18 Lesions in the Ulnocarpal Compartment
When the distal radioulnar joint is unstable and there are complaints concerning the ulnar side of the wrist, the presence of a lesion in the triangular fibrocartilage complex should be considered after excluding an osseous injury. Lesions in the ulnocarpal compartment can be degenerative, traumatic, or a combination of both, and it is not always possible to determine the exact cause. Noninvasive MRI performed with intravenous or intraarticular contrast agent, and arthroscopy, which offers treatment options in the same session, are best suited for diagnostic imaging. A frequent cause of ulnar-sided wrist pain is the ulnocarpal impaction syndrome, for which the pathoanatomic basis is positive ulnar variance (ulna relatively too long). Since all components of the triangular fibrocartilage complex go through a physiologic aging process, imaging results can be interpreted only in relation to clinical symptoms.
Lesions of the Triangular Fibrocartilage Complex
Anatomic Abnormalities and Clinical Symptoms
The triangular fibrocartilage complex (TFCC) fills the space between the ulnar head and the ulnar part of the proximal carpal row (lunate, triquetrum) like a cushioned buffer and stabilizer. It is immediately adjacent to the distal radioulnar joint, with which it forms a functional unit. The normal anatomy and methods of diagnostic imaging are elucidated in Chapter 11.
Lesions of the TFCC are manifest not only on the avascular triangular fibrocartilage (TFC), but also in the vascularized periphery of the complex. Injuries can occur to the ligaments (ulnolunate and ulnotriquetral ligaments, palmar and dorsal radioulnar ligaments, ulnar collateral carpal ligament) and the connective tissues (meniscus homologue, tendon sheath of the extensor carpi ulnaris muscle). Secondary injuries regularly develop after a while on the articular cartilage of the ulna head and the lunate and triquetrum. The following types of lesions are listed according to their origins.
Traumatic lesions: Compression, rotatory, or distractional injuries can cause avulsion of the TFC from its ulnodistal attachment together with a fracture of the ulnar styloid process. In contrast, rupture of the ulnoproximal TFC usually occurs without involvement of the ulna. The radioulnar ligaments are also frequently injured, and these injuries often lead to instability in the distal radioulnar joint. TFC tears near their radial insertion are also common. TFC avulsion directly from the radius during hypersupination or hyperpronation injuries and rupture of the ulnolunate and ulnotriquetral ligaments on the palmar side are less common injuries.
Chronic degeneration: Degenerative changes in the TFC occur from the third decade of life. Therefore, they are considerably more frequent than traumatic lesions. More than 40% of individuals over 40 years of age and at least 60% of those over 60 have asymptomatic TFC lesions. Predisposing factors are positive ulnar variance and the intensive occupational use of the hand. The degeneration progresses in stages. Initially mucocystic inclusions appear within the swollen fibrocartilage, especially on the proximoulnar aspect. With increasing age, the TFC becomes centrally thinner, and at some later stage perforates there. The degenerative process then progresses to the ligamentary periphery. In later stages, the articular cartilage of the ulna head and the proximal aspects of the lunate and triquetrum is impaired by denudation.
Combined degenerative-traumatic lesions: Among the elderly with pre-existing degenerative TFC changes, a relatively minor trauma can lead to a partial or complete tear of the TFC. These ruptures are often located on the proximal side of the TFC and run in a horizontal or oblique direction. Conversely, untreated TFC ruptures lead to early degeneration with loss of substance.
Lesions of neighboring osseous structures: Ulnar avulsion of the TFC with or without fracture of the ulnar styloid process often accompanies distal radius fractures (Frykman types II, IV, VI, and VIII). In the presence of nonunion at the base of the ulnar styloid process, both ulnar TFC insertions remain attached to the osseous fragment and can cause instability with constriction symptoms. In contrast, the radial TFC insertion is only rarely unstable enough to cause a relevant deformation of the TFC after radius fracture.
Negative ulnar variance is a congenital anomaly in which the TFC is more voluminous and usually deformed because of the enlarged ulnocarpal compartment. Positive ulnar variance always leads to mechanical alteration of the TFC and to ulnocarpal neoarticulation within the scope of an impaction syndrome.
Lunotriquetral dissociation as a form of ulnar-sided instability of the carpus is generally not the cause but the result of damage to the TFCC. A secondary result of injury to the radioulnar ligaments is subluxation in the distal radioulnar joint. Rupture of the palmar ligament leads to palmar subluxation of the radius, which results in the clinical symptom of “bouncing ulna.” Rare lesions of the dorsal radioulnar ligament cause the radius to drift dorsally.
In addition to the uncharacteristic feeling of tension, lesions of the TFCC can cause pain on the ulnar side of the wrist. In particular, proximal partial lesions on the ulnar side resulting from an injury or of a degenerative nature often cause persistent symptoms. A complete TFC avulsion on the ulnar side causes blockage resulting from constriction, as well as pain on movement. Isolated perforations perforations without surrounding degeneration generally do not cause any symptoms. Only when osteochondral remodeling of the lunate and triquetrum and the ulna head are manifest in addition to TFC perforation does swelling occur over the proximal carpal row with pain on the ulnar side of the carpus. This pain is most prominent during ulnar inclination, rotation of the forearm, and tight clenching of the fist. Patients also complain of a weak grip.
Classification
Palmer’s classification is most commonly used. It includes:
The etiology of the impaired triangular fibrocartilage complex (injury vs. degeneration)
The location of the lesion, depending on the degree of vascularization (avascular center vs. vascularized periphery)
The etiopathogenically derived form of therapy.
The following pathologies are differentiated ( Table 18.1 ).
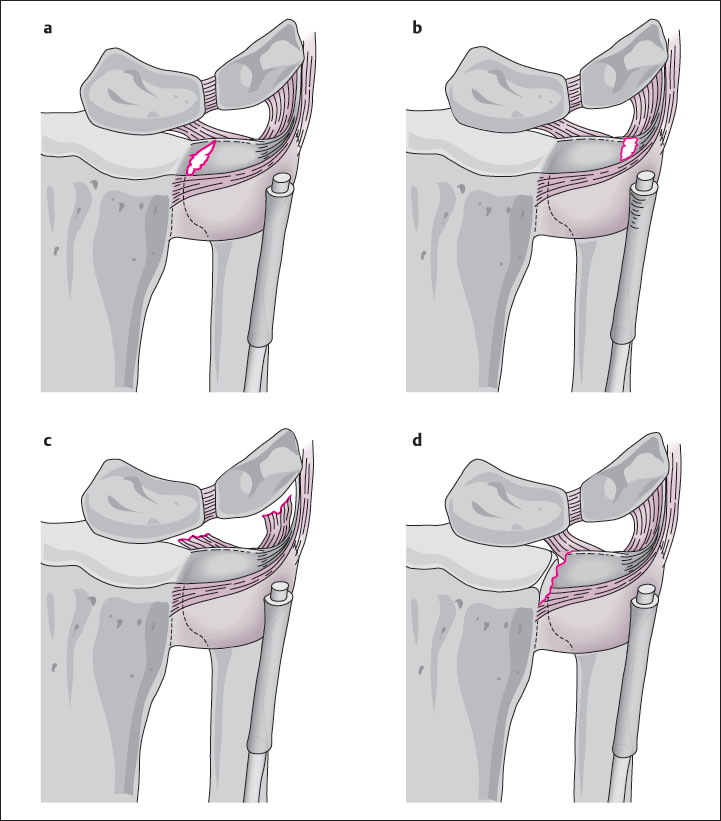
Class I: Traumatic Lesions
Subgroups I A-I D are classified according to the location of the injury and its degree of vascularization ( Fig. 18.1 ). The injury patterns I A and I D are localized in avascular areas and therefore tend to heal poorly. In contrast, lesions I B and I C are localized in vascularized segments and therefore generally heal well.
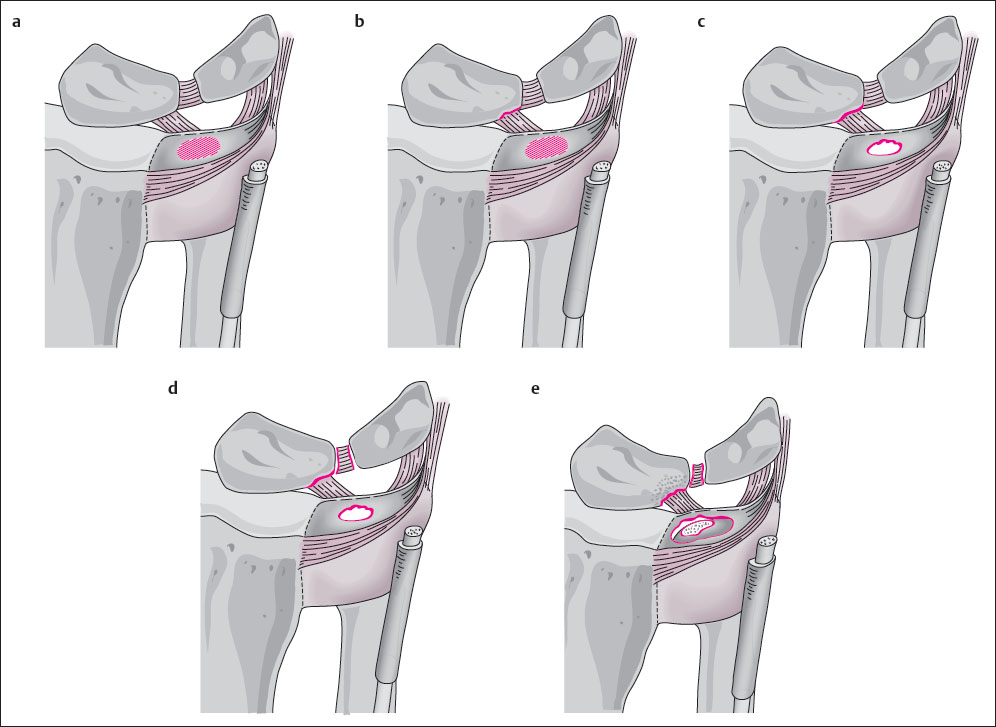
Class II: Degenerative Lesions
Categorization into subgroups II A-II E ( Fig. 18.2 ) depends on the extent of degeneration of the TFC, as well as of the articular cartilage and bone on the ulna head and the lunate and triquetrum, and the condition of the lunotriquetral ligament. Except for the ulnocarpal impaction syndrome, degenerative lesions of the TFCC cause no or only mild symptoms.
Diagnostic Imaging
It is essential that results of diagnostic imaging of the TFCC always be analyzed and evaluated in the context of the patient’s symptoms. The goal of presurgical diagnosis of the TFCC must be the exact localization and gradation of the lesion so that sophisticated therapy can be planned.
Magnetic Resonance Imaging
MR Imaging Techniques
The prerequisites explained in Chapter 11 for optimal examination of the TFCC include use of a middle- or high-field scanner, a dedicated surface coil with an FoV of 8–10 cm, slice thicknesses of 2 mm for coronal 2D sequences and partition thickness of 1mm or less for 3D datasets, as well as intravenous and/or intra-articular application of a contrast medium based on gadolinium chelates.
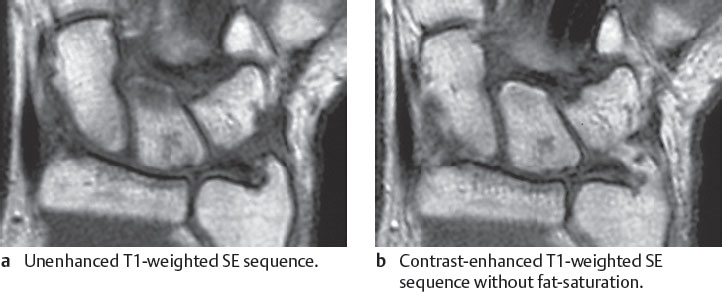
For the diagnosis of lesions of the TFCC, results of plain MRI are significantly inferior to those of examinations performed with contrast enhancement:
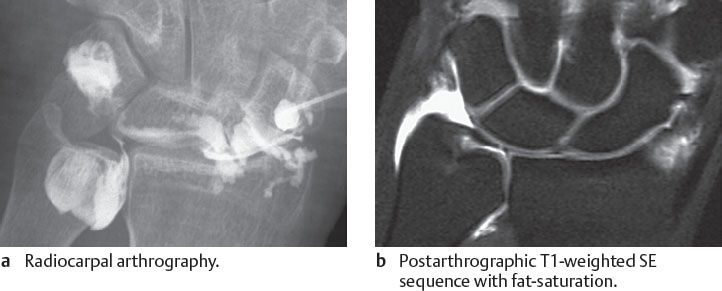
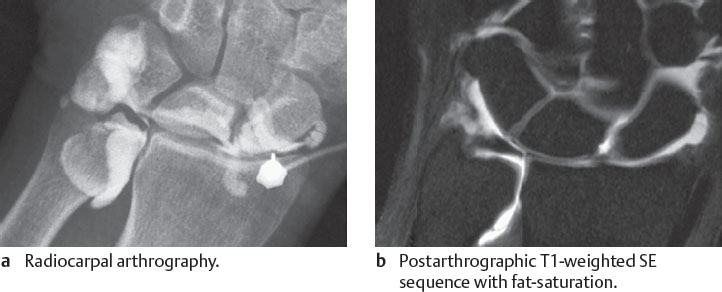
Lesions in the central, avascular segment of the TFC are best identified with a combined procedure consisting of two-compartment arthrography and MRI (MR arthrography).
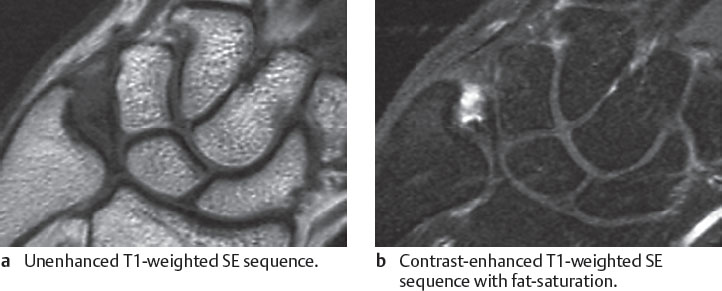
Peripheral lesions in the vascularized segments of the TFCC are detected sensitively after intravenous administration of gadolinium because of enhancement of fibrovascular tissue at the site of injury.
In clinical routine, however, not every patient with symptoms on the ulnar side of the wrist can be examined with arthrography and subsequent MRI. The sequences shown in Table 18.2 offer a reliable compromise.
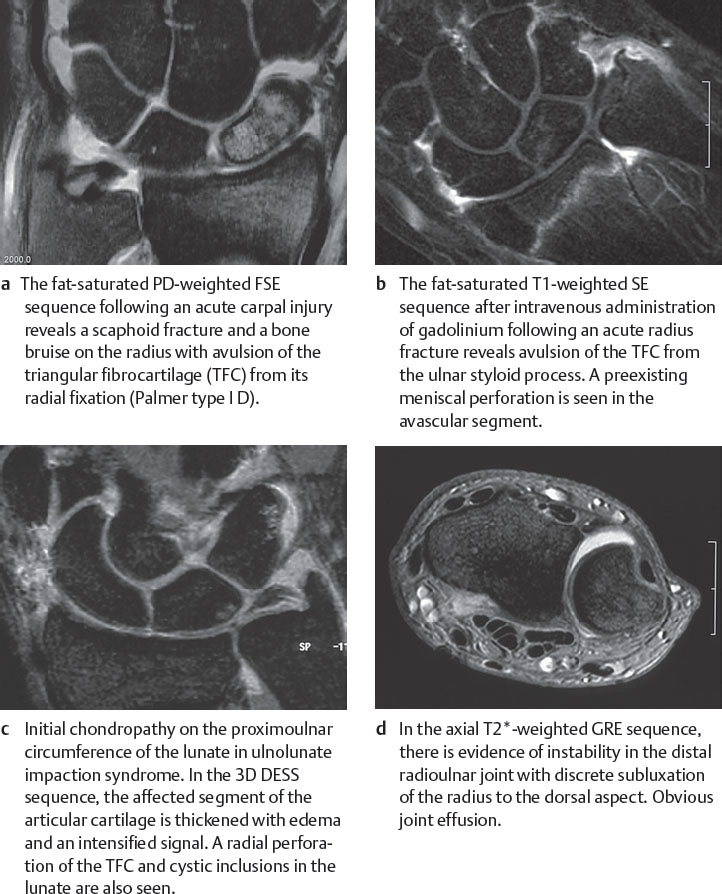
In this sequential program, lesions in the avascular segments of the TFCC are identified with the fat-suppressed PD-weighted FSE sequence (Fig. 18.3a), as well as with a 3D T2*-weighted GRE sequence. Ligamentary lesions can be detected in vascularized segments with T1-weighted SE sequences before and after intravenous application of gadolinium (Fig. 18.3b). Chondropathies of the articular cartilage can be recognized with 2D sequences (like PD-weighted FSE fat-saturated sequences) or 3D sequences (like 3D T2*-weighted GRE or water-excited, dual-echo steady-state [DESS] sequences) (Fig. 18.3c) and subluxations in the distal radioulnar joint with an axial T2*-weighted GRE sequence (Fig. 18.3d).
If the clinical question is explicitly aimed at discovering abnormality in the avascular segment of the TFC, the articular cartilage, or both, conducting MR arthrography first is recommended.
MR Imaging Results
Table 18.3 contains all MRI results that are found in traumatic and degenerative lesions of the TFCC
In the assessment of TFCC lesions, MRI by means of the technique described above shows sensitivities and specificities well above 90% in comparison to the gold standard of arthroscopy. MRI offers the advantage of demonstrating the inner structure of the TFC and the ligaments, thereby enabling degeneration to be definitively detected in early stages. In the TFCC, specific criteria of injury must be distinguished from general criteria:
A special sign of acute traumatic rupture is structural dehiscence of the TFC with sharply defined edges (Figs. 18.3a, 18.4 , 18.7 ). In contrast, a special sign of chronic degeneration is wide dehiscence with blunt edges ( Figs. 18.9 – 18.12 , 18.16 ).
General signs in an injured TFCC do not permit differentiation into degenerative or traumatic etiology. Un-specific, hyperintense accumulations of fluid with communication between the compartments of the radiocarpal and the distal radioulnar joints are often found at the site of the TFC or ligamentary lesion in T2-weighted sequences (Fig. 18.3a, c, d).
Although differentiation between traumatic and degenerative lesions in the TFCC is often not possible with imaging procedures, these two classes of lesions will be discussed separately for reasons of clarity.
Traumatic TFCC Lesions in MR Imaging
In traumatic tears, the diagnostic strategy in MRI depends primarily on the degree of vascularization at the site of injury:
Injuries of the fibrocartilaginous TFC can be recognized in plain T2*- and PD-weighted sequences that depict hyperintense inclusions with a definite form. In type I A ruptures, there is a vertical slit-shaped line 1–2mm from the radial origin of the TFC extending to both TFC surfaces ( Fig. 18.4 ). In type I D ruptures, an oval spot is seen between the articular cartilage of the sigmoid notch of the radius and the detached, often only slightly dislocated TFC (Figs. 18.3a, 18.7 ). Horizontal tears in the TFC are comparatively rare. A type I A lesion can be overlooked in plain MRI when there is a small tear without joint effusion. Complementary MR arthrography is recommended when persisting symptoms indicate a TFC injury.
Demonstration of ligamentary TFCC lesions in MRI is significantly facilitated by means of intravenous application of gadolinium. The location of the ligaments and the TFC periphery correspond to the vascularized segments of the TFCC in which fibrovascular regeneration tissue appears a few days after the injury. Pathoanatomically, the regeneration tissue has significantly increased blood circulation. The hyperemic or hypervascular reaction can be visualized in fat-saturated, T1-weighted sequences after intravenous application of gadolinium causing hypere enhancement. Focal contrast enhancement indicates avulsions of the TFC ligamentary insertions on the ulnar styloid process (type I B rupture, Figs. 18.3b, 18.5 ), avulsions of the ulnolunate and ulnotriquetral ligaments (type I C rupture, Fig. 18.6 ), and ruptures of the radioulnar ligaments in presence of an instable distal radioulnar joint.
Degenerative TFCC Lesions in MR Imaging
Early degenerative changes in the central, avascular section of the TFC can be identified in fat-saturated, PDweighted FSE sequences, as well as in T2*-weighted GRE sequences, as hyperintense spots and lines that do not reach the TFC surface. The hyperintense signal is caused by mucocystic inclusions and altered binding behavior for “free water” ( Fig. 18.8 ). Early stages of TFC degeneration and perforation can be more precisely defined with the MRI criteria listed in Table 18.4 than with Palmer’s classification.
Advanced degenerative changes in the shape of the TFC can best be seen in MR arthrography. A 1:200 diluted gadolinium solution increases the contrast between the surface of the altered TFC and the surrounding structures in the joint. The distending effect of gadolinium simultaneously optimizes detailed visualization of incomplete and complete perforations in the central, avascular segment of the TFCC (Figs. 18.3c and 18.9 – 18.11 ). MR arthrography identifies degenerative (and traumatic) lesions of the TFCC with a diagnostic precision greater than 95% in comparison to arthroscopy. In advanced stages, the etiology of a deformation of the TFC usually remains unknown, as it can occur as a primarily degenerative process, as well as secondarily through retraction after a traumatic TFC avulsion.
As early as stage II B, swelling or denudation of the articular cartilage of the ulna head, the lunate, and more rarely of the triquetrum can be depicted. An attempt can be made by using fat-saturated PD-weighted FSE sequences or a dedicated T2*-weighted 3D GRE sequence to identify a signal change within the articular cartilage and a decrease in its height (Figs. 18.3c, 18.10 ). The lesion is best detected in the presence of joint effusion, which distends the layers of articular cartilage. However, if this is not the case, initial cartilaginous lesions can escape detection in MRI due to the height of the cartilage layers measuring less than 1 mm at the wrist.
When assessing TFC lesions, attention must be paid to the following pitfalls:
The hyperintense, vertical articular cartilage of the sigmoid notch of the radius, from which the TFC originates, can be mistaken for a I D lesion.
The hyperintense fatty tissue between the two ulnar fascicles of the TFC and fluid in the ulnar recess must be differentiated from a I B lesion.
In all types of sequences, the surface of the articular cartilage is delimited by a dark, hypointense line. In case of a wide degenerative type II C perforation in the middle segment of the TFC, the articular cartilage of the ulna head and the lunate may resemble a filiform remnant of the TFC (Table 18.16). The situation becomes clearer if the layers of articular cartilage at the level of the perforation are distended by a joint effusion or intra-articular gadolinium.
Table 18.5 contains a complete summary of pathoanatomy, classification, and MRI signs of TFCC lesions.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree