42 MRI Patient-Related Motion Artifacts
42.1 Cerebrospinal Fluid Flow Artifacts
42.1.1 Case Presentation
Clinical History
A 50-year-old woman complains of mid-lower back pain. Her physical examination is normal.
Imaging Findings and Impression
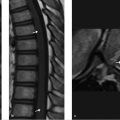
There is a linear area of increased signal within the spinal cord on the short tau inversion recovery (STIR) sequence (white arrows in ▶ Fig. 42.1a) that is not present on neither the sagittal (▶ Fig. 42.1b) nor axial (▶ Fig. 42.1c) fast spin echo (FSE) T2-wegihted images (T2WIs). This hyperintense central cord signal on the STIR image extends the entire length of the cord, does not taper superiorly, and does not expand the spinal cord.
In addition, multiple large, noncontiguous areas of decreased signal are seen in the CSF dorsal to the spinal cord on both the sagittal STIR (blue arrows;▶ Fig. 42.1a) and FSE-T2WIs (blue arrows;▶ Fig. 42.1b). Incidental note is made of a hemangioma in the body of L1 (asterisk in ▶ Fig. 42.1b).
Cause: Areas of decreased signal in the cerebrospinal fluid (CSF) are dorsal to the thoracic spinal cord in an area well known to experience turbulent CSF flow. Areas of signal loss in the CSF are bulky and noncontiguous rather than serpentine and are not closely applied to the pial surface of the cord. The linear area of increased signal seen within the spinal cord on the STIR sequence is not present in neither the sagittal FSE-T2WI nor the axial T2WI.
Diagnosis: These findings are artifactual and the spinal cord and canal are normal.
42.1.2 Differential Diagnosis
Normal thoracic spine MR: Artifactual increased signal in spinal cord due to Gibbs’ truncation artifact (TA) and artifactual decreased signal in CSF dorsal to thoracic cord due to turbulent CSF signal dephasing.
Dural arteriovenous fistula (DAVF) with diffuse spinal cord edema: Linear, serpentine flow voids are closely applied to the pial surface of the spinal cord. Central area of increased signal in the spinal cord tapers superiorly and appears “cigar-like.”
Spinal cord infarction: Hyperacutely, despite even a severe clinical presentation of acute onset of back pain and paraplegia, the spinal cord may appear normal on T1 W and T2WIs but will have increased signal on diffusion-weighted images centrally by 8 to 12 hours. By 1 to 2 days, hyperintensity is seen centrally and affecting the anterior two-thirds of the spinal cord, usually in the thoracic region. By 1 week, the diffusion-weighted images will appear normal. 1
Persistent central canal: Normal finding often demonstrated on high-resolution MRI. This finding is present more often in younger patients. It appears as a linear area of hyperintensity on the T2 W sagittal images located precisely between the anterior one-third and posterior two-thirds of the spinal cord in the cervical and higher thoracic regions, moving more centrally nearer to the conus. 2 On axial images, it should be perfectly round and measure ≤ 2 mm (reported range 1–5 mm). 3 The surrounding spinal cord should be normal in course, caliber, and signal intensity. A symptomatic persistent central canal is a diagnosis of exclusion.
Thoracic cord syringohydromyelia: Although the cavity will follow CSF in signal intensity, it is often more irregular in contour and larger than a simple persistent central canal. Contrast-enhanced MRI should be performed as some syrinxes are tumor associated. The posterior fossa should be examined for a Chiari malformation and the distal aspect of the cord should be examined to exclude the possibility of a tethered spinal cord associated with hydromyelia. In any patient with a possible syrinx, clinical correlation is very important to determine if they are symptomatic. 3
42.1.3 Differential Diagnostic Pearls and Pitfalls
Note if the area of decreased signal is bulky and noncontiguous in a region highly prone to turbulent CSF flow, that is, the dorsal thoracic region. These observations support artifactual flow-related CSF signal dephasing.
Linear, serpentine, and contiguous flow voids, closely applied to the spinal cord, are more suspicious. Contrast enhancement is recommended for further evaluation.
The gold standard test is spinal angiography, which may be required for confirmation and possible treatment in the cases in which a DAVF is suspected clinically.
42.1.4 Artifact Problem-Solving: Additional Evaluation Recommended in Difficult Cases
Possible signal abnormality in the spinal cord:
Recommended: Evaluate cord signal on the axial T2WIs as no abnormal signal will be present if due to the Gibbs TA.
Recommended: If high signal is seen within the spinal cord on the STIR sequence, compare to the higher resolution sagittal FSE-T2WI as higher resolution sequences are much less prone to TAs. 4
Recommended: Increasing resolution and decreasing field of view (FOV) will reduce Gibbs TA. 4
Possibly recommended: Contrast-enhanced (CE) T1WI, CE-MRA and volumetric FSE-T2 W or steady-state gradient recalled echo (GRE) type sequences in the cases in which DAVF cannot be excluded as either there is true edema in the cord and the linear flow void areas are more serpentine and contiguous or clinical suspicion is high.
Possible abnormal flow voids versus CSF turbulent dephasing:
Recommended: If linear, serpentine, and contiguous flow voids, closely applied to the spinal cord, the finding is more suspicious and contrast-enhanced T1 W sequence is recommended to evaluate for possible DAVF. Prior to obtaining the postgadolinium T1 W sequence, a dynamic, contrast-enhanced 3D MRA could also be acquired. 4 , 5
Recommended: A number of sequences are not as degraded by turbulent CSF flow artifacts as axial 2D FSE-T2 W imaging. GRE pulse sequences, which create images by gradient reversal rather than slice-selective radiofrequency (RF) pulse, are not affected by CSF flow artifacts. CSF should remain uniformly high in signal if normal. Volumetric (3D) heavily T2 W FSE type sequences also show much higher, uniform CSF signal that may assist in localizing the most likely site of a spinal DAVF. 6 Balanced steady-state GRE-type MRI sequences provide uniform, high signal within the CSF without signal loss due to turbulent dephasing. 4 , 7
Possibly recommended: The gold standard test to evaluate for DAVF is spinal angiography, which may be required for confirmation and possible treatment in the cases in which a DAVF is suspected clinically and routine MR imaging is highly suspicious. 8
42.1.5 Essential Information:
Artifacts produced by CSF flow:
FSE-T2 W and other spin echo–type sequences utilize a series of slice-selective RF pulses to create the image. Any substance moving through the imaging plane may lose signal due to flow-related dephasing as, although it may be “in plane” for the initial RF pulse, it has moved in location during the subsequent RF-refocusing pulse(s). This is why normal-flowing blood moving through the plane of imaging appears black. 4
GRE imaging sequences create images by gradient reversal rather than slice-selective RF pulses and are therefore not affected by CSF flow artifacts as signal is rephased by gradient reversal that is not slice selective. Therefore, this also explains why normal-flowing blood appears bright on GRE images. 4
Tarlov’s cysts and intrathecal arachnoid cysts may appear “brighter” than the normal CSF on FSE-T2WIs within the thecal sac as the fluid within them is relatively stagnant. There is always some signal loss in CSF within the normal thecal sac due to normal pulsatile motion of the fluid.
In an area of relative narrowing of the spinal canal dimensions, CSF may lose signal immediately distal to the constriction as its flow accelerates and there is increased turbulent dephasing. This phenomenon accounts for CSF flow-related signal loss in the fourth ventricle just inferior to the cerebral aqueduct on sagittal T2WI of the posterior fossa as well as triangular areas of signal loss in the CSF in the lateral recesses of the cervical spine on axial FSE-T2WIs.
The Gibbs truncation artifact:
Pitfall: On spine images, it may create a false appearance of abnormal signal throughout the spinal cord, a pseudosyrinx.
Appearance: Series of alternating high- and low-signal lines present within the image that are parallel to an area of normal anatomy that has an abrupt high-signal/low-signal interface. The artifact is most commonly seen on STIR images, which always have low signal-to-noise ratio because of suppression of virtually all signal except that which is coming from CSF (i.e., the bone marrow and subcutaneous fat signal that contributes to overall signal of the image has been completely suppressed). Lower field strength magnets will often make the situation even worse as they have inherently lower signal than high field strength magnets. Therefore, the low field strength magnet imaging protocols often employ a low matrix and low bandwidth to try and increase the signal-to-noise ratio on STIR imaging. Low matrix means that high-frequency information is not being collected, which is the source of the Gibbs TA.
Typical locations: Inner table of the skull and CSF interface. Spinal cord and CSF interface.
Cause: Abrupt transition from very high to very low signal over a very short distance is high-frequency information that must be collected during the MR imaging process in order to be accurately represented. In low-resolution imaging (the matrix is small and/or FOV is large), the collection of high-frequency data is much reduced. The data acquisition is basically “truncated,” which results in the Gibbs TA, a periodic overshoot–undershoot in signal intensity immediately adjacent and parallel to a high-signal/low-signal interface. 4
42.1.6 Companion Case
A 55-year-old man complains of progressive lower extremity weakness and now has trouble climbing stairs.
Imaging Findings and Impression
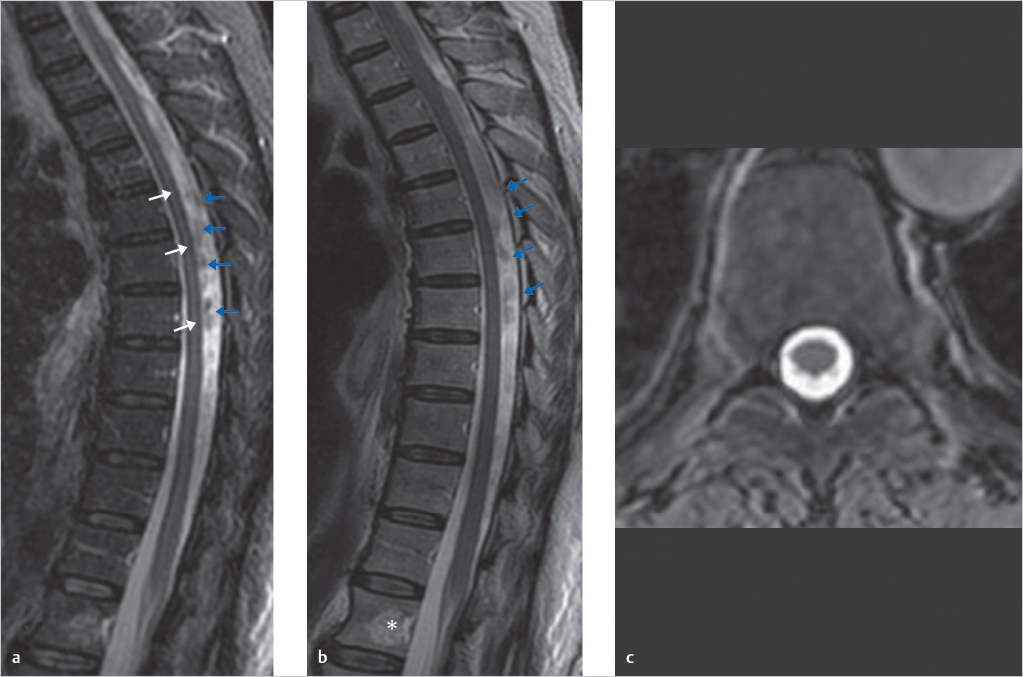
Numerous flow voids are present that appear punctate and serpentine and are closely applied to the pial surface of the spinal cord. The post contrast image (▶ Fig. 42.2b) shows abnormal enhancement of vessels that extend along the entire extent of the visualized spinal cord.

The T2WIs show edema centrally within the spinal cord and mild expansion of the cord in the second patient (▶ Fig. 42.2c). The edema, however, tapers superiorly and does not extend the entire length of the cord.
The following findings prove that this is a real abnormality rather than the Gibbs TA: lack of involvement of the entire spinal cord; no adjacent, alternating lines of high and low signal; tapering of the abnormal signal within the cord superiorly; subtle expansion of the spinal cord; association of the edema with abnormal flow voids in the subarachnoid space.
Furthermore, the patient had symptoms related to venous congestion and edema in the spinal cord, which are clearly not incidental findings.
Diagnosis: Spinal cord edema due to a DAVF.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree