20 Scaphoid Nonunion
The natural course of scaphoid nonunion is mainly determined by the parameters of fracture location, fragment dislocation, and osseous blood supply. Bony resorption begins at an early stage, followed by sclerosis and osteonecrosis of the proximal fragment. The final stage includes carpal collapse and osteoarthritis. This course can be reliably classified into stages or degrees of severity radiographically. Cross-sectional imaging (CT, MRI) should be performed for exact classification into stages of scaphoid nonunion and osteonecrosis of the proximal fragment. High-resolution CT best depicts the bony remodeling processes in the scaphoid and the periscaphoid joints. Contrast-enhanced MRI demonstrates the blood supply and viability of the proximal scaphoid fragment.
Pathogenesis and Clinical Symptoms
Nonunion develops after a scaphoid fracture if no osseous bridging between the fragments takes place. Causes can be an initially overlooked fracture (most often misdiagnosed as a simple sprain), insufficient immobilization, severe fragment dislocation with or without disturbance of the carpal alignment, and a fracture located at the proximal pole of the scaphoid. The special vascularization of the scaphoid with retrograde course of the nutrient vessels from distal to proximal is considered a predisposing factor for the development of scaphoid nonunion and avascular osteonecrosis of the proximal fragment.
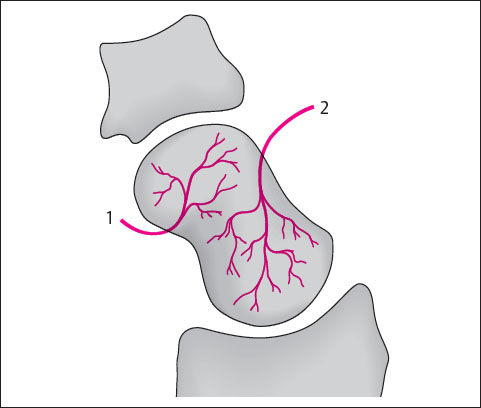
The peripheral entry of vessels from the radial artery at the level of the tubercle ensures that the middle and distal segments of the scaphoid are sufficiently vascularized, whereas the proximal pole is fed only by the terminal arteries and therefore has a comparatively sparse blood supply ( Fig. 20.1 ). Since the proximal section of the scaphoid has no independent blood supply, nonunion and osteonecrosis often develop after a proximal scaphoid fracture when the retrograde intraosseous vessels are interrupted by the injury. The special pattern of vascularization supports empirical observations that nonunion can be expected in 0% of fractures of the distal pole, 20% of fractures of the scaphoid middle (waist), and 36% of fractures of the proximal pole.
The natural course of scaphoid nonunion is characterized by progressive stages. As a sign of delayed union, excessive demineralization is seen near the fracture line in the fourth and sixth months after the trauma. During this transitional stage, the band-shaped resorption zones are still reversible under adequate immobilization therapy. If no osseous consolidation occurs, pseudocystic areas due to bone resorption indicate the irreversible stage of scaphoid nonunion. Cystic inclusions can be found in both scaphoid fragments. During progressive widening of the fracture line – especially on the palmar aspect as a result of fragment mobility – the margins of the fragments become sclerotic. These margins are either smoothed and eburnated or osteophytic. Trapping of the radioscaphocapitate ligament between the fragments can predispose to scaphoid nonunion.
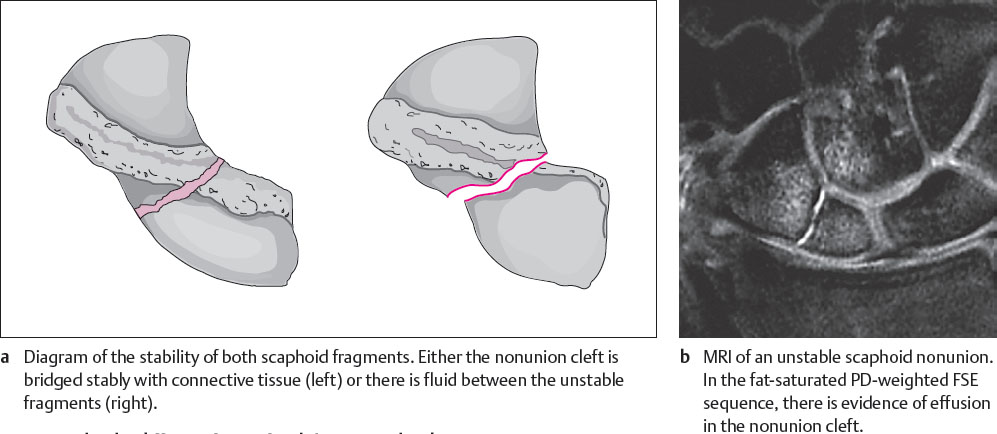
Table 20.1 lists possible results of a failed healing process following scaphoid fracture.
Delayed union of a scaphoid fracture must be differentiated from nonunion ( Table 20.2 ). The widened pseudarthrotic cleft with sclerotic margins can be filled with stabilizing connective tissue, but this is not always the case. Therefore, depending on whether tissue fills the cleft between the pseudarthrotic scaphoid fragments or not, stable (tight) nonunion is differentiated from unstable nonunion ( Fig. 20.2 ).
|
If there is a fragment dislocation immediately or an unstable nonunion, the altered statics and kinematics affect the entire carpus as time passes. First axial malalignment develops (carpal instability). Because of the configuration of the joint surfaces, the lunate together with the proximal scaphoid fragment rotates into an extended position, causing the so-called dorsiflexed intercalated segment instability (DISI) of the middle carpal column. The distal scaphoid fragment rotates oppositely into palmar flexion because the pseudarthrotic cleft is usually widened by increased palmar wear.
Unstable scaphoid nonunion always leads to osteoarthritis, which progresses in stages. The degenerative process begins focally as so-called styloid osteoarthritis between the radial styloid process and the distal scaphoid fragment (stage I osteoarthritis). The proximal fragment and the radiolunate joint compartment are characteristically not involved. With time, the progressive increase in pressure between the lunate and the head of the capitate leads to midcarpal osteoarthritis in the capitatolunate joint compartment (stage II osteoarthritis). The pattern of carpal collapse (scaphoid non-union advanced collapse = SNAC wrist) is obvious. This terminal stage of osteoarthritis is characterized by migration of the capitate in a proximal and radial direction and by a further increase in the radiocarpal and midcarpal osteoarthritis. These processes are further explained in Chapter 27.
The clinical symptoms are manifold. In the early stages, they are mild and consist of pain on radial inclination and vertical compression of the thumb. Wrist movement in radial and dorsal directions can be restricted. Carpal instability causes pain and swelling on the radial side of the wrist during exertion. At the stage of periscaphoid osteoarthritis, the wrist is swollen on the radial side and tends to swell with exertion; strength is also limited.
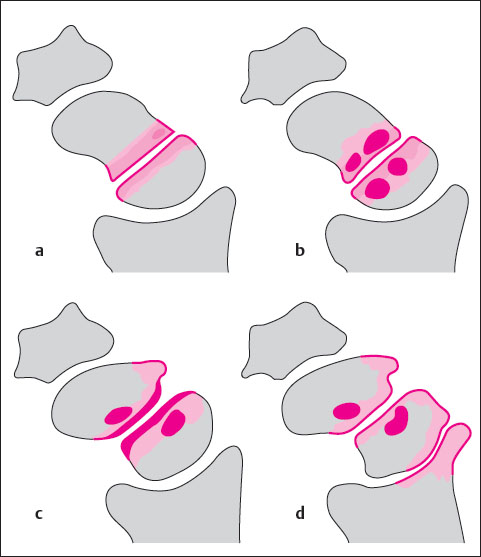
From a clinical standpoint it makes sense to apply stages I-III of Trojan and Jahna’s classification (1955), not only to add the final stage of osteoarthritis (stage IV) but also to consider whether carpal instability is also present in the other stages ( Table 20.3 , Fig. 20.3 ). The parameters of carpal instability and osteoarthritis primarily determine the therapy, which must include the entire carpus if both parameters have already become manifest.
Diagnostic Imaging
In diagnostic imaging of scaphoid nonunion, not only the osseous morphology of the scaphoid and the carpus but also the viability of the bone and bone marrow of the proximal scaphoid fragment must be assessed.
Radiography
Basic radiographic evaluation of the scaphoid consists of dorsopalmar and lateral projections in neutral position, as well as a Stecher’s projection (closed fist and ulnar inclination). If further imaging is required, high-resolution CT is recommended. If a CT scanner is not available, the additional radiographic projections of the so-called scaphoid quartet are taken (Schreck’s view in quill-holding position, Bridgeman’s view in 30° carpal extension, and hyperpronation view). The following radiographic signs are characteristic for scaphoid nonunion:
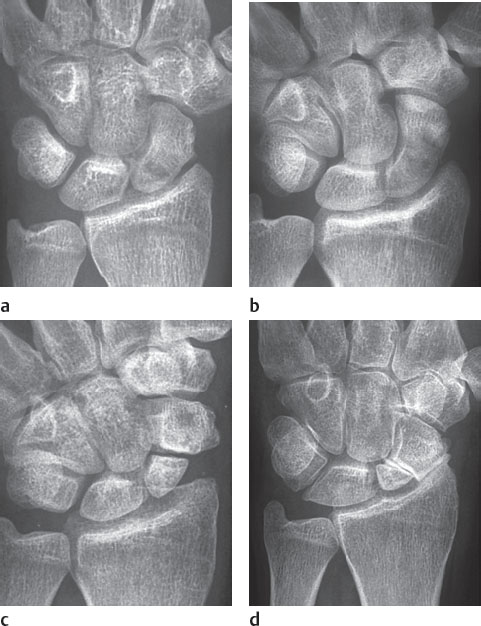
In reversible stage I, band-shaped resorption zones running parallel to the fracture line appear as a result of perifocal demineralization. These demineralized areas are symmetrical in both fragments and have indistinct margins (Fig. 20.4a).
In stage II, resorption cysts appear adjacent to the fracture. They indicate the irreversibility of the nonunion course. In both fragments the pseudocystic inclusions are most often located next to the nonunion cleft or in the periphery of the fragments (Fig. 20.4b). The cysts are characteristically surrounded by sclerotic margins. In projection radiographs, assessment of these pseudocysts is made difficult at later stages by displacement of the fragments and scleroses or osteophytes.
In stage III, complete manifestation of scaphoid nonunion has become apparent morphologically. On both fragments, the sides facing the nonunion cleft are covered with osteosclerotic bands, and their surfaces appear to have overhanging edges (Fig. 20.4c). The transition zones between the nonunion cleft and the radiocarpal and midcarpal joints are either rounded (atrophic form of nonunion) or has osteophytes (hypertrophic form of nonunion), especially on the dorsal aspect. Fibrocartilaginous connective tissue, which sometimes can be present in the nonunion cleft, cannot be directly visualized radiographically. Differentiation between a stable (“fibrous union”) and unstable (“pseudarthrosis”) nonunion can, therefore, be made only with stress views, arthrography, or MR arthrography.
In stage IV, styloid osteoarthritis is located between the radial styloid process and the distal scaphoid fragment (Fig. 20.4d). The joint space is focally narrowed, the subchondral bone is increasingly dense as a result of osteosclerosis, and the joint partners are deformed with osteophytes. Initial stages of osteoarthritis may not showup in conventional radiographs and are more easily recognized in CT images. At later stages, these osteoarthritic signs can be identified in the radioscaphoid compartment and in the midcarpal joint between the lunate and the head of the capitate. Finally, the capitate slides proximally along the lunate, which is in a DISI rotated position. This lessens the height of the carpus and ultimately leads to a carpal collapse (SNAC wrist).
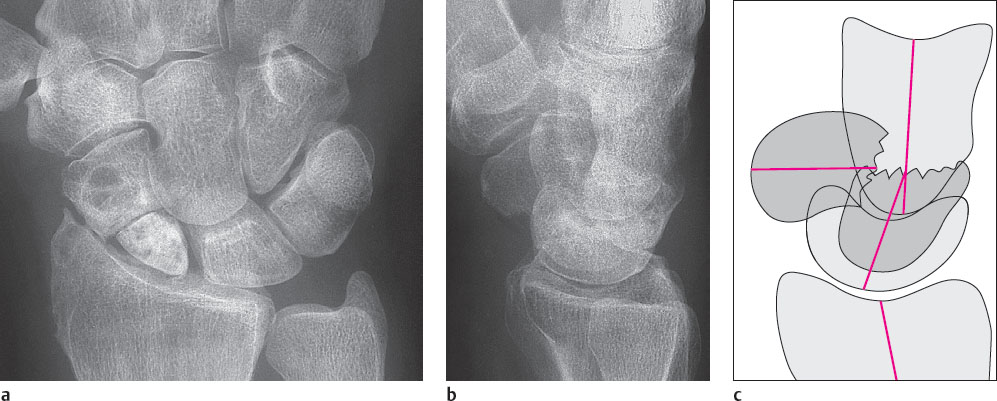
An associated carpal instability can easily be recognized in standard radiographs in two planes ( Fig. 20.6 ). The lunate, together with the proximal scaphoid fragment rotates dorsally, while the distal fragment is in a palmar flexed position. In the dorsopalmar radiograph, the distal scaphoid pole appears circular (“ring sign”), and the lunate assumes a triangular shape. The lines connecting the radius, the lunate and capitate, and metacarpal III, which are normally colinear in lateral radiographs, are interrupted in a zigzag deformity. The result is a loss in height in the proximal carpal row, which can be quantified with Youm’s carpal index (ratio of the lengths of the carpus and metacarpal III, normal value: 0.54±0.03) or with the Nattrass’ carpal index (ratio of the lengths of the carpus and the capitate, normal value: 1.57±0.05).
In advanced stages of scaphoid nonunion, the proximal fragment is increasingly narrowed and small (“nipple sign”), leading to discrepancy between the sizes of both scaphoid fragments. Furthermore, the proximal fragment appears radiographically dense. A manifest osteonecrosis of the proximal scaphoid fragment can only be indirectly diagnosed on the basis of the relative density of the trabecular bone as demonstrated on radiographs. The increased bone density is primarily a sign of disturbed osteoclastic function. However, the degree of osteosclerosis must be estimated carefully for two reasons. First, dorsal extension of the proximal fragment may imitate abnormal bone density because of its orthogonal projection in standard radiographs. Second, osteosclerotic changes in the proximal fragment, whose viability is endangered, can only be assessed in relation to the other parts of the carpus, which is often osteoporotic due to wrist disability.
With osteoporosis or after bone graft surgery, reduced bone density makes it difficult to recognize fine osseous bridges in delayed union.
In principle, the same morphologic parameters of scaphoid evaluation are assessed in conventional radiography and in CT. Therefore, the findings of both methods in scaphoid nonunion are combined in Table 20.4 .
Computed Tomography
High-resolution CT is preferably carried out with use of the multislice spiral technique with 0.5 mm, 0.75 mm, or 1.0 mm thick oblique-sagittal slices parallel to the longitudinal axis of the scaphoid (Chapter 8). In general, CT should be performed when scaphoid nonunion is known or suspected. High-resolution CT offers several advantages:
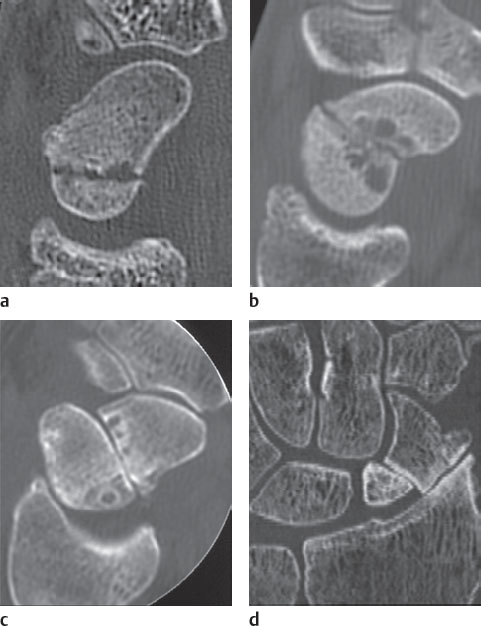
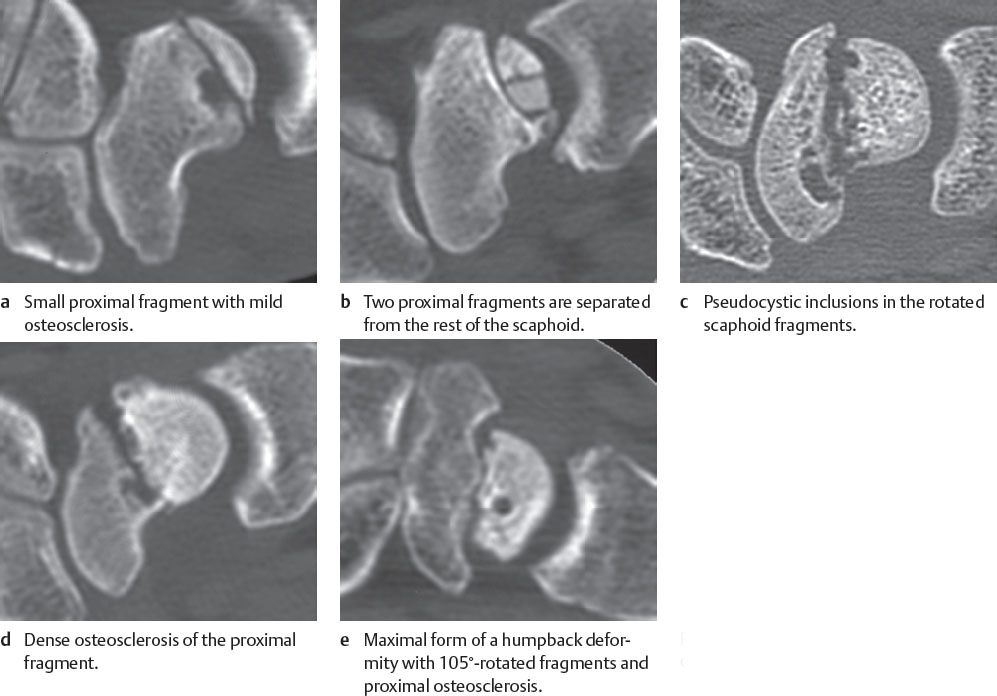
Osseous resorption zones along the fracture line, as well as adjacent pseudocystic inclusions in the scaphoid fragments, are detected earlier and with fine morphologic details in CT imaging (Fig. 20.7a, c). Osteosclerosis of the fragment margins can generally be visualized only in CT scans.
In high-resolution CT imaging, the nonunion cleft often appears larger because the summation effect that is always present in projection radiography is avoided.
Radioscaphoid osteoarthritis between the radial styloid process and the distal scaphoid fragment and midcarpal osteoarthritis between the lunate and the head of the capitate are visualized earlier and in more detail on CT images (Fig. 20.5d).
Spongiosclerosis of the proximal fragment as a sign of manifest osteonecrosis (Fig. 20.7d, e) is recognized with greater certainty because CT provides improved density resolution, and the possibility of misdiagnosis due to the tilted scaphoid fragment is avoided.
The domain of CT is the identification and quantification of fragment dislocations. It is of clinical importance to identify the so-called “humpback” deformity, where the proximal scaphoid fragment is rotated into extension and the distal fragment into flexion (Fig. 20.7c, e). The resulting angle between the fragments is often up to 90°. An ad-latus dislocation to the palmar or dorsal aspect can be recognized within the scan plane. However, dislocation to the radial or ulnar side is visualized better in multiplanar reconstructed CT images.
An osteophyte, which is typically located on the dorsal side of the nonunited scaphoid and can also be clearly recognized in CT imaging. It contributes to the humpback deformity.
Osteosclerotic processes with eburnation along the nonunion cleft can be visualized equally well with conventional radiography and CT (Figs. 20.4c, 20.5c ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree