis: Ectopic pregnancy
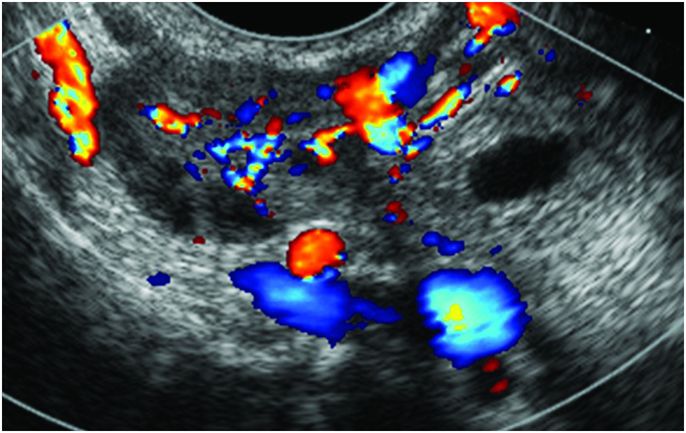
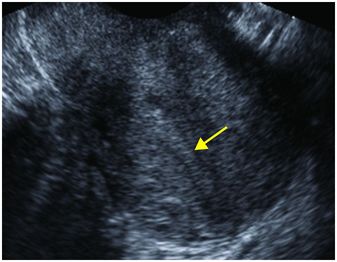
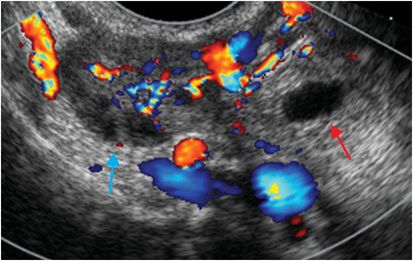
Grayscale transvaginal transverse ultrasound view of the uterus demonstrates no intrauterine gestational sac. The echogenic endometrial stripe is thin and linear (yellow arrow). Transvaginal ultrasound of the right adnexa with color Doppler overlay demonstrates an echogenic, ring-shaped ectopic gestational sac in the right adnexa (red arrow) that is separate from and medial to the right ovary (blue arrow). There is Doppler flow within the wall.
Discussion
Ectopic pregnancy is the most common cause of pregnancy-related mortality in the first trimester.
Approximately 2% of all pregnancies are ectopic.
Risk factors include prior ectopic pregnancy, history of gynecologic surgery, infertility, in vitro fertilization, endometriosis, history of placenta previa, intrauterine device, and smoking.
A history of pelvic pain along with a positive beta human chorionic gonadotropin (β-hCG) level should trigger an evaluation for ectopic pregnancy.
In addition to measurement of the β-hCG level, initial evaluation must include pelvic ultrasonography.
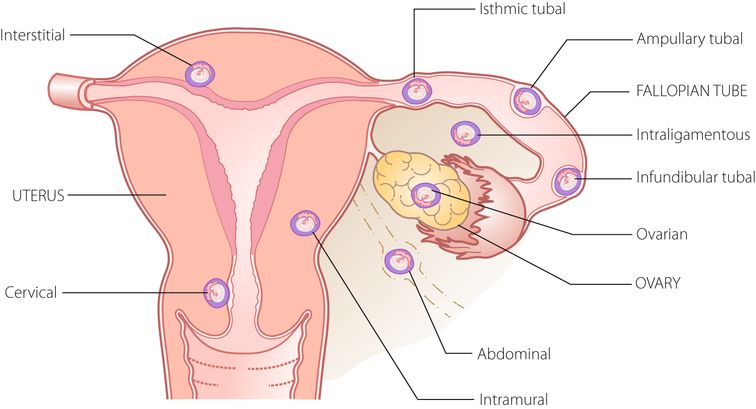
The fallopian tube is the most common location for an ectopic pregnancy (95%).
Within the fallopian tube, the ampulla is the most common site (70–80%).
Unusual sites that are important to consider are the uterine cornua and cervix.
The most common sonographic sign of ectopic pregnancy is the “tubal ring” sign, which is an adnexal mass that does not contain a yolk sac or embryo (seen in 89–100% of ectopic pregnancies). This sign is also highly specific.
An adnexal mass containing a yolk sac or embryo with a heartbeat is less common, but pathognomonic for ectopic pregnancy.
Doppler flow at the periphery of a tubal ring (the “ring of fire” sign) is not specific for ectopic pregnancy and may be seen with physiologic corpus lutea. Corpus lutea are common in normal intrauterine pregnancies. Demonstrating that a non-ovarian adnexal lesion is separable from the ovary on real-time exam with pressure from the ultrasound transducer raises specificity by differentiating it from a primary ovarian mass such as a corpus luteum.
It is important to remember that a positive β-hCG without a detectable intrauterine gestational sac or with a nonspecific-appearing endometrial fluid collection (sometimes referred to as a “pseudo-gestational sac”) does not equate to ectopic pregnancy.
If the patient is clinically stable, a follow-up study should be scheduled in 3–7 days (depending on the clinical setting), as these findings may be seen in early intrauterine pregnancies.
If the radiologist is not mindful of this consideration, some patients may be treated with methotrexate with resultant loss of desired pregnancy at this stage.
Following treatment with methotrexate, falling ß-hCG is a more accurate indicator of treatment success in ectopic pregnancy than ultrasound appearance.
An ectopic pregnancy successfully treated with methotrexate may initially increase in size and even vascularity before involuting.
Self-assessment
|
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








