

Diagnosis: Paraesophageal foreign body (metallic bristle from grill brush)
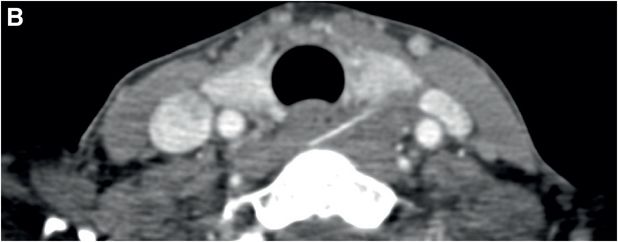
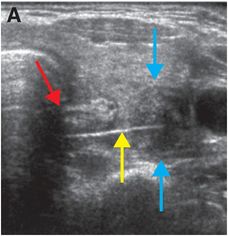
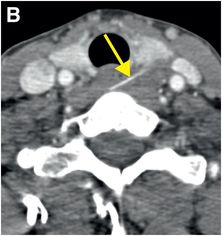
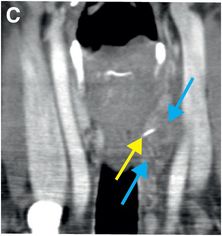
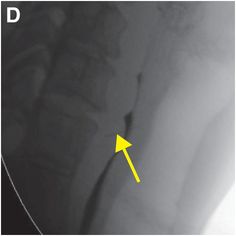
Transverse grayscale ultrasound image (A) demonstrates a linear echogenic structure (yellow arrow) posterior to the thyroid gland and traversing the esophagus (red arrow). The tip of the structure is located in a hypoechoic collection (blue arrows) adjacent to the left common carotid artery. Axial (B) and coronal (C) enhanced CT images demonstrate a linear metallic-density structure (yellow arrows) embedded in the cervical esophagus and penetrating the left lobe of the thyroid, with the tip located in an ill-defined mixed-attenuation collection (blue arrow). A single lateral image from an esophagram (D) with water-soluble contrast demonstrates the linear metallic object (yellow arrow) projecting over the esophagus, with no evidence of esophageal leak.
Discussion
Overview of oropharyngeal foreign bodies
The tonsils, base of tongue, valleculae and piriform sinuses are common locations for swallowed foreign bodies to lodge, with 50% of oropharyngeal foreign bodies lodged in either the tonsils or base of tongue.
Patients may present with dysphagia, odynophagia, sensation of foreign body, dysphonia, coughing, stridor, or hoarseness. Patients may be able to localize sharp foreign bodies above the level of the cricopharyngeus muscle better than those below it.
Children may present with refusal to feed, drooling, or dysphonia.
Treatment of oropharyngeal foreign bodies
Oropharyngeal foreign bodies usually require emergent removal.
The standard of care in non-asphyxiating foreign body aspiration (passage beyond the vocal folds) is diagnostic fiberoptic bronchoscopy. If that is unsuccessful, surgery is necessary.
Imaging of oropharyngeal foreign bodies
Plain films are limited in making the diagnosis of pharyngoesophageal and tracheobronchial foreign body aspiration, as only radiopaque foreign bodies can be clearly identified.
Foreign bodies made of wood and some plastics as well as many food items may be radiolucent. Additionally, if the foreign body is made of clear plastic, it may also be missed on direct laryngoscopy. Because of these two problems, the diagnosis of aspirated clear plastic items may be significantly delayed.
Foreign body aspiration is much more common in children than adults. In children, about 90% of aspirated foreign bodies are radiolucent on radiography. Of children who have a known aspirated foreign body, the chest x-ray may be normal in up to 30% of cases. In children with negative CXR and suspected foreign body aspiration, virtual bronchoscopy shows diagnostic promise with high sensitivity. If CT bronchoscopy is negative, children may be able to avoid rigid bronchoscopy. Virtual bronchoscopy has the added advantages of being able to visualize changes in the lung parenchyma, and potentially to offer an alternative diagnosis if no aspirated foreign body is seen.
Clinical synopsis
The patient recalled eating a meal of grilled steak tips the prior weekend, which immediately preceded her discomfort. Prior to cooking the meat, the grill had been cleaned with a metallic brush. Because this foreign body was felt to be in the paraesophageal soft tissues rather than the airway, the patient was taken for open (rather than endoscopic) surgical removal of foreign body. A grill brush bristle was removed after it was dissected from adjacent granulation tissue and phlegmon (the collection seen on imaging). The patient recovered well, with rare residual odynophagia and no swallowing dysfunction.
Self-assessment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








