23 Carpal Instability
The historical term carpal instability means a derangement of the carpal joints with malalignment of the carpal elements in relation to each other. Depending of the degree of severity, dynamic types, which only become manifest during movement of the wrist, are differentiated from static types, which can be identified during rest. The causes are generally traumas, degenerative or constitutional ligamentary lesions, and less often arthritis or crystal deposition diseases. Clinical signs are click and snap phenomena, as well as a weak grip. More recent classifications differentiate dissociative instability types located in the proximal carpal row (scapholunate and lunotriquetral dissociation) from nondissociative instability types, in which dissociation of the entire proximal carpal row exists en bloc (radiocarpal and midcarpal instability, ulnar translocation). The diagnostic methods include, in addition to radiography and stress views, cineradiography, computed tomography (CT), and magnetic resonance imaging (MRI), with intravenous or intra-articular administration of a contrast agent, and arthroscopy. The diagnostic significance of the individual procedures is described in this chapter.
Pathoanatomy and Clinical Symptoms
Stability of two joint partners is defined as their ability to maintain a physiologic position in relation to each other under normal conditions. An equilibrium exists, in which each external force calls forth a counterforce, which restores the original articular condition.
Instability or derangement between two articulating structures describes the unphysiologic condition in which the anatomic order or the regular movement of the two articulating partners is disturbed. In unstable conditions, the counterforces are tooweak to maintain or restore the physiologic equilibrium.
The wrist is predisposed to malalignment for two main reasons. As an intercalated link in the chain between the forearm and the metacarpus, the wrist is exposed to intense axial forces (“kinetics”). With its several small joints, the wrist has an unusually high freedom of movement (“kinematics”). Both characteristics of the wrist — the constant height in spite of considerable axial forces and the motion-dependent plasticity – can be summarized with the term “flexible spacer.”
Although the original term “carpal instability” (Linscheid 1972) described only malalignment of the lunate, the term now denotes any disturbance of the carpal equilibrium in which an abnormal alingment of two or more carpal elements is present under conditions of normal load in daily life.
Pathophysiologically, carpal instability can be initiated by intrinsic or extrinsic factors:
Intrinsic factors denote an insufficiency of the wrist stabilizers (carpal ligaments, joint capsules, and flexor and extensor tendons). Rupture of the scapholunate ligament followed by development of scapholunate dissociation (SLD) is an example of such an intrinsic factor.
Extrinsic factors come into play as a result of the abnormal geometry of the joint surfaces of the carpal bones and the distal forearm. Malunion of a distal radius fracture with an abnormal tilt of its joint surface is a typical example of extrinsic factors.
Hyperextension injury is the most common pathomechanism of carpal instability. It usually leads to injury on the radial side of the carpus. Hyperpronation as a cause of carpal instabilities is rare and can cause instability on the ulnar side of the carpus. Many questions remain unanswered, however. Aside from the common traumatic causes, ligament lesions can arise from a number of different pathologic conditions ( Table 23.1 ).
The severity of carpal instability generally is determined by the intensity of the causative ligamentary and/or osseous injury. When there is mild ligament insufficiency, instability only becomes manifest under dynamic conditions. If the same ligament is completely ruptured, static instability can occur. Dynamic instability is present if the carpal bones appear normal in standard radiographs taken at rest, but abnormal movement is identified in clinical examination, radiographic stress views, or cineradiography. If an abnormal alignment of the carpal bones is depicted during imaging of the resting hand, the discriptive term is static instability.
Mayfield’s categories of progressive perilunate instability are useful for quantification of the articular derangement of the wrist. Four degrees of severity are differentiated according to the number of injured ligaments ( Table 23.2 ). These were determined on anatomic specimens that were exposed to injuries in extension, ulnar inclination, and supination under experimental conditions.
|
Classification
Since many questions regarding carpal instability remain unanswered, every attempt at classification appears inadequate and incomplete. Of the multitude of classifications that have so far been attempted, the classification presented in Table 23.3 is based on a suggestion by Amadio from the Mayo Clinic in Rochester, MN. The classification is based on the degree of continuity of the proximal carpal row, which either shows a ligament interruption (so-called dissociative instability) or remains intact in its entirety in the presence of an instability that is located elsewhere (so-called nondissociative instability).
In this classification, dissociative instability (CID = carpal instability dissociative) is distinguished from nondissociative ones (CIND = carpal instability nondissociative), as well as from complex instability (CIC = carpal instability complex) and axial instability (CIA = carpal instability axial).
In the dissociative CID group, the bones of the proximal carpal row are displaced in relation to one another. If a ligament of the proximal row is ruptured, either the scaphoid is malaligned in relation to the lunate (CID-DISI), or the lunate is out of alignment with the triquetrum (CID-PISI). When the scaphoid is fractured or pseudarthrotic, the two scaphoid fragments are out of alignment.
In the nondissociative CIND group, the proximal carpal row is intact, but as a union is malaligned with the distal carpal row (CIND-DISI and CIND-PISI) or is subluxated in relation to the forearm (so-called translocation). The pathoanatomic basics are lesions of the extrinsic (capsular) carpal ligaments or a malaligned radial joint surface. The dissociative and nondissociative forms of instability often represent chronic sets of complaints, which are caused by a sufficient wrist trauma or so-called lax joints (especially the CIND type). Often, however, no sufficiently plausible causes can be found.
These instability conditions are opposite to the acute dislocation or fracture-dislocation of the carpus, in which the complex CIC instability group and axial CIA instability group should be differentiated. These patterns of dislocation generally include dissociative and nondissociative elements. They lead to gross deformity and acute loss of functional ability of the hand. The complex and axial forms of injury, which were discussed in Chapter 22, will not be further elucidated here. A multitude of different patterns of carpal injury exists between the acute and chronic lesions, which represent the opposite extremes on a pathoanatomic and clinical scale.
The acronyms DISI and PISI describe characteristics of the pathologic alignment of the lunate in the middle carpal column. They are not terms for individual disease entities. The lunate, as an intercalated and therefore potentially unstable link in the middle carpal column, can be rotated into positions that induce two carpal zigzag deformity patterns as follows ( Fig. 23.1 ).
A DISI configuration (dorsal intercalated segment instability) is present when the lunate is rotated in extension so that the radiolunate angle is larger than 15°. This is seen most often in scapholunate dissociation (SLD).
In contrast, a PISI configuration (palmar flexed intercalated segment instability) is present when the lunate is in flexion (radiolunate angle smaller than−15°). This relatively rare condition is found in midcarpal instabilities (MCI) and those located on the ulnar side – usually with lunotriquetral dissociation (LTD).
Clinically, the different forms of carpal instability cause pain and different degrees of carpal dysfunction, which will be discussed together with the individual forms of instability because of the considerable differences in clinical and radiographic presentation.
Diagnostic Imaging
Radiography
It is essential for correct interpretation that radiographs are taken with the wrist in neutral position and with correct beam alignment (Chapter 1). The radiographic settings in Table 23.4 represent a standard program for radiographic evaluation of carpal instability.
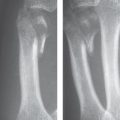
A carpal malalignment is suspected in the dorsopalmar projection when at least one of the three radiographic Gilula’s carpal lines is interrupted, i.e., the cortical contours of the carpal bones involved are no longer parallel or have a step deformity, or the lunate is triangular or moon-shaped. It must be borne in mind, however, that a severe ligament injury can be present without any signs in standard radiographs. In this situation, functional stress views are indicated. Conventional stress views include the dorsopalmar projection in maximal radial and ulnar inclination, as well as lateral projections in maximal flexion and extension (Chapter 1). Experience has shown that insufficiency of the carpal ligaments can be documented better with dorsopalmar radiographs while the hand grips a tennis ball tightly or, alternatively, with Stecher’s view. Since this procedures are diagnostically more efficient and exposes the patient to less radiation, these two functional projections are designated as the preferred stress views in Table 23.4 .

In the lateral radiograph, each angle that exceeds the normal values listed in Table 12.1 must be considered as a pathologic DISI or PISI configuration. Figure 23.2 shows the pathologic angles of the most common types of carpal instability.
|
Stres radiographs of first choice
|
Stress radiographs of second choice
|
In diagnostically unclear situations, appropriate comparison radiographs must be taken of the other hand.
Cineradiography
A cineradiographic examination is indicated when click or snap phenomena during movement cannot adequately be explained with radiographs taken at rest and under stress loading. The imaging method of choice is high-resolution cineradiography with at least 25 views/second (Chapter 2). After the forearm is placed in neutral position, four series are acquired: radial inclination/ulnar inclination movements in dorsopalmar and lateral projections, as well as flexion/extension movements in lateral and dorsopalmar projections. The patient usually knows best which movements provoke a “snap.” Video documentation and storage of pulsed fluoroscopy are also possible, but image quality is lower.
Arthrography
When symptoms are on the ulnar side of the wrist, three-compartment arthrography is performed. Two-compartment arthrography is generally applied for complaints concerning the radial side. A bidirectional passage of contrast medium in patients younger than 30 years almost certainly indicates a relevant ligament lesion. In patients more than 30 years old, there is only a loose correlation between the clinical and arthrographic findings due to degenerative perforations at the ligaments, so that correct film interpretation can only be made together with clinical symptoms. It is advantageous to perform arthrography as a combined procedure followed by MRI or CT. So-called MR arthrography and CT arthrography offer the advantage of direct imaging of the intra-articular ligamentary stabilizers with excellent contrast-to-signal ratio.

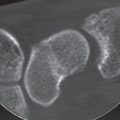
Computed Tomography
In early stages of instability, CT is advantageous only when stress views cannot be taken because the limb is immobilized in a cast or the joint surfaces at the level of the suspected articular malalignment overlap in several planes in the radiographic projection views. This is especially true for midcarpal forms of instability. In later stages, CT is the method of choice when osteoarthritic changes in the involved unstable joint are to be confirmed or excluded in surgical treatment planning.
Magnetic Resonance Imaging
As discussed in detail in Chapter 10, different plain and contrast-enhanced types of MRI sequences are available for the evaluation of ligament tears:
In plain MRI, the carpal ligaments are best seen in a T2*-weighted gradient-recalled echo (GRE) sequence in the coronal plane. The slices should be no thicker than 2 mm, as otherwise partial-volume effects appear on the scapholunate and lunotriquetral ligaments. Axial slices are recommended with the same sequence because the dorsal and palmar segments of the ligaments can be especially well demonstrated in this plane.
In indirect MR arthrography, a T1-weighted sequence is performed about one hour after intravenous injection of gadolinium-DTPA followed by active joint movements (see Fig. 9.5e, f). Because of only the slight distending effect of the contrast medium that has dispersed into the joint space, direct MR arthrography is superior to the indirect technique.
Direct MR arthrography is an invasive procedure with intra-articular injection of a 1:200 diluted solution of a gadolinium dye. Under sterile conditions and fluoroscopic control, a solution consisting of 200 parts of an x-ray dye and one part of a gadolinium dye is injected into the midcarpal, the radiocarpal, and/or the distal radioulnar joint(s), applying the two- or three-compartment technique (Fig. 9.5c, d).
In contrast-enhanced MRI, there is increased uptake of gadolinium at the site of the ligament tear (Fig. 9.5a, b). The pathoanatomic foundation is hyperemia within the fibrovascular repair tissue, which immediately develops in the injured area. The focal hyperemia leads to contrast enhancement.
Dynamic MRI can demonstrate movement patterns of the wrist. In real-time imaging, high-field scanners with strong gradient systems are essential. Movements of the carpal bones can be analyzed in the cineloops. Carpal ligaments are not seen or are inadequately depicted because of the reduced resolution matrix. For this reason, dynamic MRI at present offers no advantages over conventional cineradiography.
Moreover, joint surfaces can be seen without overlapping in the sectional scan in MRI and in CT, with which joint malalignment causing static instability can be recognized more easily. Table 23.5 shows MRI results in relation to the pathoanatomy of the ligaments.
Arthroscopy
Diagnostic arthroscopy is indicated for carpal instability with typical symptoms but unremarkable findings in the imaging procedures and also for pretherapeutic determination of accompanying damage of the articular cartilage (Chapter 4). This approach must be differentiated from arthroscopy performed primarily for therapeutic reasons.
Forms of Instability
Dissociative Carpal Instability (CID)
Scapholunate Dissociation (SLD)
Pathoanatomy and Clinical Symptoms
The most common and most important form of carpal instability is caused by an insufficiency of the scapholunate ligament. An acute or previous fall on the dorsally extended hand is generally the traumatic cause. Chapter 17 discusses the combined injury, including an intraarticular radius fracture with force vector which radiates into the scapholunate compartment (see Fig. 17.9 ). Somewhat less common are the causes listed in Table 23.1 , which should be taken into consideration especially in chronic stages and when a causative accident cannot definitely be identified. In nontraumatic dissociations, a partial rupture develops from a stretched ligament, which finally proceeds to a complete rupture after various intervals of compensation.
A partial rupture must be differentiated from a complete rupture in degree of the SLD severity. In a partial rupture, only one or two ligament segments are discontinuous – generally the palmar and middle segments – while the remaining segments are intact. In complete ruptures, all ligament segments are interrupted in their continuity. The most common rupture site is on the scaphoid side of the scapholunate ligament because Sharpey’s fibers are less dense on this side of the ligament than on the lunate side.
The lesion of the scapholunate ligament precedes the dissociative form of carpal instability (CID-DISI). An isolated injury of the scapholunate ligament corresponds with stage I in Mayfield’s classification of perilunate instability. In more severe stages, additional ligaments are injured, the so-called secondary stabilizers of the scaphoid, particularly the palmar scaphotrapeziotrapezoidal and the radioscaphocapitate ligaments. In the “model of the broken ring” (Lichtman’s model), the scaphoid and lunate rotate independently because of the loss of their ligamentary connections ( Fig. 23.3 ):
The scaphoid rotates into flexion because of the increased axial pressure, resulting in a radioscaphoid angle greater than 60°. The flexion tendency of the scaphoid is increased if the radioscaphocapitate ligament, which acts as a fulcrum is also injured. The axial pressure now simultaneously presses the scaphoid in dorsal direction, where it rides on the dorsal rim of the radius. The pattern of malalignment combining flexion and dorsal translation is referred to as rotatory subluxation of the scaphoid (RSS) (Fig. 23.3c, e).
After the scaphoid has been uncoupled, the lunate follows its natural tendency to rotate dorsally (Fig. 23.3d, f). Main causes are its wedge-shaped configuration with a thicker palmar portion as well as the asymmetric dorsally more curved proximal surface. Further influences on the dorsal rotation of the lunate are applied by the adjacent carpal bones, e.g., by the triquetrum, which rotates in the same direction via the connecting lunotriquetral ligament, and also by the capitate, which is in relative flexion. The result is a dorsal zigzag deformity of the middle carpal column with abnormal radiolunate and lunocapitate angles. Together with a mild palmar translation of the lunate, a so-called DISI configuration develops.
As a result of rotations in opposite directions, the scapholunate angle increases to over 60° (normal value 30–60°). The scapholunate angle is the characteristic parameter of the scapholunate dissociative pattern.
Later, osteoarthritis sets in. It begins in the radioscaphoid joint, first between the proximal scaphoid pole and the dorsal rim of the radius. As it progresses, the osteoarthritis spreads to the entire radioscaphoid compartment before the degenerative process finally reaches the midcarpal joint. Because of destruction of the proximal scaphoid pole and ulnar translocation of the lunate, the head of the capitate continually pushes into the developing scapholunate gap and approaches the joint surface of the radius. This leads to carpal collapse (SLAC wrist = scapholunate advanced collapse). Further details can be found in Chapter 27.
The severity of scapholunate ligament (SLL) insufficiency is determined by the results of conventional radiographs ( Table 23.6 ).
In stage I of scapholunate insufficiency, there is usually a rupture of the palmar and middle sections of the SLL. In this early stage, radiographs of the wrist in two planes are always unremarkable. If Watson’s maneuver (scaphoid shift test) is positive, giving rise to suspicion of a partial rupture of the SLL, clinical suspicion can best be confirmed or excluded arthroscopically. A partial rupture of the SLL can also be identified in MRI with intravenous or intra-articular application of contrast medium, but with a somewhat lower rate of accuracy.
In stage II of scapholunate insufficiency, the SLL has already completely ruptured. The static radiographs of the wrist in two planes, however, reveal a normal alignment of the proximal carpal row. Diagnostic evidence of complete ligament dehiscence can be provided by arthroscopy, MRI, and cineradiography. The extent of associated lesions of the extrinsic ligaments is mild and cannot be identified by means of imaging procedures.
In stage III of scapholunate insufficiency (= dissociation), the static form of instability with oppositely rotated scaphoid and lunate becomes manifest as a result of complete tear of the SLL and severe lesions of the extrinsic ligaments, especially the palmar scaphotrapeziotrapezoidal ligament (STTL) and the radioscaphocapitate ligament (RSCL). Plain radiographs now reveal the characteristic radiographic signs listed in Table 23.7 , but no osteoarthrotic remodeling of the wrist.
Although it is not mentioned in conventional classifications, stage IV of scapholunate dissociation indicates manifest osteoarthritis. When the scapholunate dissociation has been present for some time, osteoarthritis develops in stages, as does carpal collapse (so-called SLAC wrist). Further details can be found in Chapter 27.

Acute symptoms of scapholunate dissociation after hyperextension trauma include a transient swelling, dorsal tenderness over the carpus and the anatomical snuff box, and limited range of movement. If the patient delays treatment, as is often the case, reduced strength and limited mobility with pain at the end of maximal motion predominate. Watson’s scaphoid shift maneuver provokes a dorsal subluxation of the proximal scaphoid pole in relation to the lunate during a radial inclination motion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree