Diagnosis: Community-acquired pneumonia
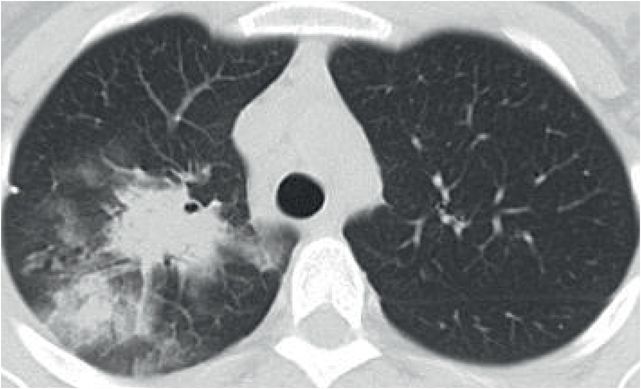
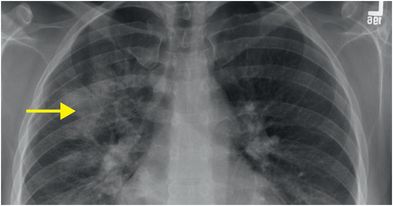
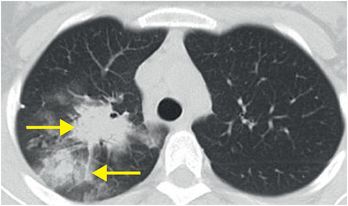
PA chest radiograph (left image) demonstrates a patchy right upper lobe parenchymal opacity (arrow). Unenhanced axial CT confirms two adjacent patchy consolidative opacities in the right upper lobe (arrows), consistent with bronchopneumonia.
Discussion
Overview and classification of pneumonia
Pneumonia is infection of the lung parenchyma. Although pneumonia can be caused by several different viral, bacterial, and fungal pathogens, it is clinically divided into community-acquired pneumonia (CAP) and other types of pneumonia associated with current or recent hospitalization. These include:
Hospital acquired pneumonia (HAP), which is thought to be due to microaspiration of secretions in a hospitalized patient, with high prevalence of antibiotic-resistant gram-positive cocci such as methicillin-resistant Staphylococcus aureus (MRSA) and gram-negative bacilli such as Pseudomonas aeruginosa.
Healthcare-associated pneumonia (HCAP), which is defined as pneumonia in a nursing home resident or a patient with a hospitalization within the past 90 days. The causative pathogens are similar to those that cause HAP.
Ventilator-associated pneumonia (VAP), which occurs within 48 hours of mechanical ventilation.
There are 5.6 million cases of CAP reported each year, with up to 1.1 million hospitalizations and associated health care costs of up to $8 billion.
CAP usually starts as an upper respiratory infection, spreading into the distal airways. There are dozens of microorganisms that can cause CAP; however the most common are Streptococcus pneumoniae, viruses, and atypical bacteria such as Mycoplasma pneumoniae.
Imaging patterns of pneumonia
Pneumonia can present with several different patterns of imaging, which may correlate with the causative organism.
Lobar pneumonia (complete opacification of a single lobe) is typically seen with Streptococcus pneumoniae (pneumococcus) or Klebsiella pneumoniae.
Bronchopneumonia (patchy opacification along the bronchovascular bundle, as in this case) can be seen with atypical organisms, Staphylococcus aureus, viral pneumonia, or Legionella pneumophila.
Interstitial pneumonia (diffuse opacification, often partial, of multiple lobes) can be seen with viral pneumonia, Legionella pneumophila, and Pneumocystis jirovecii pneumonia (previously called Pneumocystis carinii pneumonia, or PCP).
Cavitary pneumonia (pneumonia causing cavitation) can be caused by anaerobic bacteria, Klebsiella pneumoniae, Mycobacterium tuberculosis, Staphylococcus aureus, or fungal pneumonia.
Pneumonia imaging
Chest radiography is the primary modality to evaluate for clinically suspected pneumonia. A chest radiograph can identify the presence, location, and extent of disease, and can also detect some complications, such as cavitation, abscess, pneumothorax, and effusion.
CT is an adjunct to the chest radiograph. CT is used for failed medical treatment or lack of radiographic resolution despite clinical improvement. Also, CT can suggest additional or alternative diagnoses.
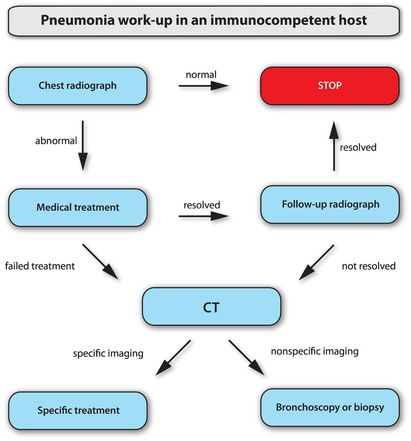
Pneumonia treatment and follow-up algorithm (in an immunocompetent individual)
If the patient does respond clinically to medical treatment, a follow-up radiograph is recommended to ensure resolution.
For a patient < 50 years old, CAP should clear in 3–4 weeks.
For a patient > 50 years old, CAP should clear in 8–12 weeks.
In cases where the clinical or radiographic findings do not respond to medical treatment, a CT should be performed to evaluate for an alternative explanation.
Pneumonia in an immunosuppressed individual
The immunosuppressed host may have altered immunity due to HIV infection, hematological malignancy, transplant, chemotherapy, chronic corticosteroid use, or diabetes.
In addition to the infectious organisms discussed on the previous page, opportunistic fungal and viral infections are common in the immunosuppressed, including Pneumocystis jirovecii and Aspergillus fumigatus. Additionally, reactivation of latent infections such as tuberculosis occurs much more commonly in the immunosuppressed.
If there is high clinical suspicion for pneumonia in an immunosuppressed patient and the chest radiograph is negative, further imaging with CT is often performed.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








