19 Fractures of the Scaphoid
Fractures of the scaphoid are often not detected radio-graphically on the day of the accident and, therefore, requires particularly meticulous diagnosic attention. It appears justified to limit radiographic views to the dorsopalmar, lateral, and Stecher’s views if complementary examinations with high-resolution CT and MRI are available. Fractures of the scaphoid can be confirmed or excluded on the day of the accident with cross-sectional imaging. Fracture morphology with possible dislocation of fragments or comminuted areas is best visualized in high-resolution CT performed parallel to the longitudinal axis of the scaphoid. The assessment of fragment stability and the indication for surgical stabilization can best be made on the basis of CT findings. MRI has the highest sensitivity in revealing traumatic marrow edema. A scaphoid fracture, otherwise than the “bone bruise,” can be diagnosed only if MRI unmistakably reveals a fracture line. Three-phase scintigraphy is justified only if there is a special indication, such as repeated scaphoid injury.
Pathophysiology and Clinical Symptoms
A fracture of the scaphoid is generally caused by a fall on the hyperextended hand. This causes compression of the bone along a force vector extending from metacarpal III over the capitate and scaphoid to the radius. With increasing extension in the wrist, the distal part of the scaphoid becomes increasingly vulnerable. The proximal region of the scaphoid remains in a comparatively safe position between the radius and the radioscaphocapitate ligament ( Fig. 19.1 ). This anatomical condition explains why, in addition to the dorsal extension, the direction of carpal abduction also influences the fracture mechanism. Inclination toward the radial side causes flexion of the scaphoid; ulnar inclination causes extension of the scaphoid (Chapter 12). Accordingly, a combination of radial inclination and dorsal extension leads primarily to fracture of the distal parts, and a combination of ulnar inclination and dorsal extension leads primarily to fracture of the proximal parts of the scaphoid.
The incidence rates of scaphoid to radius fractures are in the ratio of 1:10, and both can be fractured at the same time in rare cases. Fracture of the scaphoid is by far the most common at just under 80% of carpal fractures. Males and younger individuals, between 15 and 40 years of age, are primarily affected by scaphoid fractures, whereas radius fractures occur more often among those between 50 and 70 years of age.
Depending on the severity of the injury, scaphoid fractures can occur in isolation or in combination with other carpal fractures and dislocations. For systematic imaging analysis of the injured carpus, see the passage on force vectors of the “lesser arc” and “greater arc” in Chapter 22. As described, a scaphoid fracture caused by an injury along the “greater arc” can also involve fractures of the styloid process of the radius, the capitate, hamate, and the triquetrum, and the styloid process of the ulna. An injury along the “lesser arc” generally causes ruptures of the intrinsic ligaments. A characteristic combined injury is de Quervain’s transscapho-perilunate fracture-dislocation (see Fig. 22.7 ).

Location of Fracture | Incidence |
Proximal third of scaphoid | 15% |
Middle third (waist) of scaphoid | 60% |
Distal third of scaphoid | 15% |
Tubercle of scaphoid | 10% |
Types of scaphoid fractures are differentiated according to their location and incidence ( Table 19.1 ). Scaphoid fractures occur most frequently in the middle third (scaphoid waist). Avulsion fractures of the scaphoid tubercle, which are extra-articular, are relatively rare.
The localization of a scaphoid fracture is the decisive criterion in the prognosis of fracture healing and, therefore, for the choice of the therapeutic procedure. The pathoanatomical explanation is the particular arterial supply of the scaphoid:
The distal and middle parts of the scaphoid receive sufficient blood supply from the radial artery, which provides small vascular branches at the level of a bony ridge on the dorsum of the scaphoid.
There is no independent blood supply in the proximal part of the scaphoid, however. This region is supplied by “retrograde perfusion” from an intraosseous vascular network fed by arteries entering the distal part of the scaphoid (see Fig. 20.1 )
The proximal pole of the scaphoid is therefore a vascular terminal zone in which a fracture can cause a critical metabolic supply if the intraosseous blood vessels are interrupted. A proximal fracture of the scaphoid, in comparison with a fracture in the other scaphoid parts, therefore often leads to the development of nonunion, as well as avascular osteonecrosis due to a disturbance in the osseous and medullary viability of the proximal scaphoid fragments.
Several classifications of fractures of the scaphoid exist. From a clinical point of view, Herbert and Fisher’s classification of 1984, which deduces therapeutic consequences from criteria of stability, has proved suitable ( Fig. 19.2 ). This classification differentiates acute fractures, stable forms (type A) and unstable forms (type B). Early recognition of unstable scaphoid fractures is of particular importance because these can develop into nonunions in up to 50% of cases. This classification further differentiates acute scaphoid fractures from delayed fracture healing (type C) and scaphoid nonunion (type D). Table 19.2 lists the acute fractures of the scaphoid according to the modified Herbert classification.
Symptoms of scaphoid fractures are pressure pain over the anatomic snuff-box (tabatière), pain on axial compression of the thumb, and painful restriction of mobility in extension and radial inclination of the wrist. Tenderness and pain often subside even if the fracture is mistaken for a sprain. It is important to remember that the diagnosis of a sprained wrist or contusion can only be a diagnosis by exclusion, i.e., after a fracture or traumatic lesion of a ligament has been definitely ruled out.

Table 19.3 summarizes the possible complications of scaphoid fractures. These will be explained in the later section.
Special Considerations in Childhood
Fractures of the scaphoid in childhood are relatively rare. They represent not quite 3% of all fractures of the hand in individuals under 15 years of age and are even rarer among children under 10 years of age. They occur primarily in the distal third of the scaphoid and on the extra-articularly localized scaphoid tubercle. Further diagnostic examinations in children should be performed with MRI.
Diagnostic Imaging
Diagnostic Radiography
Conventional projection radiography always constitutes the fundamental diagnostic technique in an injured wrist, and thus of the scaphoid. Images are acquired by using a small focus (0.6 mm−0.1 mm) and film-screen combinations with a sensitivity of 100 or 200 or with a digital system of at least 2K matrix size. When clinical examination suggests a scaphoid fracture, in addition to radiographs of the wrist in the neutral position in two planes, special views are taken to optimize visualization ( Fig. 19.3 ). There are two approaches to the diagnosis, as depicted in Table 19.4 .

Traditional radiographic diagnosis of scaphoid fractures calls for, in addition to the dorsopalmar and lateral views, the four views of the so-called scaphoid quartet series: Stecher’s view (closed fist and ulnar inclination), Schreck’s view (quill-holding position), and Bridgeman’s view (hand in slight extension), as well as a hyperpronation view (Chapter 1). The anatomic foundation of these dedicated views is the double-oblique tilt of the scaphoid with regard to the orthogonal planes. With these special views the attempt is made to position the scaphoid with its longitudinal axis parallel to the film plane and thereby to obtain a view of the entire length of the scaphoid ( Fig. 19.4 ). The scaphoid quartet series can also be acquired with Ahlbäck’s method by centering the x-ray tube on the carpus, which is constantly positioned in 10° extension. The tube is then angled in the following four positions: 25° ulnarly, 20° radially, 10° distally, and 10° proximally.
In a modified approach, conventional radiographs are limited to three views and, if a fracture is suspected, complemented immediately by a high-resolution CT examination. Projection radiography consists only of dorsopalmar, lateral and Stecher’s views. This approach omits repeated diagnostic examinations 10- 14 days later, as well as radioisotope bone scanning in the presence of characteristic clinical symptoms and unremarkable radiographic results, since even nondislocated fractures can be recognized early with thin-slice CT imaging. This requires 0.5 mm to maximally 1.0 mm thick, oblique-sagittal scans aligned parallel to the longitudinal axis of the scaphoid (Chapter 8).
Conventional Approach | Modified Approach | |
Primary diagnostics | Wrist in two orthogonal views | Wrist in two orthogonal views |
Stecher’s view | Stecher’s view | |
Further diagnostic measures | ||
1Three days after the accident; | ||
2after 10–14 days; | ||
3as early as possible. |
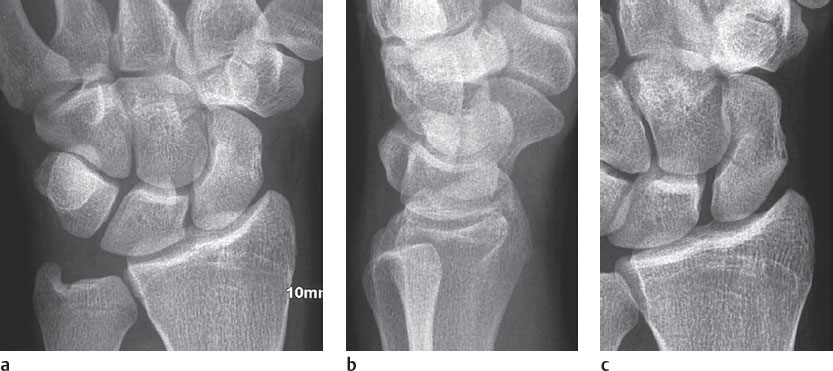
As with other fractures, the classical fracture criteria also apply to the scaphoid. Because the scaphoid is small and because of its unique oblique orientation, fracture signs are usually very discret and can be identified only as an infraction or fissure ( Fig. 19.4 ). Fractures are described as transverse, horizontal, or vertical in relation to the longitudinal axis of the scaphoid ( Fig. 19.5 ). A characteristic form of dislocated scaphoid fracture is the so-called “humpback” deformity, in which the proximal fragment is rotated in extension and the distal fragment is rotated in the opposite direction in flexion (“humpback flexion deformity”). This is caused by the tendency of the lunate to rotate dorsally, thereby pulling the proximal scaphoid fragment dorsally also if the scapholunate ligament is intact. Another reason is the axial force of the remaining carpus, which presses the distal scaphoid fragment toward the palm. The “humpback” deformity of the scaphoid can only be recognized and quantified in the lateral radiograph of the wrist. Table 19.5 lists radiographic signs of an acute fracture of the scaphoid, which also apply to CT imaging.
The so-called scaphoid fat-stripe sign serves as an indirect fracture criterion. The scaphoid fatty stripe is a radiolucent band of about 1 mm width between the collateral radiocarpal ligament and the tendon of the extensor pollics brevis muscle. In low-kilovoltage exposures of the dorsopalmar and quill-holding views, it appears as a transparent, convexly arching margin immediately adjacent the scaphoid. Fractures of the scaphoid or the styloid process of the radius (rare even in a fracture of the base of metacarpal I) result in parossal hematoma, which straightens the fatty stripe and displaces it laterally or even obliterates it. The fat-stripe sign is said to be present in over 90% of fractures of the scaphoid.
The decisive criterion for therapy is radiographic proof of fragment stability, since only stable fractures of the scaphoid should be treated conservatively by immobilization in a cast. Unstable scaphoid fractures should receive primary osteosynthesis to avoid long immobilization in a cast and the accompanying risk of developing nonunion. The criteria for scaphoid stability are summarized in Table 19.6 .

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree