24 Head and Neck–Related Incidental Findings
24.1 Parotid Mass
24.1.1 Case Presentation
History
A 44-year-old man presents with hoarseness. A CT scan of the neck with contrast was performed.
Imaging Findings and Impression
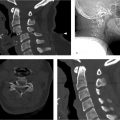
Axial contrast-enhanced CT images of the neck shows a well-circumscribed mass in the superficial lobe of the right parotid gland (arrow in ▶ Fig. 24.1a). There is an area of calcification within the mass (arrow in ▶ Fig. 24.1b). There is no evidence of infiltration into the superficial or deep soft tissues. This is a solitary, solid mass in the parotid gland. The differential diagnosis is given below; however, clinical evaluation by an otolaryngologist will be needed to make the definitive tissue diagnosis.

24.1.2 Clinical Evaluation
History
A 44-year-old man presents to otolaryngology clinic for evaluation of hoarseness. An incidental parotid mass is identified on neck CT with contrast. He denies any recent illness, pain, or swelling in the region of the parotid gland.
Physical Examination
A small, firm mass detected in the right parotid gland was nontender and slightly mobile. There was no adenopathy or overlying skin lesions. Sensation was intact and there was no evidence of trismus or facial nerve palsy. Examination of the airway revealed an incidental polyp of the right vocal cord.
Impression
Incidentally detected solid mass of the superficial lobe of the right parotid gland.
Management
Fine needle aspirate was performed and pathology suggested acinic cell carcinoma. Superficial parotidectomy with identification and preservation of the facial nerve was performed. Clear margins were reported by the pathologist and the patient was referred to a head and neck surveillance clinic for monitoring.
24.1.3 Differential Diagnosis
Parotid acinic cell carcinoma:
The majority arise in the parotid gland.
A rare, slow-growing variant of adenocarcinoma.
On CT, it is well defined, usually homogenously enhancing, and may have cystic areas.
Important to evaluate for extent of tumor and CN VII perineural invasion.
Parotid benign mixed tumor (pleomorphic adenoma):
Most common benign parotid neoplasm.
Most often demonstrates homogeneous enhancement with contrast.
Well defined, typically marked T2 hyperintense on MRI.
Calcifications may be present.
Warthin’s tumor (lymphomatous papillary cystadenomas):
Second most common benign parotid tumor.
Most common cause of bilateral or multifocal solid parotid masses.
Propensity to be located within the parotid tail.
Mural nodule in a cyst is a common appearance.
Calcification is rare.
Usually does not enhance with contrast.
Low incidence of malignant transformation.
Tumor of the elderly with a male predominance. Extremely rare in patients younger than 40 years.
A Warthin Tumor Score, which incorporated low mean and standard deviation ADC in addition to age older than 49 years and male sex, has been found to have a 100% specificity and 85.7% sensitivity for distinguishing Warthin’s tumor from pleomorphic adenomas and carcinomas.
Mucoepidermoid carcinoma:
Most common malignant parotid neoplasm.
Imaging appearance depends upon the tumor grade:
Low-grade tumors: similar to benign mixed tumors, well defined, T2 hyperintense.
High-grade tumors: poorly defined margins, low signal intensity on T2-weighted imaging.
Adenoid cystic carcinoma:
Most common malignancy involving the MINOR salivary glands but relatively rare in the parotid gland.
Locally aggressive tumor with tendency for perineural spread, local infiltration, recurrence postresection, and distant, late metastasis.
24.1.4 Clinical and Diagnostic Imaging Pearls and Pitfalls
CT is the imaging modality of choice to evaluate extent of lesion within the gland and to evaluate for cervical adenopathy
MRI is superior for evaluation of perineural tumor spread.
In the absence of infiltrating tumor or perineural tumor spread, imaging alone lacks the specificity to differentiate malignant tumors from benign etiologies.
Tissue diagnoses remain the standard of care for most parotid lesions.
Clinical findings that suggest malignancy include the following:
Lymphadenopathy.
Rapid increase in size.
History of new onset of pain.
24.1.5 Essential Facts
Nonspecific imaging appearance. Tissue diagnosis is required.
Considered a low-grade malignancy.
Good prognosis with surgical resection alone.
Post-op XRT (radiotherapy) is performed if there is concern for margins or perineural invasion.
Poorer prognosis if perineural or vascular invasion.
24.2 Thyroglossal Duct Cyst
24.2.1 Case Presentation
History
A 69-year-old woman presents with neck pain. A CT scan of the neck without contrast was performed.
Imaging Findings and Impression
CT of the cervical spine without contrast shows a well-circumscribed, lobular hypodense mass in the right paramidline anterior infrahyoid neck (arrows in ▶ Fig. 24.2a–c). The mass is embedded with the strap muscles (arrowheads in ▶ Fig. 24.2b). There is no solid nodule associated with the hypodense mass. This is an incidentally detected cystic, midline mass with no evidence of inflammation about the cyst or solid component. It most likely is an uncomplicated thyroglossal duct cyst (TDC).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree