44 MRI Technical and Sequence-Specific Artifacts
44.1 Pulse Sequence–Specific Artifacts: FLAIR
44.1.1 Case 1 Presentation
Lack of cerebrospinal fluid (CSF) suppression on fluid-attenuated inversion recovery (FLAIR) mimicking subarachnoid space abnormality (hemorrhage, meningitis, mass).
44.1.2 Imaging Findings
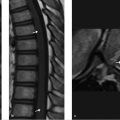
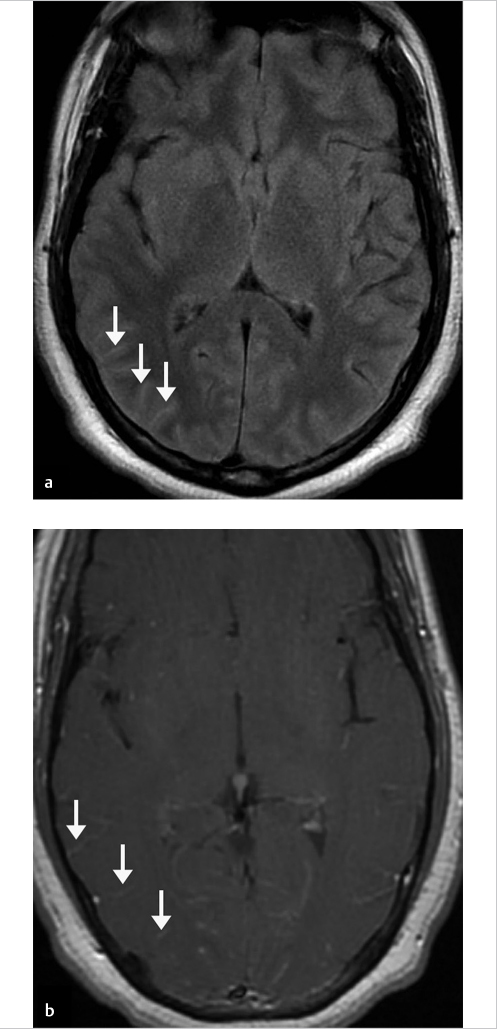
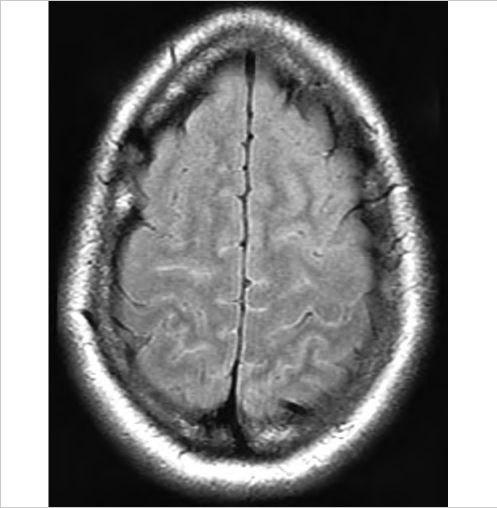
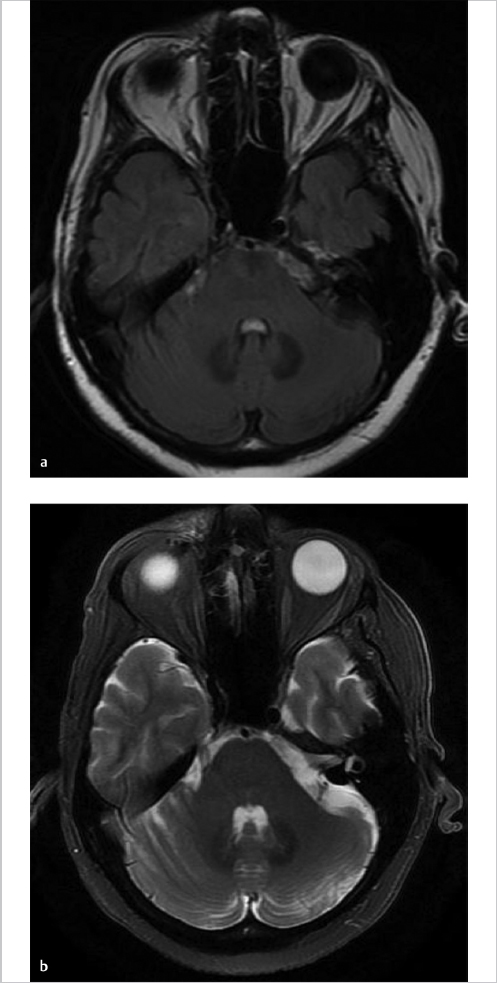
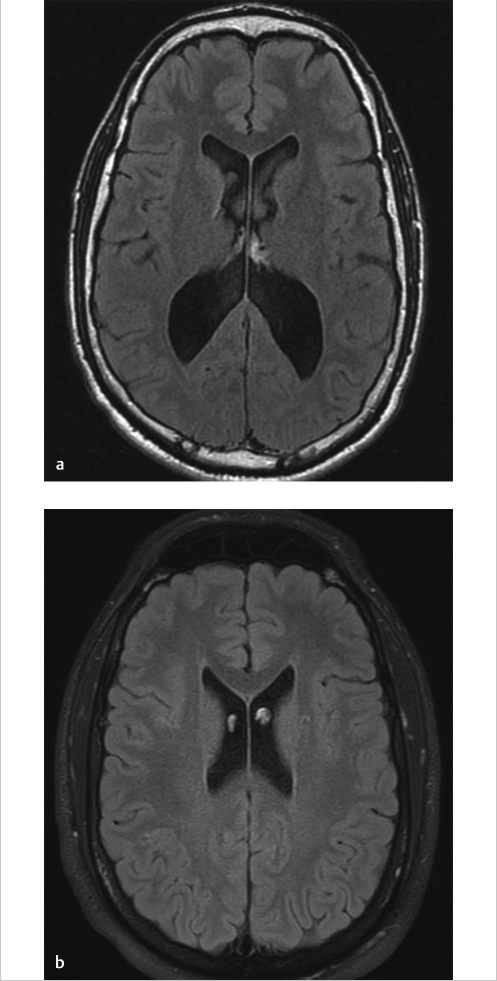
Axial FLAIR image (▶ Fig. 44.1a) through the posterior fossa reveals increased signal in the CSF of the prepontine cistern, anterior to the cerebellar hemispheres bilaterally and within the fourth ventricle. This CSF hyperintensity results from the incomplete suppression of signal due to the presence of a metallic pellet within the left ethmoid air cells (▶ Fig. 44.1b). Marked signal loss is seen in the immediate vicinity of the pellet due to magnetic susceptibility artifact. The artifact persists well superior to the inciting metallic object and mimics subarachnoid hemorrhage (SAH) in the region of the frontal lobes at the vertex (▶ Fig. 44.1c). Additional images from the patient’s brain MRI are shown in ▶ Fig. 44.2.
Impression: Normal brain MRI. The hyperintense CSF on FLAIR imaging is an artifact created by the presence of a metallic foreign body in the ethmoid sinus.
44.1.3 Differential Diagnosis of Subarachnoid FLAIR Hyperintensity
Artifactual hyperintensity:
Magnetic susceptibility artifact.
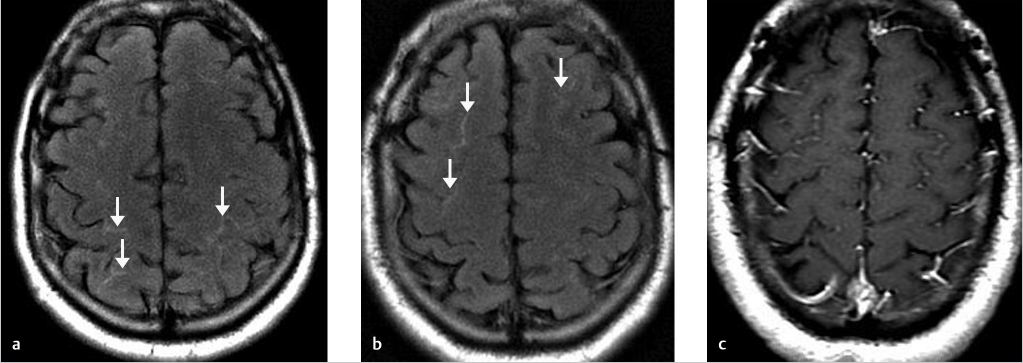
Vascular pulsation or CSF flow artifact: Although this can occur on any pulse sequence, the FLAIR sequence is markedly affected by this artifact especially in the region of the foramen of Monro and in the posterior fossa.
Gadolinium: In renal dysfunction or in cases of delayed imaging after contrast administration in patients who have blood–brain barrier disruption, gadolinium may leak into the CSF space and simulate SAH or meningitis.
One-hundred percent oxygen inhalation, but not found in those receiving 50% oxygen. 2
Moderate to severe motion artifact.
True pathologic causes:
SAH.
Meningitis.
Meningeal carcinomatosis.
Melanocytosis; melanomatosis.
Ruptured dermoid.
Moyamoya disease—“ivy sign.” 3
Acute stroke—pathologic vascular prominence on FLAIR.
44.1.4 Pearls and Pitfalls of FLAIR Imaging
An increase in signal on FLAIR sequences, which is artifactual, will often cross normal anatomic boundaries and fail to have expected associated findings on other sequences.
Increased signal of the CSF on FLAIR that is due to SAH or meningitis is typically very subtle. When it is due to lack of CSF nulling from metal artifact, the signal is most often very hyperintense and involves the entirety of the region affected in a very “nonanatomic” manner.
Examine the entire study for the presence of metallic artifact to see if the increased in CSF signal may be related.
Clinical correlation is very important. Always consider the possibility of a true pathological condition, such as SAH or meningitis, in a patient with a metallic foreign body that may falsely lead one to assume the increased signal on FLAIR imaging is artifactual. Artifacts may conceal real pathology!
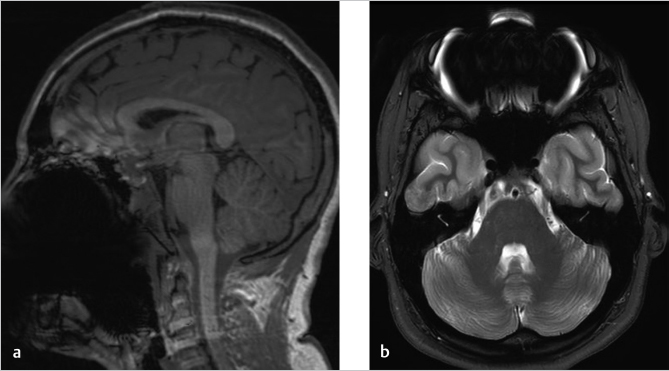
Increased signal of the CSF due to inhalation of 100% oxygen, as often occurs in patients under general anesthesia (GA) for MRI, may result in diffuse increase in CSF signal on FLAIR that is indistinguishable from that due to meningitis or very diffuse SAH. Focal enhancing areas of the leptomeninges or dura and/or loculated CSF collections, cortical edema, and mass effect would obviously suggest an infectious etiology although their absence does not exclude it. Clinical correlation must be made.
Normal pulsatile CSF motion results in lack of its suppression on FLAIR images and resulting areas of increased signal within the CSF. Typical areas affected include the lateral and third ventricles adjacent to the foramen of Monro and the prepontine and ambient cisterns as well as the fourth ventricle.
44.1.5 Essential Facts about FLAIR Imaging
The FLAIR sequence is a heavily T2WI that has an initial inversion recovery pulse to null the CSF signal. 1
Nulling of CSF signal results in increased sensitivity for edema or increased water content in the brain, particularly at CSF interfaces such as the periventricular region and cortex.
However, FLAIR is not used in spine imaging due to excessive CSF pulsatility artifacts.
The inversion time (TI) is defined as the time between the initial 180-degree inversion pulse and the time of the 90-degree RF pulse, which converts any existing longitudinal magnetization into transverse magnetization.
In inversion recovery sequences, the TI is chosen in such a way that any tissue whose longitudinal magnetization is at the null point at the time of the 90-degree RF pulse will not generate any signal, hence fluid signal suppression in FLAIR or fat signal suppression in STIR sequences.
Factors that alter the T1 recovery time of CSF result in lack of its suppression:
Increased protein content in the CSF due to SAH or meningitis, whether carcinomatous or infectious, may decrease the T1 recovery time and result in increased signal on FLAIR.
Substances with a short T1 appear bright on FLAIR, that is, fat and gadolinium enhancement.
Gadolinium results in a shift to the left of the T1 recovery curve for water protons so affected by its presence and therefore generates higher signal on FLAIR images.
Postgadolinium, FLAIR imaging is superior for the detection of meningitis compared with conventional postcontrast T1WIs as there is very little, if any, normal cortical venous enhancement on FLAIR images, which improves confidence that leptomeningeal enhancement is abnormal.
Oxygen is weakly paramagnetic and, therefore, when in high concentration in the subarachnoid space, it may result in shortening of the CSF T1 recovery curve.
The initial inversion pulse is slice selective and therefore frequency specific:
Patient motion or CSF pulsatility between the time of the inversion pulse and the echo acquisition may result in lack of complete CSF suppression.
Magnetic susceptibility artifact creating local magnetic field inhomogeneity results in differences in frequency, which often results in lack of CSF suppression.
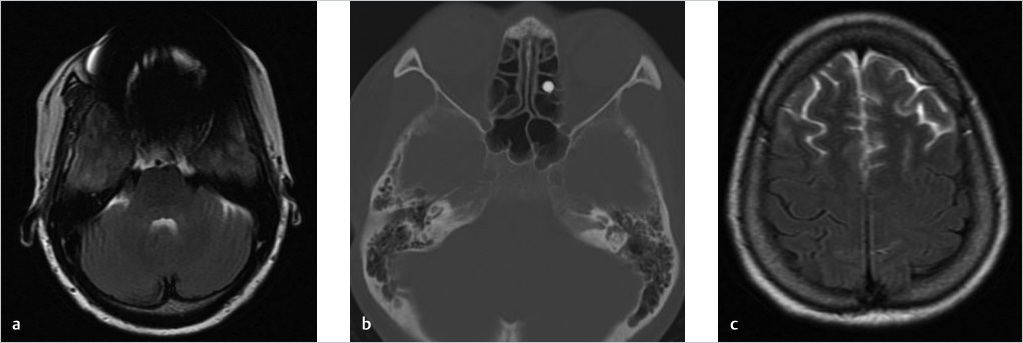
44.1.6 Companion Cases
Companion Case 1: Confirmed Case of Meningitis with Abnormalities on the FLAIR Imaging Sequence
Companion Case 2: Additional Confirmed Case of Meningitis on the FLAIR Imaging Sequence
Companion Case 3: 100% O2 Inhalation
Companion Case 4: CSF Pulsation on FLAIR Results in the Artifactual Appearance of a Lesion or Hemorrhage in the Posterior Fossa Subarachnoid Space
Companion Case 5: CSF Motion in the Lateral Ventricles on FLAIR Causes Artifactual Appearance of a Mass in the Frontal Horns Near the Foramen of Monro
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree