34 Abdominal Aortic Aneurysm
34.1 Case 1
34.1.1 History
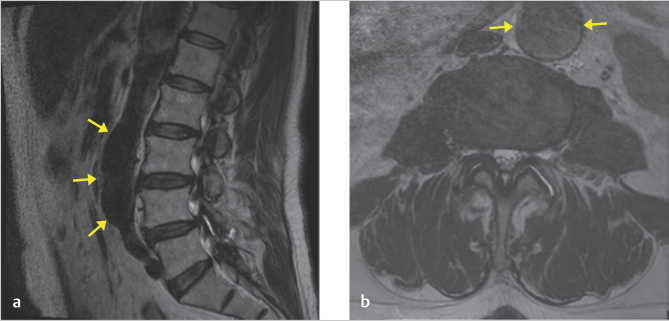
A 75-year-old man presented with a 3-month history of left lower extremity L5 radiculopathy. He had a history of chronic mild lower back pain that had been stable for years. Pulses were equal in his lower extremities. An MRI of the lumbar spine without contrast was performed.
34.1.2 Imaging Findings
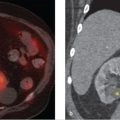
The noncontrast MRI of the lumbar spine reveals a partially visualized fusiform dilation of the abdominal aorta. On axial images (▶ Fig. 34.1b), it measures 3.4 cm in maximal caliber. On sagittal images (▶ Fig. 34.1a), the craniocaudal extent is approximately 8.0 cm.
34.1.3 Impression
An incidentally detected infrarenal abdominal aortic aneurysm (AAA) measuring 3.4 cm.
34.1.4 Additional Testing Needed and Rationale
Follow-up imaging is essential as AAAs have a risk of rupture that increases with caliber size. Further, AAAs are typically asymptomatic and may continue to enlarge without significant symptoms. 1
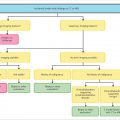
Follow-up imaging time interval: The American College of Radiology (ACR) Incidental Findings Committee II has developed specific recommendations for the imaging follow-up of patients with incidentally detected AAAs.
Modality options for AAA cross-sectional imaging evaluation and follow-up are as follow:
ACR Incidental Findings Committee II does not specifically endorse a modality for follow-up; however, most other recommendations in the past have relied on ultrasound, 2 , 3 , 4 which has near 100% sensitivity and is the least expensive modality.
CT and MR provide the most detail and are most accurate.
If there are any suspicious findings on ultrasound or clinical examination, further characterization may be obtained with a more detailed CT angiogram.
MR angiography may also be considered for more detailed characterization.
34.1.5 Management Decision
In this case, it was recommended to the referring doctor that an abdominal ultrasound to evaluate the infrarenal AAA be performed in 3 years.
34.2 Case 2
34.2.1 History
A 59-year-old man presented with mild, chronic lower back pain that had been stable for several years. The pain was worse in the evenings and improved with rest. Physical examination was within normal limits and lower extremity pulses were equal. An MRI of the lumbar spine without contrast was performed. Images are shown below.
34.2.2 Imaging Findings
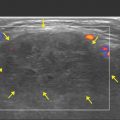
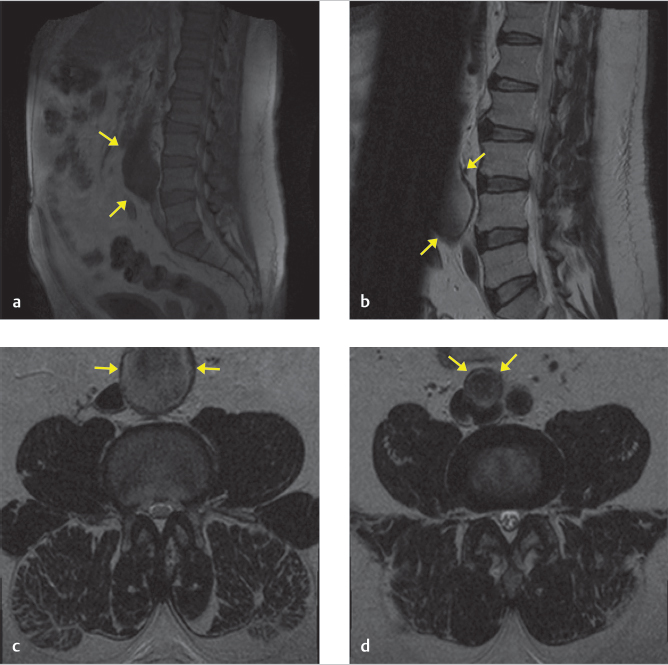
The noncontrast MRI of the lumbar spine reveals a partially visualized fusiform dilation of the abdominal aorta and the right iliac artery. The localization image (▶ Fig. 34.2a) shows the anterior aspect of the aneurysm better than other images, which have saturation bands that partially obscure the aorta (▶ Fig. 34.2b). On axial images, the aneurysm measures 4.6 cm in maximal caliber. On sagittal images, the craniocaudal extent is approximately 7.5 cm. The right iliac artery is 2.5 cm, also dilated (▶ Fig. 34.2d).
34.2.3 Impression
A large, 4.6-cm infrarenal AAA and 2.5-cm right iliac artery aneurysm with uncertain relationship to the patient’s lower back pain. As lower back pain was mild, mechanical in nature, and unchanged in severity for many years, the aneurysm was most likely incidental in nature.
34.2.4 Additional Evaluation Needed and Rationale
Because of the large size, this aneurysm is at a higher risk of rupture, and requires a shorter follow-up (see ▶ Table 34.1). Further, the risk is such that it is prudent to establish a referral with a vascular surgeon, especially with the history of lower back pain.
In addition, this patient also has an incidentally found 2.5-cm right iliac artery aneurysm.
Iliac artery aneurysms are defined as greater than 1.5 times the normal iliac artery diameter or greater than 2.5 cm in diameter.
Follow-up imaging time interval: The ACR Incidental Findings Committee II also has criteria for follow-up of iliac artery aneurysms (▶ Table 34.2).
Iliac artery diameter (cm) | Follow-up interval |
2.5–2.9 | Tend to expand slowly; no specific follow-up interval given |
3.0–3.5 | Initial 6-mo follow-up, then, annual follow-up if unchanged |
> 3.5 | Consider vascular/endovascular therapy |
Source: Adapted from Khosa et al. 2 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree