Diagnosis: Testicular torsion
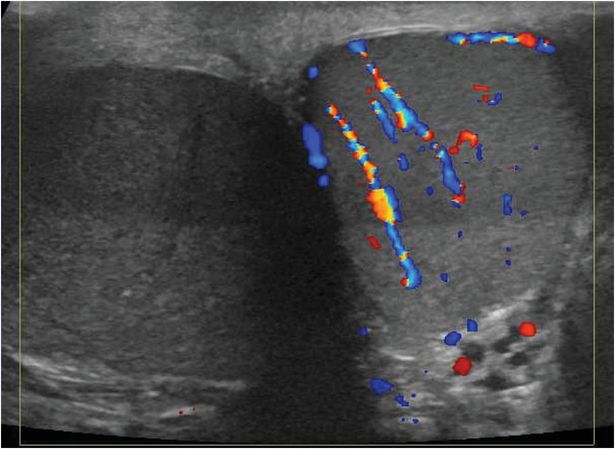
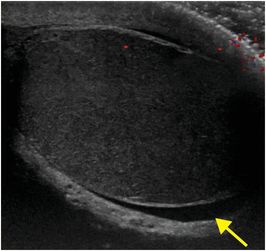
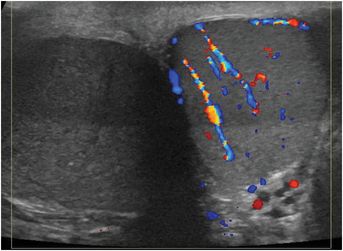
Sagittal grayscale ultrasound image of the right testis (left image) and transverse image of both testes with Doppler overlay (right image) demonstrate diffuse hypoechogenicity of the right testis and no demonstrable blood flow. There is a small, simple, reactive right hydrocele (arrow). The left testis is normal in echotexture, with normal Doppler flow.
Discussion
Testicular torsion most often affects pubescent boys and young adult males.
Typical symptoms include pain that may radiate into the groin and lower abdomen, nausea and vomiting, and swelling of the scrotum.
On physical examination, there is often marked tenderness, and the testis may be oriented in a transverse lie.
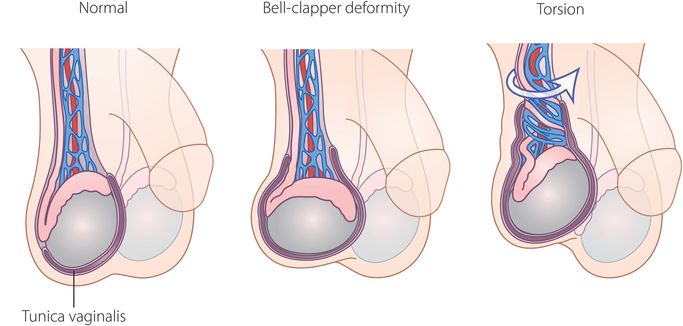
The normal testis is anchored to the wall of the scrotum by a broad posterior attachment that prevents excessive rotation. Testes with “bell clapper” deformity are predisposed to torsion.
The “bell clapper” deformity is a congenital anomaly in which the normal testicular–scrotal attachment is absent, so that the testis is suspended in the scrotal sac by its vascular pedicle.
Forceful contraction of the cremasteric muscles can be the precipitating event in testicular torsion, resulting in elevation and rotation of the testis.
Diagnosis is difficult to make on the basis of grayscale ultrasound alone. In the early stages of torsion, the grayscale appearance of the affected testis is frequently normal. Color Doppler ultrasound with spectral analysis is the most accurate and important imaging modality in the evaluation of testicular torsion.
The normal testis is homogeneously hyperechoic. If the testis appears heterogeneous or hypoechoic on gray scale imaging, it is almost certainly nonviable.
Torsion may also be associated with a small reactive hydrocele and thickening of the scrotal skin.
The most important finding is absence of testicular vascularity. Demonstration of testicular flow does not completely exclude torsion, because some flow can be seen in patients who have incomplete or intermittent torsion (usually in an atypical pattern).
If surgery occurs within six hours of symptom onset, the majority of testes will maintain viability.
With prompt diagnosis and surgical detorsion, there is a good chance that the testis can be salvaged.
If surgery is delayed beyond 24 hours, infarction resulting in irreversible necrosis may occur.
Between 6 and 24 hours after symptom onset, the chance of testicular salvage progressively diminishes.
Clinical synopsis
The patient underwent scrotal exploration with right testicular detorsion. Bilateral orchiopexies were performed.
Self-assessment
|
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








