39 Collagenoses
Clinically heterogeneous systemic diseases are included in the term collagenoses, which was coined by Klemperer in 1942. They have in common a generalized inflammatory reaction in the connective tissue with fibrinoid necroses and degeneration, as well as autoantibodies, which will not be further discussed here. Vasculitic diseases can be included in the classic collagenoses due to their clinical and immunological similarities. The following disease entities all affect the joints, and therefore illustrate the overlapping of symptoms within the systemic connective-tissue diseases.
Systemic Lupus Erythematosus (SLE)
Pathoanatomy and Clinical Symptoms
Antinuclear antibodies, among other pathophysiologic processes, lead to immune-complex vasculitis, which has an episodic course and primarily affects women of child-bearing age (female:male ratio = 10:1). A genetic predisposition is assumed because of the DR3 association in 60% of cases. The disease can be triggered by ultraviolet light, viruses, and hormonal changes. Lupus erythematosus is manifested in the skin (butterfly erythema), the musculoskeletal system, internal organs (nephritis, myocarditis, serositis), and the nervous system. In 90% of cases, there are arthralgias, which predominantly affect the joints of the hands and the knees with symmetric soft-tissue swelling.
Radiography
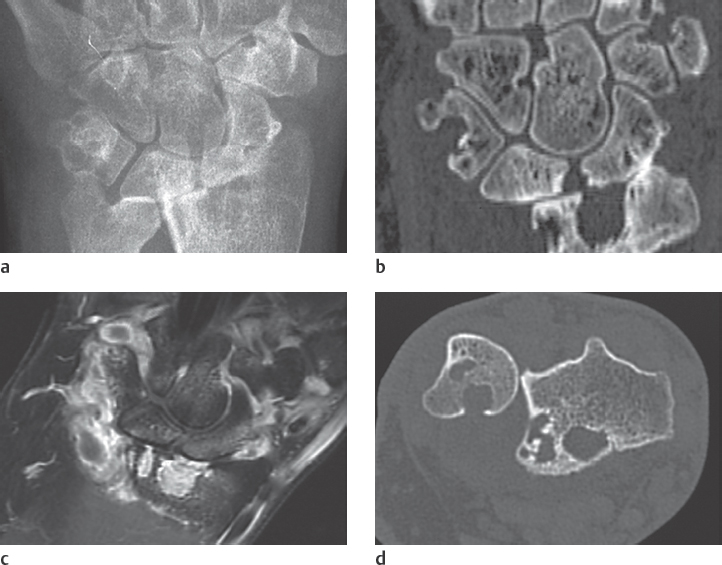
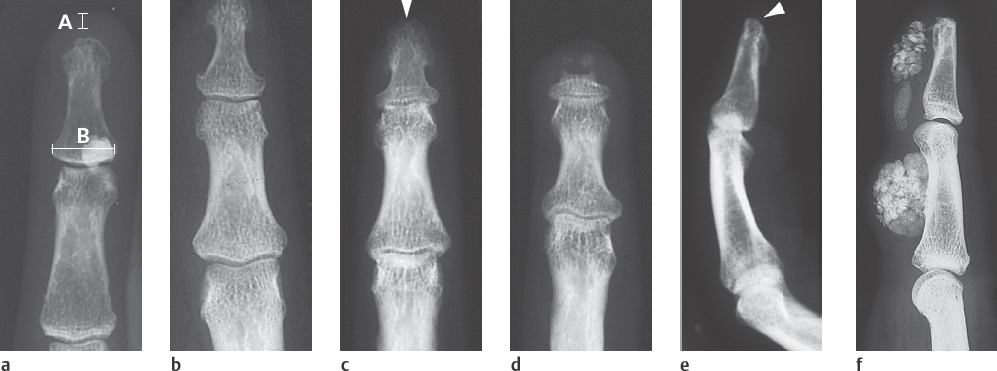
Typical findings are severe articular malalignments in the hands due to ligamentary instability without any other radiographic lesions ( Table 39.1 , Figs. 38.1c, 39.1 , 39.2 ).
Differential Diagnosis
Differential diagnoses include rheumatoid arthritis, which can be differentiated by the typical marginal erosions (see Figs. 36.1 and 38.1b ), Jaccoud arthropathy of rheumatic fever, which predominantly affect the ulnar side, Sharp syndrome, Ehlers-Danlos syndrome with articular malalignment, subcutaneous fat necroses, and signs of deforming osteoarthritis, as well as avascular osteonecroses.
Therapeutic Options
Depending on the disease activity, one can either wait or treat with immunosuppressive drugs. These include nonsteroidal anti-inflammatory drugs (NSAIDs), lowdose corticosteroids, hydroxychloroquine, azathioprine and even cyclophosphamide. The effectiveness of methotrexate, cyclosporine A, intravenous immunoglobulins, androgens, plasmapheresis, and immunoadsorption has not been confirmed.

Scleroderma, Progressive Systemic Sclerosis (PSS)
Pathoanatomy and Clinical Symptoms
Overproduction of collagen and obliteration of small blood vessels leads to inflammatory, fibrotic, and regressive lesions in the cutis and subcutis, as well as in internal organs. Manifestations in the gastrointestinal tract, lungs, kidneys, heart, transverse-striated muscles, and bones result in the classic disease entity of progressive scleroderma, as well as a number of variants, which are listed in Table 39.2 . Painful micronecroses of the integument arise as a result of the underlying angiopathy. Immobile joints are a result of fibrosis of the synovium. Women in their third to fifth decades of life are primarily affected (female:male ratio = 3:1).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree