25 Os Odontoideum
25.1 Introduction
The os odontoideum is a rare abnormality of the odontoid process that may present with neck pain and myelopathy but may also be detected as an incidental finding. In this chapter, the diagnostic workup, as it relates to management of the patient, will be discussed. In addition, the developmental anatomy of the craniocervical junction is presented as it provides the key to understanding the distinction between the os odontoideum and other entities in the differential diagnosis.
25.2 Case Presentation
25.2.1 History and Physical Examination
A 15-year-old boy status post a fall presents to the emergency room (ER) with a deep laceration present on his forehead but does not complain of neck pain. The head CT performed in the ER showed a possible abnormality of the craniocervical junction. Therefore, a cervical spine CT scan was performed. The physical examination was normal and his neck was not tender and had a full range of motion.

25.2.2 Imaging Findings and Impression
Sagittal reformatted CT image of the upper cervical spine reveals a well-corticated, prominent ossicle (arrow in ▶ Fig. 25.2) separate from and superior to a hypoplastic odontoid whose superior margin is also well corticated. The ossicle lies near the basion but is not fused to it or to the anterior arch of C1. The basion is normal. There is no evidence of soft-tissue swelling. These findings are typical of an os odontoideum.

25.2.3 Additional Imaging to Be Considered for Further Evaluation
Flexion–extension lateral cervical spine radiographs.
Flexion–extension lateral views of the cervical spine are the most important diagnostic test after detection of an os odontoideum. Abnormal motion between C1 and C2 is present in the vast majority of cases imaged (93%). Anterior instability is most common, occurring in 70%, with posterior instability (10%) and both posterior and anterior instability (13%) occurring less commonly. Lack of motion is uncommon and occurs in only 7%. 1 In the majority of cases, the ossicle will move with the anterior arch of C1.
Lateral views in flexion and extension show significant anterior subluxation of C1 and of the ossicle relative to the body of C2 (▶ Fig. 25.3). The space available for the spinal cord between the posterior aspect of the body of C2 and the posterior arch of C1 is less than 13 mm in flexion.
CT of the cervical spine. CT scan of the craniocervical junction is not needed for diagnosis but provides greater anatomic detail especially if the bony anatomy of C1–C2 is obscured on plain films. If surgery is contemplated, CT with multiplanar reconstruction is very helpful to define the bony anatomy. If a C1–C2 fusion is considered, close inspection of the posterior arch of C1 is important to be sure that the arch is not incomplete or assimilated into the skull base.
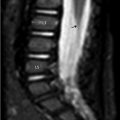
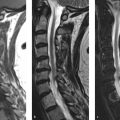
MRI of the cervical spine. MRI may show associated soft-tissue/synovial hypertrophy not detected by plain film. MRI should be performed if there are subtle signs of myelopathy to look for intrinsic increased signal in the spinal cord on the T2-weighted images. An os odontoideum may be associated with an anomalous vertebral artery or persistent fetal circulation; therefore, MRI with or without MRA may be useful if surgery is contemplated. Flexion–extension MRI may be useful as well. Contrast administration for either MRI or CT is not indicated. The sagittal T2-weighted image of the cervical spine (▶ Fig. 25.4) reveals abnormal subluxation of C1 and of the ossicle (asterisk) relative to the base of the dens and the body of C2 as the patient′s neck was in a relatively flexed position for the MRI. There is effacement of CSF signal anterior to the cord at the base of the odontoid, immediately superior to the subdental synchondrosis (SDS; arrow). The space available for cord (SAC, indicated by the thick horizontal white line) measures less than 13 mm. Most commonly, the os will move with the anterior arch of the atlas and SAC will be most compromised in flexion. On plain radiographs, the SAC is measured with a line drawn from the dorsum of the odontoid base/body of C2 to a perpendicular line tangential to the anterior cortical margin of the posterior arch of C1 (vertical thin white line as shown on ▶ Fig. 25.4). On this MRI, upon which these lines have been constructed, it is revealed that ligamentous tissue further decreases the SAC in comparison to that which would be suggested by plain radiographs.


25.3 Clinical Evaluation
This is a 15-year-old adolescent boy with an incidentally detected os odontoideum. There is significant motion of C1 on C2 and the space available for the spinal cord is less than 13 mm at C2, which has been associated with development of myelopathy.
Although the os odontoideum was incidentally detected and asymptomatic, the decision was made to perform C1–C2 posterior fusion (▶ Fig. 25.5) due to the patient’s young age, and significant anterior subluxation and instability on the flexion/extension radiographs.

25.4 Differential Diagnosis
Os odontoideum:
Round or oval, well-corticated ossicle at the skull base between the smoothly corticated but hypoplastic odontoid process and the basion.
Type 2 fracture of odontoid with nonunion (see companion Cases 1 and 2):
The plane of the separation in the os odontoideum is most often well above the superior articulating facets of C2, whereas a type 2 fracture, through the “neck of the odontoid,” often extends below this level. 2
The os odontoideum is round or oval in shape, whereas a type 2 odontoid process fracture fragment has a “peg-shaped” appearance.
Hypertrophy and rounding of the anterior arch of C1 rather than its usual half-moon shape has also been reported in patients with the os odontoideum and may distinguish it from a type 2 fracture fragment. 3
Importantly, in chronic cases, it is often not possible or of importance clinically to distinguish the os odontoideum from a chronic nonunion of an odontoid process fracture as both may have a similar posttraumatic etiology and be functionally equivalent in terms of their potential for C1–C2 instability. 4
Os terminale/os terminale persistens (see companion Cases 3 and 4):
A secondary ossification center, the os terminale (ossiculum terminale of Bergmann) sometimes forms within the distal tip of the dens, an epiphysis called the chondrum terminale. It usually appears by 3 to 6 years of age and unites with the body of the odontoid around 11 to 12 years of age. 5 , 6 , 7 If it does not fuse with the base of the odontoid, and the apicodental synchondrosis (ADS) remains open in the adult, it is termed an os terminale persistens. 5 , 8
An os terminale persistens is readily diagnosed when the ossicle is small, the proximal dens is virtually normal, and, on coronal imaging, the characteristic “V” shape of the unfused ADS is seen.
Importantly, the os terminale with minimal or no odontoid hypoplasia has very little potential for atlantoaxial instability (AAI), unlike a large os odontoideum with significant dens hypoplasia. 1 , 5 , 6
Large os terminale versus small os odontoideum: The distinction between os terminale persistens and os odontoideum is semantic in many cases as a dislocated ossiculum terminale may aberrantly enlarge to “give rise” to an os odontoideum and the proximal dens becomes increasingly hypoplastic over time. 5 , 6 , 9 , 10 , 11 , 12 , 13
Unfused SDS, also known as the dentocentral or lower dental synchondrosis:
The SDS is a wide cartilaginous epiphyseal plate, a remnant of the C1–C2 intervertebral disk, that is visualized in 100% of children ≤ 3 years of age and 50% of children 4 to 5 years of age and therefore may be mistaken for a fracture in children younger than 5 years of age. It may persist as a thin sclerotic line on CT and a dark line on T2 W MR images from 5 to 11 years of age. 7 , 14
The SDS lies well caudal to the plane of the C2 superior articulating facets, deep within the body of C2. 5
An unfused SDS should not show any motion with flexion and extension. 1
In children younger than 7 years of age, the SDS is a site of relative weakness and the most common site of injury. 15 , 16
If there are symptoms or a high clinical suspicion of injury, MRI is useful to look for associated edema in the vertebral body, adjacent to and through the SDS, and within ligaments of the craniocervical junction.
Dystrophic calcification in ligaments due to old injury or arthritis (see companion Case 8):
The odontoid appears to have formed normally but may be sclerotic and/or eroded.
Dystrophic calcifications are not well rounded and corticated and their location is variable.
Calcium pyrophosphate dihydrate crystal deposition disease (CPPD)/“pseudogout”:
Dystrophic calcification and erosion of the odontoid process in patients with “pseudogout.”
It may result in the “crowned dens syndrome” in which soft-tissue calcium deposits occur around the dens and result in neck pain.
Condylus tertius (see companion Case 7):
Rare congenital abnormality that results from lack of integration of embryonic mesenchymal tissue ventral to the notochord. 4 , 17 , 18 , 19 , 20 , 21 , 22 , 23 , 24
It appears as a small midline bony tubercle firmly attached to the basion and is essentially a third occipital condyle that may form a true synovial joint with the anterior arch of C1 and/or the odontoid process and limit the range of motion of the craniocervical junction.
If the odontoid process appears normal and the clivus hypoplastic, or dysmorphic with a comma-shaped basion, the diagnosis of condylus tertius is favored over an os odontoideum that has fused to the skull base (aka os avis). 8 , 17 , 18
25.5 Clinical and Diagnostic Imaging Pearls
Smooth, well-defined cortication of the round-shaped ossicle and the superior margin of the hypoplastic odontoid favor the diagnosis of os odontoideum, orthotopic subtype.
Flexion–extension radiographs are needed as the os odontoideum almost always has some degree of C1–C2 instability that strongly influences the surgeon’s management decision.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree