
Diagnosis: Pneumocystis pneumonia
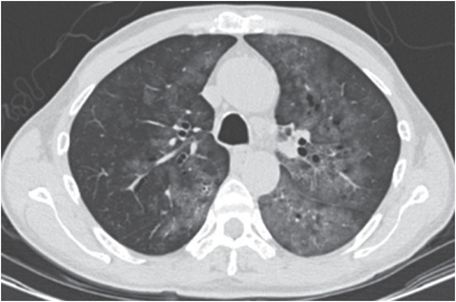
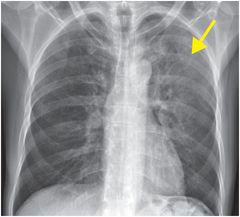
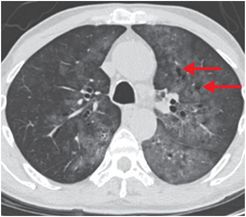
PA chest radiograph demonstrates diffuse ground glass opacification (GGO) in the left upper lobe (yellow arrow). Axial CT images demonstrate bilateral perihilar GGO with mild bronchiectasis and cystic changes in the left upper lobe (red arrows).

Discussion
Pneumocystis jirovecii pneumonia (PJP), or pneumocystosis, is a type of pneumonia that is prevalent in immunocompromised individuals.
The causal organism is the yeast-like fungus (previously erroneously classified as a protozoan) Pneumocystis jirovecii.
Histologically, there is thickening of the interstitium and fibrous tissue of the lungs, including the alveolar septa and alveoli, which lead to compromise of gas exchange.
PJP is characterized clinically by fever, dyspnea, hypoxemia, and productive cough.
Spontaneous pneumothorax can occur. Infection may involve extra-pulmonary sites such as liver, spleen, and skin.
The risk of infection increases when CD4 count decreases below 200 cells/mL. Serum lactate dehydrogenase levels may be elevated and PaO2 lower than expected for a given degree of dyspnea.
Chest radiography is the primary imaging modality in patients in whom pneumonia is suspected, including the immunocompromised. CT may be needed for further refinement of diagnosis.
Bilateral symmetric or asymmetric perihilar GGO on both chest x-ray and CT is typical.
Cavitation in the form of pneumatoceles without lobar predilection can be seen; with treatment, this finding resolves within 6 months.
Pneumothorax is seen in 13% of patients.
Lymphadenopathy, pleural effusions, and pulmonary nodules are associated findings.
Clinical synopsis
The patient was found to be HIV positive, and his clinical condition improved with trimethoprim-sulfamethoxazole.
Self-assessment
|
|
|
|
|
|
|
|
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








