37 Seronegative Spondylarthropathies
Besides rheumatoid arthritis in children and adults, there are a number of seronegative polyarthritic diseases with involvement of the axial skeletonwhose pathogenesis and terminology are still indefinite. Among these are psoriatic arthritis, the Reiter syndrome, ankylosing spondylitis, and enteropathic arthritis. Common characteristics are extraarticular manifestations and specific serological associations. Imaging procedures can be performed on all compartments of the musculoskeletal system and soft tissues to document the extent and distribution pattern of disease. They are, therefore, fundamental not only for differential diagnosis but also for conservative or surgical therapy decisions and follow-up.
Definition
The common term “seronegative spondylarthropathies,” in contrast to rheumatoid arthritis, represents the main group of inflammatory joint diseases with a negative rheumatic factor. The main symptoms are inflammation of the axial skeleton in the form of spondylitis and sacroiliitis, as well as peripheral arthritis, but also enthesiopathies and other extra-articular manifestations. Table 37.1 summarizes the common features and the diagnostic criteria. There is a genetic predisposition and association with the histocompatibility antigen (HLA) B27 ( Table 37.2 ). Transitions from the individual spondylarthropathies entities into classical spondylitis ankylosans and other diseases are possible.
Diagnostic Imaging
Radiography
Regardless of the rheumatoid serology, the joint inflammations can be characterized radiographically by three main phenomena, which unspecifically represent the inflammatory pathomorphological processes of the joint:
Soft-tissue signs of arthritis correspond to the swelling of articular and periarticular tissues, such as the synovium, the joint capsule, and their surroundings. Widening of the joint space caused by effusion or synovitic swelling can be seen in children and also in the hand and finger joints of adults.
Collateral signs of arthritis represent periarticular demineralization of the subchondral and metaphyseal bone. They can be triggered by inflammatory circulatory disturbances, altered osteoblastic function, immobilization, and prostaglandins.
Direct signs of arthritis are direct or indirect results of the destructive effect of inflammatory exudation and proliferation of the synovial membrane on bones and cartilage ( Table 37.3 ).
|
Rheumatoid Arthritis | Seronegative Arthritis | |
Synovial joint involvement: | Generally proliferative | Generally inflammatory |
• Soft-tissue swelling | ++ | ++ |
• Marginal erosions | ++ | ++ |
• Central erosions and cysts | ++ | ++ |
• Osteopenia | ++ | (+) |
• Malalignment/subluxation | ++ | (+) |
• Bony ankylosis | +(generally fibrous) | ++ |
• Bony proliferation | − | +++ |
Tendon and bursa involvement: | ++ | ++ |
• Soft-tissue swelling | ++ | ++ |
• Bony erosions | ++ | ++ |
• Bony proliferation | − | ++ |
Articular cartilage involvement: | + | ++ |
• Bony erosions | + | ++ |
• Bony proliferation | + | ++ |
• Bony ankylosis | + | ++ |
Enthesiopathies: | + | ++ |
• Bony erosions | + | ++ |
• Bony proliferation | + | ++ |
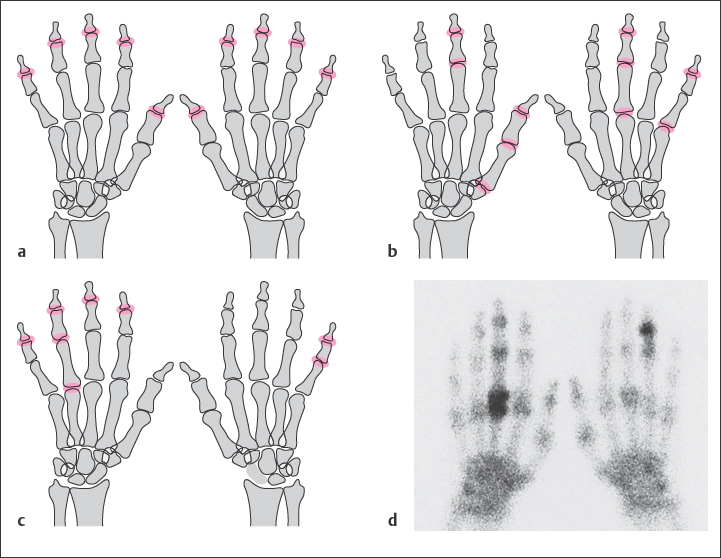
Table 37.4 differentiates seronegative spondylarthritis from rheumatoid arthritis. Four characteristics are useful in the differential diagnosis of seronegative polyarthritis:
Asymmetric distribution pattern
Lack of periarticular osteopenia
Bone proliferation
Bony ankylosis
Nuclear Medicine
Various techniques are available:
Three-phase skeletal scintigraphy with 99mTc phosphonates detects inflammatory soft-tissue reactions and osseous lesions at a very early stage. When several foci are located, the disease pattern can be defined (Fig. 37.1d) Follow-up examinations during therapy are controversial because they often do not provide any additional information to the clinical findings.
Joint scintigraphy with Tc-pertechnetate is rarely indicated. This radiopharmacologic agent accumulates only in the inflamed synovium and synovial fluid. Arthritic manifestation in the hand and fingers can be seen without overlapping, particularly in children.
Inflammation scintigraphy with 99mTc-HMPAO-labeled autologous leukocytes and Tc-nanocolloid, as well as immunoscintigraphy with 99mTc-labeled murine monoclonal granulocytes or human unspecific immunoglobulin, sensitively identify granulocyte-induced inflammations. Aseptic or chronic arthritides are generally not marked.
Ultrasonography
Differentiation between periarticular soft-tissue edema and effusions in joints and tendon sheaths (Chapter 7) can be achieved with a high-frequency probe(7.5 MHz and higher) using a water coupling.
Computed Tomography
In addition to differentiating pathologic soft-tissue swellings, CT imaging can also detect early erosions on the subchondral bone plate. A high-resolution reconstruction algorithm must be used. CT is superior to MRI in visualizing the bone structure. It is recommended to perform axial slices in the carpal area and longitudinal slices in the fingers. Puncture can be accurately guided with CT and ultrasonography (US).
Magnetic Resonance Imaging
MRI is the method of choice to detect the early stages of intra- and extraarticular inflammation and the initial involvement of the bone marrow because of its superior differentiation of soft tissues. It provides a detailed view of the small joints, including cartilage, synovium (pannus), joint capsules, tendons, and bone marrow. Fat-suppressed T2-weighted sequences sensitively record edema in the bone marrow and soft tissues, as well as minimal effusions. Gadolinium dye should always be administered intravenously in patients with arthritic diseases because hyperemic lesions can be clearly detected and localized by their massive enhancement. Coronal slices in T1- and T2-weighted sequences are the procedures for standard orientation.
Disease Entities
Psoriatic Arthritis (Psoriatic Osteoarthropathy)
Pathoanatomy and Clinical Symptoms
In 0.5–25% of cases patients suffering from psoriasis, an independent polyarthritic syndrome develops with primarily erosive joint destruction on the hands and feet, as well as bone proliferation on the limbs and axial skeleton. Histology reveals nonnecrotizing synovitis and inflammatory reactions on the insertions of ligaments and tendons, as well as synchondroses. The coincidence of cutaneous psoriasis and rheumatoid arthritis is possible, when the cutaneous symptoms generally precede the joint complaints. In about 6% of cases, the osteoarthropathy precedes the cutaneous symptoms. They rarely begin simultaneously, and psoriatic arthritis without psoriasis is also rare.
Diagnostic Imaging
Radiography
The characteristic pattern of distribution on the hand ( Table 37.1 ) and the combination of osteoproliferative and osteodestructive lesions ( Table 37.5 , Fig. 37.2 –37.4 and 37.5 ) are useful for differential diagnosis. Involvement of bone sections and soft tissues far from joints leads to the typical appearance of psoriatic dactylitis.
On the foot, psoriatic arthritis is manifested by erosive defects on the interphalangeal and metatarsophalangeal joints, as well as fibro-ostitis on the calcaneus in the insertion of the Achilles tendon and the plantar aponeurosis. A fairly asymmetric sacroiliitis is found in 30–50% of cases. Psoriatic spondylitis is characterized characterized by asymmetric parasyndesmophytes-paradiscal, lumpy new bone formations to be differentiated from the syndesmophytes of ankylosing spondylitis. Involvement of the medium-sized and large joints is rarer and radiomorphologically comparable to rheumatoid arthritis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree