27 Approach to the Solitary Vertebral Lesion on Magnetic Resonance Imaging
27.1 Introduction
The detection of multiple bone lesions on MRI, in combination with clinical data, most commonly leads to the diagnosis of metastatic disease or multiple myeloma. The evaluation of a solitary bony lesion in the spine may be more challenging and will often require additional diagnostic testing if benign imaging features are not present on MRI. 1 When the vertebral lesion has no benign features, especially in the older adult patient, metastatic disease is always a significant consideration. It is important to realize that the majority of the spine and the entire nonaxial skeleton will not be visualized on a routine lumbar spine MR. Therefore, the incidentally detected, indeterminant “solitary” vertebral lesion may, in fact, be one of multiple lesions. Even in patients with a known primary malignancy, however, the diagnosis is not certain from imaging alone as it has been found that a solitary bone lesion has a 12% chance of being either benign or due to metastatic disease with a different histopathology than the known primary. 2
This section will begin with a case presentation of the most commonly detected incidental bone tumor in the spine, the hemangioma. We will then present a more generalized approach to any solitary, incidentally detected bone lesion on MRI. With increased utilization of spine MRI, it is expected that incidental bone lesions will be frequently detected. It is therefore important to differentiate benign lesions, which need no treatment or follow-up, from those that will require additional evaluation and possibly affect patient management.
27.2 Case Presentation
27.2.1 History and Physical Examination
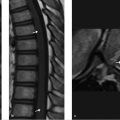
A 30-year-old woman presented with lower back pain at the L5–S1 level for which an LS spine MRI was performed. Her physical examination was normal. A lesion within T12 was incidentally detected.
27.2.2 Imaging Analysis
There is a focal lesion within the T12 vertebral body that is high in signal on both T1WIs and T2WIs (▶ Fig. 27.1). Linear areas of decreased signal are seen within the lesion on the T2WI. The appearance of this lesion is consistent with a typical vertebral hemangioma.

27.3 Recommended Management
A focal, well-defined lesion in the vertebrae that has increased signal on both the T1 W and T2WIs is considered to most likely be a benign hemangioma and no further workup or follow-up imaging is needed.
27.4 Differential Diagnosis for a Focal Vertebral Lesion on MRI That Is Hyperintense T1-Weighted Images
Hemangioma:
The most common benign bone tumor consisting of both vascular and fatty elements the ratio of which determines its signal characteristics. The greater the amount of fat, the more indolent the lesion, the higher the signal on T1WI and the more complete the suppression of signal on fat-suppressed images.
Typical hemangiomas are asymptomatic, incidental, discrete lesions that are high in signal on both T1WIs and T2WIs that most often occur in the vertebral bodies.
Linear areas of decreased signal often seen on the T2WI correspond to coarsened trabeculae.
Most commonly, their signal does not completely suppress on fat-suppressed T2WIs due to the vascular stroma component.
Discrete lesion may be seen on CT with characteristic corduroy pattern.
Focal fatty marrow:
It is commonly seen in adults with patchy, progressive conversion of red to yellow marrow.
It suppresses completely on short tau inversion recovery (STIR) and other fat-suppression sequences.
No discrete lesion is typically seen on CT.
Intraosseous lipomas:
These are benign, rare lesions in the spine.
They are uniformly high in signal on both the T1WIs and fast spin echo (FSE) T2WIs.
Complete signal suppression is found on fat-suppressed sequences.
Discrete low attenuation lesion is seen on CT with no coarsened trabeculae.
Degenerative end plate changes, Modic type II:
Fatty infiltration of the end plates, high in signal on both T1WI and T2WI, adjacent to a degenerative disk.
Signal suppresses completely on fat-suppressed sequences.
Bone infarction:
Geographic area of increased signal intensity on the T1WIs with a rim of marked decreased signal.
The dark rim is surrounded by increased signal on the T2WIs.
Typically found in the watershed zone of vertebral body that has been described as predominantly in the anterior half or in multiple areas near the end plate and/or deep medullary portion of the vertebral body involving several levels. 3
It is often associated with steroid use. Subchondral region of the femoral heads is most often affected and may be seen on scout images of lumbar spine MRI.
Chronic or healing infectious process:
Associated with disk space abnormality and edematous soft-tissue changes.
Metastatic melanoma:
Melanin has increased signal on noncontrast T1WIs.
Hyperintense signal on T1W images from melanoma bone metastases is exceedingly rare.
Hemorrhagic foci appearing as areas of decreased signal on T2WI that bloom on gradient echo (GRE) and susceptibility weighted imaging (SWI) sequences are common.
It is an extremely rare cause of a solitary bone lesion as usually lesions are multiple and the patient, in the vast majority of cases, has a known diagnosis of metastatic melanoma.
27.5 Clinical and Diagnostic Imaging Pearls: An Approach to the Solitary Vertebral Lesion Detected Incidentally on MRI
I. Prime considerations when evaluating the MRI
Signal intensity on T1WIs:
Hyperintense lesions on noncontrast T1WIs are virtually always benign.
High signal on noncontrast T1WIs is most often due to fat.
The most commonly encountered lesions are the typical hemangioma, focal fatty marrow, and degenerative Modic type II end plate changes.
Hypointense lesions on T1WIs that are hyperintense on the fat-suppressed T2WIs are indeterminate on MRI and often need further evaluation. The most commonly encountered lesions are described as follows:
Islands of red marrow are a fairly common benign finding in younger patients but may also occur in times of hematopoietic stress and reconversion of fatty replaced marrow.
Red marrow is lower in signal on T1WIs than surrounding fatty marrow but is typically NOT lower in signal than intervertebral disks or skeletal muscle. On fat-suppressed T2WIs, it is iso- to slightly hyperintense relative to skeletal muscle but should not be extremely bright. 4
The “bull’s eye sign,” focal internal islands of preserved high signal on T1WIs, indicates the lesion is very likely to be benign. 5
MR in-phase/opposed-phase imaging may be very helpful to confirm focal red marrow as a drop in signal on the out-of-phase images by more than 20% is due to the presence of both water and fat signal within the lesion, which suggests a benign lesion as most tumors, with myeloma being the exception, completely displace normal marrow fat. 6 , 7 , 8
Fat content (fat fraction) can also be measured by use of m-Dixon fat suppression techniques and has been shown in some studies to help differentiate focal red marrow from malignant lesions. 9 , 10
Gadolinium contrast enhancement may also be helpful as although red marrow enhances to a greater extent than yellow marrow, marked enhancement is atypical. Normal red marrow on DCE (dynamic contrast-enhanced) MRI time intensity curves (TICs) shows a slow wash-in, low maximal peak, and either minimal or no apparent washout. Pathological marrow enhances much more quickly, reaches a higher absolute level, and shows significant contrast washout. Morales et al found that a high K-trans and, most importantly, higher plasma volume was indicative of metastatic disease rather than atypical hemangiomata as these parameters reflect the increase vascular permeability and increase in number of immature vessels in neoangiogenesis, the hallmark of neoplastic lesions. 11
Atypical hemangioma:
Low signal on T1WIs but high in signal on T2WIs. Confirmation with CT revealing typical, coarsened trabecula is diagnostic. If the lesion is indeterminate on MRI and CT, and there is no known primary malignancy, FDG-PET/CT is useful as atypical hemangioma do not have increased uptake.
Hematological malignancies:
Signal intensity is often much lower than intervertebral disks and skeletal muscle on T1WIs and markedly increased on fat-suppressed T2WIs.
Metastatic disease:
Lytic metastases most often appear as well-defined, focal areas of decreased signal on the T1WIs with increased signal on T2WIs.
Hypointense lesions on both T1WIs and fat-suppressed T2WIs are less common and further workup is sometimes required (also see ▶ Table 27.1). The most common lesions are as follows:
Modic type III (fibrosis) degenerative change. Linear area of decreased signal on T1 W and T2WIs associated with degenerative intervertebral disk disease.
Bone island (enostosis). Island of dense cortical bone within cancellous bone that is markedly dense (mean ≥ 885 HU and maximum ≥ 1,060 HU) and often oval in shape with a spiculated border. 12 A cold bone scan is helpful in distinguishing bone island from an osteoblastic metastasis, whereas increased focal uptake within the solitary lesion is not of assistance, as a bone island may have increased activity.
Osteoblastic metastatic disease. Less dense than bone island, round shape, and halo of increased signal on T2WIs surrounding the low signal lesion is highly suggestive of metastatic disease. 5
Patient’s age:
The vast majority of malignant lesions in the adult spine are due to metastatic disease and multiple myeloma/plasmacytoma rather than primary bone tumors, which are rare.
In patients older than 40 years of age, the majority of metastases to vertebrae are due to breast, lung, prostate, kidney, and thyroid primary cancers, all of which are extremely rare in children.
Breast and prostate cancers have a very high propensity to develop skeletal metastatic disease.
In children and young adults, eosinophilic granuloma (EG), the solitary bone involvement form of Langerhans cell histiocytosis (LCH), and osteoid osteomas may present as an incidental finding but when discovered in the spine, the majority manifest with complaints of back or neck pain and therefore would seldom be incidentally detected, asymptomatic lesions.

Location of the lesion, whether centered in the vertebral body versus the posterior elements, may provide guidance as to the most likely diagnosis:
Vertebral body:
Areas of focal red marrow.
Intervertebral degenerative disk disease related or Schmorl’s node.
Hemangioma.
Metastatic disease.
Plasmacytoma/multiple myeloma.
Bone island.
Intraosseous lipoma.
Benign notochordal cell tumor.
Paget’s disease.
Chordoma.
Leukemia/lymphoma.
Giant cell tumor.
Osteosarcoma.
LCH.
Infection.
Fibrous dysplasia.
Posterior elements: Lesions arising in the posterior elements are more likely to be primary bone tumors.
Osteochondroma.
Osteoid osteoma.
Osteoblastoma.
ABC.
Osteosarcoma.
Chondroblastoma.
Chondrosarcoma.
Continuity with a severely degenerative disk and irregular vertebral end plates:
Degenerative end plate changes have been characterized into three types based on MRI appearance that relates to their chronicity by Modic et al 13 :
Modic type I is consistent with more acute edematous change and is T1 signal hypointense and T2 signal hyperintense. Focal enhancement is often present.
Modic type II is consistent with more chronic change and fatty infiltration and is therefore hyperintense on both T1 and FSE-T2 sequences.
Modic type III represents chronic degenerative, sclerotic reaction and is therefore hypointense on both T1 W and T2WIs.
Although rarely an incidental finding, infectious spondylitis should also be considered in the differential diagnosis of edematous end plates adjacent to an abnormal disk space and additional clinical correlation sought. Extensive enhancement of end plates, disk space, and especially the paravertebral soft tissues may occur in advanced degenerative change but is worrisome for infection so that clinical correlation and laboratory testing for infection, erythrocyte sedimentation rate (ESR), and C-reactive protein is indicated.
A Schmorl node, which is a herniation of the disk through a weakened area in the vertebral end plate, often presents as an incidental finding, although it may be a cause of pain acutely. Identification of an end plate defect adjacent to the area of marrow signal abnormality is helpful in making this diagnosis. Contrast enhancement is typical.
II. Additional diagnostic testing modalities to be considered if typical benign imaging features on MRI are not present and the lesion appears to be solitary (further testing and clinical correlation will be necessary)
CT scan of the vertebral lesion is recommended to determine if the lesion is lytic or sclerotic. Practically speaking, although conventional radiographs are very helpful for assessing ribs, long bones, and the skull, they most often lack sufficient sensitivity to assist in the diagnostic workup of an indeterminate vertebral lesion detected on MRI:
Lytic lesion. The most common tumors producing lytic lesions are as follows:
Multiple myeloma/plasmacytoma.
Non–small cell lung cancer.
Renal cell cancer.
Thyroid carcinomas (except medullary thyroid carcinoma, which is typically sclerotic or mixed).
Head and neck cancers.
Melanoma
Sclerotic/osteoblastic lesion. The most common primary tumors producing osteoblastic lesions or mixed sclerotic/lytic lesions are the following:
Prostate cancer.
Carcinoid.
Transitional cell cancer.
Breast cancer (mixed lytic/sclerotic appearance).
GI primaries.
Medullary thyroid carcinoma.
Thorough clinical evaluation is extremely important to guide further workup as the diagnostic performance of imaging tests depends largely upon the primary malignancy:
Metastatic lesions and multiple myeloma represent the majority of malignant tumors of the adult spine. Primary bone tumors are rare. A complete blood count, urinalysis, basic serum chemistries, as well as serum-free light chains, serum, and urine protein electrophoresis to evaluate for the possibility of multiple myeloma should be performed. 14 In women, routine gynecologist’s evaluation with pelvic examination and mammography are recommended. In men, a routine clinical prostate examination and serum prostate-specific antigen (PSA) level are recommended.
In the cases in which the lesion appears lytic with no bony reaction present, FDG-PET/CT is frequently recommended not only to identify the primary but also to provide TNM staging and hopefully identify additional lesions that may be in a location more amendable to biopsy than the spine. Two of the most common primary malignancies to result in lytic metastases are lung cancer and renal cell carcinoma. Currently, FDG-PET/CT is the staging test of choice for lung cancer. For renal cell carcinoma, however, FDG-PET/CT has decreased sensitivity due to normal uptake and excretion of the radiotracer by the kidneys. Therefore, a chest, abdomen, and pelvis CT scan is the superior test to evaluate the kidneys and provide TNM staging. Bone scan is not recommended due to its decreased sensitivity for highly aggressive, purely lytic tumors.
If plasmacytoma/multiple myeloma is suspected (i.e., urine protein electrophoresis [UPEP] or serum protein electrophoresis [SPEP] positive, or hypercalcemia, anemia, or renal failure in the older adult), then whole body MRI (WB-MRI) is recommended. If WB-MRI is not available, skeletal survey plus FDG-PET/CT may be utilized. MRI has the highest sensitivity for infiltration of the marrow by myeloma cells before cortical destruction occurs. The Myeloma working group recommended that patients with smoldering or asymptomatic myeloma undergo WB-MRI (or spine and pelvic MRI if WB-MRI is not available) and that the finding of more than one focal lesion of a diameter greater than 5 mm is definitional for symptomatic disease that requires therapy. In the cases of equivocal small lesions, a second MRI should be performed after 3 to 6 months, and if there is progression on MRI, the patient should be treated as having symptomatic myeloma. 15 Bone scan is not appropriate as it is very insensitive for myeloma. For many years, skeletal survey plain radiographs have been part of the standard workup in patients suspected of having multiple myeloma. Low-dose whole body CT and MRI have been proposed as alternatives to the skeletal survey as they are reported to provide higher sensitivity. 16 However, these techniques have not replaced the plain radiograph skeletal survey in many tertiary cancer centers and are more expensive and time-consuming.
For rare, primary bone tumors, analysis for presence and type of tumor matrix is very important:
Osteoid matrix is cloudlike and may be seen in osteoid osteomas, osteoblastomas, and osteosarcomas. Osteoid osteomas and osteoblastomas occur most frequently in the posterior elements.
Diffuse sclerosis is often seen in benign notochord cell tumors (BNCTs). Chordomas may have some internal calcification. Both chordomas and BNCTs occur in the vertebral body.
Chondroid matrix has a classic appearance of rings and arcs of calcification and may be seen in chondrosarcoma, which has a predilection for occurring in the sacrum and posterior elements.
Giant cell tumors lack calcified matrix, occur more frequently in the sacrum and vertebral bodies and often have a partially sclerotic border on CT. They are frequently lower in signal on T2WI than most other tumors in the differential diagnosis, (plasmacytoma, chordoma and metastatic disease) due to the presence of hemosiderin and fibrous tissue.
If the lesion is indeterminate on MR and CT/plain radiographs, there is no demonstrable primary malignancy and evidence of wider spread metastatic disease, UPEP/SPEP and serum-free light chain assay are negative, and there is no increased uptake on FDG-PET/CT (routine bone scan/SPECT if PET not available), then the indeterminate, solitary lesion may be managed conservatively with close follow-up imaging or a biospy ordered depending on the level of concern of the referring physician and patient. In these cases, the diagnosis of “atypical hemangioma” is often suggested by the radiologist. If the lesion has increased uptake on FDG-PET/CT or bone scan/SPECT, biopsy is the next step in evaluation. 14 , 15 , 17
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree