Diagnosis: Lung cancer
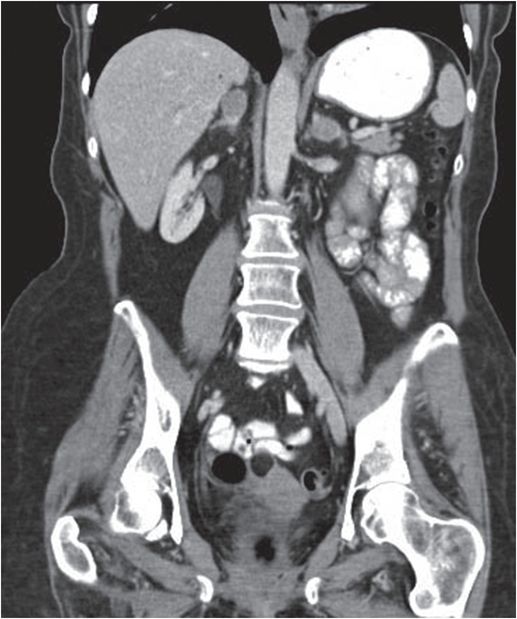
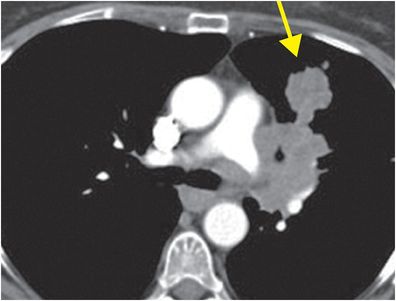
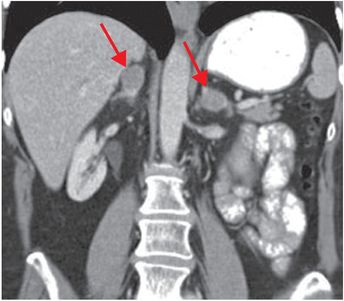
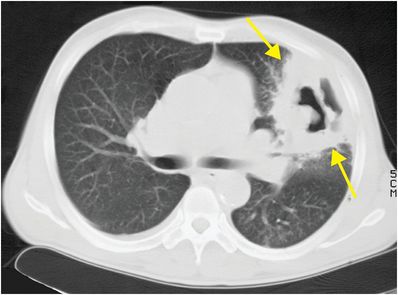
Axial (left image) and coronal (right image) contrast-enhanced CT images show a left upper lobe mass (yellow arrow) with aortopulmonary window and hilar adenopathy, and bilateral adrenal metastases (red arrows). Hoarseness was secondary to recurrent laryngeal nerve involvement. Left phrenic nerve involvement with diaphragmatic paralysis caused dyspnea.
Discussion
Lung cancer is the cancer with highest mortality in the United States, accounting for 33% of cancer deaths in men and 24% of cancer deaths in women. It is only lower in incidence than skin cancer, breast cancer in women, and prostate cancer in men.
5-year survival is better with diagnosis in early stages (14% for all stages with breakdown as follows: stage 1A: 61%, 1B: 38%, 2A: 34%, 2B: 24%, 3A: 13%, 3B: 5% and stage 4: 1%).
70% of patients present with advanced stage cancers.
Primary lung tumors were most recently classified by histologic appearance in the 2004 WHO criteria.
“Non-small-cell lung cancers” as classified as:
Adenocarcinoma
Squamous cell carcinoma
Large cell carcinoma
Small cell carcinoma is considered in a different category given its different histopathological features, prognosis, and treatment considerations.
Lesions classified as “unresectable” by TNM staging are considered so because resection has not been shown to improve survival. These include:
T4 lesions that invade the mediastinum or a vertebral body or manifest as tumor nodules in a separate ipsilateral lung lobe.
N3 lesions (scalene, supraclavicular, or contralateral mediastinal or hilar lymph nodes greater than 1 cm in short axis).
Metastatic lesions in the contralateral lung or distant sites.
Effusions or lesions that may categorize disease as unresectable must be diagnostically sampled.
Metastases are a common differential consideration for primary lung cancer.
Known non-lung primary malignancy and multiple lesions of varying shape and size favor a diagnosis of metastatic disease.
The most common sites to which primary lung cancer metastasizes are the adrenal glands (40%), liver (30%), bones (20%), and brain (10%).
It is important to establish histologic type and tumor receptor status (e.g., presence or absence of epidermal growth factor receptor [EGFR] mutation) to guide treatment choice.
Spectrum of lung cancer
Adenocarcinoma
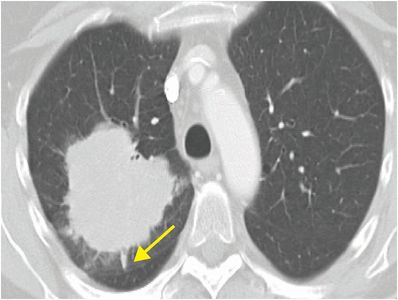
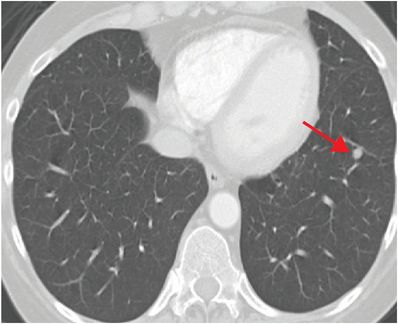
Adenocarcinoma is the most common type of lung cancer. Tumors tend to be peripheral and range from pure ground glass nodules (GGN), to mixed solid–GGN, to solid nodules, with a spectrum of behaviors. The nomenclature of adenocarcinomas was recently refined by histological type. The term “bronchioloalveolar carcinoma” (BAC) is being phased out. The entity previously known as “mucinous BAC” is now known as “invasive mucinous adenocarcinoma”. Pure GGN may represent “pre-invasive” minimally invasive adenocarcinoma or adenocarcinoma in situ, which have 100% disease-free survival when resected. Surveillance over several years may be necessary, as many adenocarcinomas are slow-growing. Increasing solidity, even if the lesion is decreasing in size, is concerning for development of invasive malignancy. Axial contrast-enhanced CT images show an adenocarcinoma as a large, spiculated mass with linear extensions to the pleura (pleural tags; yellow arrow), and a small, contralateral metastasis (red arrow). The presence of contralateral metastasis makes this an unresectable M1 / Stage IV cancer.
Squamous cell carcinoma (SCC)
SCC tends to be a cavitating central (75%) lesion that causes airway obstruction and obstructive atelectasis. Differential diagnosis includes necrotizing pneumonia (including tuberculosis) and pulmonary abscess. Benign infectious and inflammatory lesions tend to have surrounding consolidation and smooth, rather than “shaggy” or “nodular”, internal cavitation. In this case, axial unenhanced CT shows a large, peripheral mass (arrows) with nodular internal cavitation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








